Dialysis patients are a risk group for SARS-CoV2 infection and possibly further complications, but we have little information. The aim of this paper is to describe the experience of the first month of the SARS-Cov2 pandemic in a hospital haemodialysis (HD) unit serving the district of Madrid with the second highest incidence of COVID19 (almost 1000 patients in 100,000 h). In the form of a diary, we present the actions undertaken, the incidence of COVID19 in patients and health staff, some clinical characteristics and the results of screening all the patients in the unit.
We started with 90 patients on HD: 37 (41.1%) had COVID19, of whom 17 (45.9%) were diagnosed through symptoms detected in triage or during the session, and 15 (40.5%) through subsequent screening of those who, until that time, had not undergone SARS-CoV2 PCR testing. Fever was the most frequent symptom, 50% had lymphopenia and 18.4% <95% O2 saturation. Sixteen (43.2%) patients required hospital admission and 6 (16.2%) died. We found a cluster of infection per shift and also among those using public transport. In terms of staff, of the 44 people involved, 15 (34%) had compatible symptoms, 4 (9%) were confirmed as SARS-Cov2 PCR cases by occupational health, 9 (20%) required some period of sick leave, temporary disability to work (ILT), and 5 were considered likely cases.
ConclusionsWe detected a high prevalence of COVID19 with a high percentage detected by screening; hence the need for proactive diagnosis to stop the pandemic. Most cases are managed as outpatients, however severe symptoms are also appearing and mortality to date is 16.2%. In terms of staff, 20% have required sick leave in relation to COVID19.
Los pacientes en diálisis son un grupo de riesgo de sufrir la infección por el SARS-CoV2 y posiblemente de tener más complicaciones, pero la información con la que contamos es escasa. El objetivo de este trabajo es describir la experiencia del primer mes de pandemia por SARS-Cov2 en una unidad hospitalaria de hemodiálisis (HD) que atiende al 2º distrito madrileño con más en incidencia de COVID19 (casi 1000 pacientes en 100,000 h). Se presenta mediante un diario las acciones llevadas a cabo, la incidencia de COVID19 en pacientes y en el personal sanitario, algunas características clínicas y el resultado de un cribado entre todos los pacientes de la unidad.
Al inicio, teníamos 90 pacientes en HD: 37(41,1%) han tenido COVID19, de los que 17 (45,9%) fueron diagnosticados por síntomas detectados en el triaje o durante la sesión y 15 (40,5%) en un cribado realizado a posteriori en los que no se había hecho test diagnóstico por PCR-SARS-Cov2 hasta ese momento. El síntoma más frecuente fue la fiebre, el 50% presentó linfopenia y el 18,4% saturación de O2 <95%. Precisaron ingreso hospitalario 16(43,2%) y 6 fallecieron (16,2%). Encontramos un agrupamiento de contagio por turnos y también en aquellos que usaban transporte colectivo. En cuanto al personal, de las 44 personas involucradas, 15 (34%) presentaron sintomatología compatible y 4 (9%) tuvieron PCR SARS-Cov-2 positiva determinada por Salud Laboral y 9 (20%) precisaron algún periodo de Incapacidad Laboral Transitoria (ILT), y 5 fueron considerados casos probables.
ConclusionesDetectamos una elevada prevalencia de COVID19 con un elevado porcentaje detectado por cribado y por tanto la necesidad de ser proactivos en el diagnóstico para detener la pandemia. La mayoría están siendo manejados de forma ambulatoria, aunque también aparecen cuadros graves y la mortalidad hasta ahora es del 16,2%. En cuanto al personal un 20% ha precisado ILT en relación con COVID19.
Dialysis patients may have impaired immunity, so they constitute a group at risk of suffering SARS-CoV-2 infection and possibly with a high rate of complications. Furthermore, they have relevant epidemiological connotations: they visit a medical center regularly (2–6 times per week), with more than 4 h per day exposed to possible contagion and the majority use collective sanitary transport. Once infected they are itinerant sources of new infections within this risk group. Thus, it can be stated that a Dialysis unit is a place that deserve special consideration in relation with the epidemiology of Covid -19.
On February 26 we had the first case confirmed of COVID-19 in the Community of Madrid, on the 28th there were 5 cases and on March 3rd, 56, 5 of them were severe cases. The first case diagnosed in our hospital occurred on March 4, and on March 5 it was created a group dedicated to coordination the work. At that time, the specific information on kidney patients or in dialysis units was scarce. There was a publication from the area of Wuhan (China)1 describing cases from a dialysis unit with 230 patients and 33 staff; later on, this information was reported as a letter to the editor.2 There were a series of recommendations published by the ASN3 and subsequently by EDTA, SEN4 and other authors.5
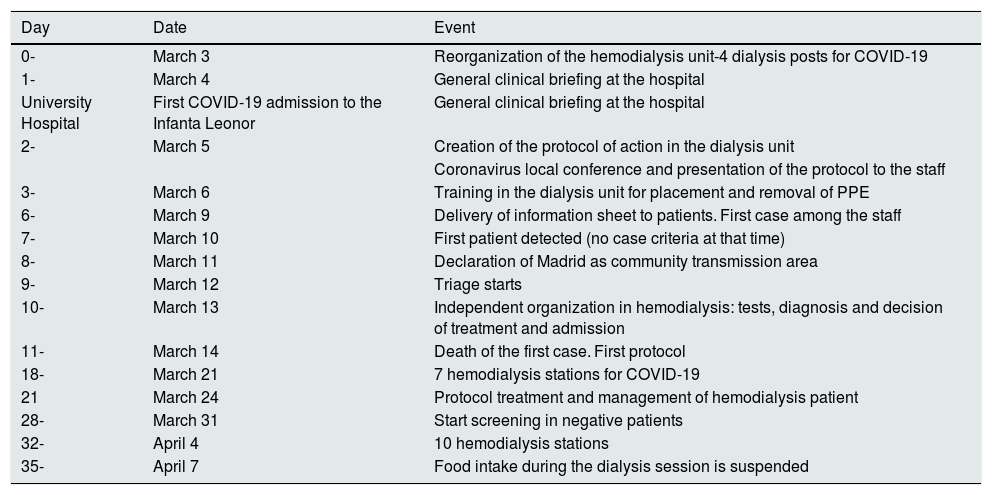
Our objective is to collect the experience of the first month of the SARS-CoV-2 pandemic in a hospital based HD unit in Madrid. For us is fundamental to highlight the high prevalence of asymptomatic patients detected in a PCR-SARS-CoV-2 screening study. Initially, there was a significant nervousness and uncertainty, we organized ourselves according to our criteria, and it was possible to carry out an epidemiological study in our entire HD unit which has allowed the detection of asymptomatic patients and therefore prevent, to a certain degree, the spreading of the infection in our medium. Will present the general data, initial measures, implementation of a protocol, description and evolution of cases and the result of the epidemiological study.nFinally, we will make a brief discussion and reflections based on our findings. The chronological evolution is collected in Table 1.
Chronological evolution of events.
| Day | Date | Event |
|---|---|---|
| 0- | March 3 | Reorganization of the hemodialysis unit-4 dialysis posts for COVID-19 |
| 1- | March 4 | General clinical briefing at the hospital |
| University Hospital | First COVID-19 admission to the Infanta Leonor | General clinical briefing at the hospital |
| 2- | March 5 | Creation of the protocol of action in the dialysis unit |
| Coronavirus local conference and presentation of the protocol to the staff | ||
| 3- | March 6 | Training in the dialysis unit for placement and removal of PPE |
| 6- | March 9 | Delivery of information sheet to patients. First case among the staff |
| 7- | March 10 | First patient detected (no case criteria at that time) |
| 8- | March 11 | Declaration of Madrid as community transmission area |
| 9- | March 12 | Triage starts |
| 10- | March 13 | Independent organization in hemodialysis: tests, diagnosis and decision of treatment and admission |
| 11- | March 14 | Death of the first case. First protocol |
| 18- | March 21 | 7 hemodialysis stations for COVID-19 |
| 21 | March 24 | Protocol treatment and management of hemodialysis patient |
| 28- | March 31 | Start screening in negative patients |
| 32- | April 4 | 10 hemodialysis stations |
| 35- | April 7 | Food intake during the dialysis session is suspended |
Infanta Leonor University Hospital serves the Vallecas district of Madrid which is the 2nd district with the highest accumulated incidence of Covid-19: 994.39 patients per 100,000 inhabitants (as of April 16, 2020).6 In our HD unit, which includes 90 patients, 37 (41.1%) have been diagnosed with COVID-19 (36 cases confirmed by positive PCR, and a probable case [without positive PCR]); 22 (59.5%) were symptomatic and 15 (40.5%) asymptomatic, which shows a high prevalence and highlights the importance to detect the cases to avoid their expansion, since it is not possible perform adequate isolation without identifying all cases. Among those affected, 16 have required hospital admissions and 6 died, representing 43.2% of hospitalization and 16.2% of mortality.
Hay incidence of cases have been found in the afternoon shifts that included 25 patients: 9 (24.3%) in M.W.F. and 11 (29.7%) in T.T.S. The morning shift of T.T.S. has been the least affected with only 4 cases, despite the fact that the first positive patient was detected in that shift.
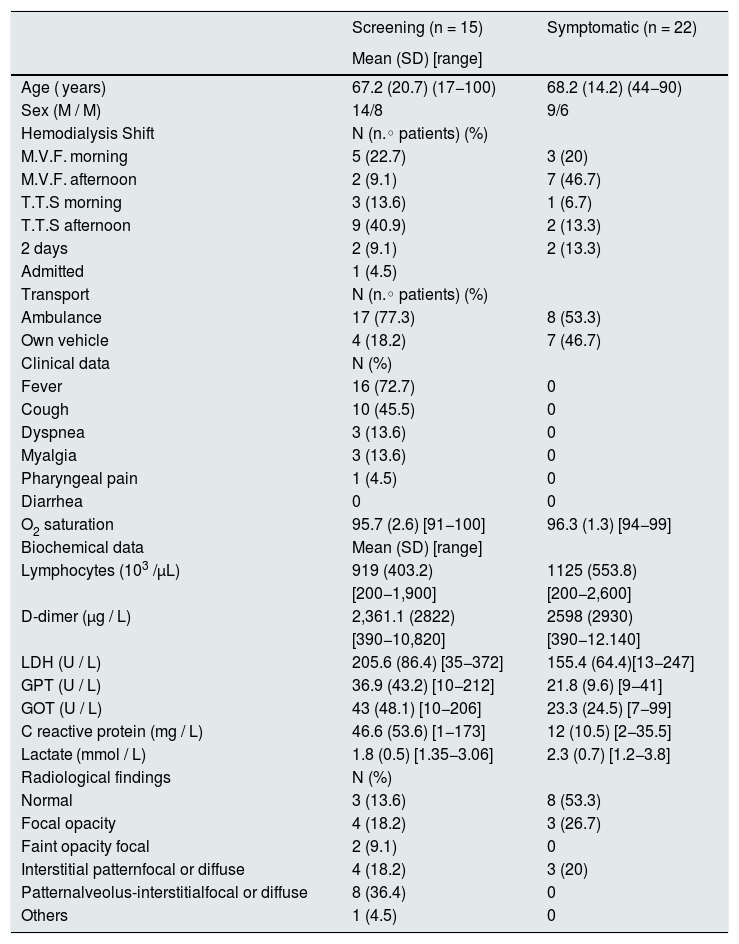
The majority of infected patients (n = 25; 67.6%) shared the transportation vehicle from home to the hospital and back. Between symptomatic and asymptomatic patients there were no difference in age, O2 saturation or biochemical data. However, there were differences in patterns of X-ray changes; in most asymptomatic patients X-ray was normal or with less severe radiological changes, which translates into differences in treatment.
Initial cases. Development of a protocol and organization of the hemodialysis unit from day 0With the initial case and the progressive increase of affected patients, on day 3 of March (day 0) the staff have a conference meeting to organize the referral of patients to a peripheral HD unit and modify shifts in order to maximize the number of stations available in the hospital unit. The number of active patients was reduced from 95 to 90.
Based on a previous document made for influenza A, a protocol was drafted and completed day 5 of March (day 2) and was forwarded to the Executive Administrator, preventive medicine service and the hospital COVID-19 coordinating group.
The protocol included:
- 1)
Information directed to patients about infection, prevention and measures to be taken when symptoms appear (Annex 1 of the additional material).
- 2)
Basic management of hemodialysis patients: creation of a triage; physical separation of patients infected / suspicious; and staff ; structure and organization of staff and resources (appendix 2 to additional material)
The transport by collective ambulance was discouraged, promoting transport in own vehicle.
On March 9 (day 6) patients received the information sheet and this same day we had the first COVID-19 sick leave from the staff (a doctor). On March 10 (day 7) it is detected the first confirmed case of SARS-CoV-2 in a hemodialysis patient. On March 11 (day 8) Madrid was declared a SARS-CoV-2 transmission community. March 12 (day 9) the triage was started.
The triage is carried out in the outpatient consultation room that is closest to the patients waiting room where patients are asked to seat
separated by two empty chairs. The triage is performed as they enter the room to avoid accumulation of patients in the waiting room. This triage was initially performed by a doctor and the help of a nurse and and an auxiliary assistant; currently it is performed by the nurse and the assistant, the doctor is consulted if there is a question about a possible infection. The patients are requested to wash their hands and the arm with the fistula before leaving home and all patients must wear a surgical mask since hospital arrival. In the same triage the patients have hand hygiene with hydroalcoholic solution. On a sheet (Annex 3 of the additional material) the following information is recorded: temperature, suspicious symptoms, affected relatives and type of transport used (own vehicle or collective ambulance). If there is no suspicion, the patient goes to the dialysis room where they are accommodated according to order of entry and always maintaining a separation of at least 2 m waiting until the session is started. If during session there is fever, dyspnea or any other clinical suspicion symptom in a patient that was considered negative, then the patient is dialyzed by a nurse with the individual protection equipment (PPE) or the patient is moved to the COVID-19 area. As an additional protective measure on April 7, (day 35) the food intake during the session was not allowed. In the case of suspicion in the triage, the patient is conducted to the area reserved for patients with COVID-19 and a number of measures are taken that are described below.
From March 15th and with the aim of avoiding sanctions for violation of confinement, letter / certificate was given to drivers, specifying the name of the patient without specifying the shift in anticipation of possible changes.
The protective equipment that has been used in triage and in the care of non-suspicious patients consist in surgical mask and gloves. From April 6th (day 34), after becoming aware of the high prevalence of asymptomatic positive patients in the epidemiological study, the protection equipment was changed to disposable gown, glasses or face mask and FFP2 mask for triage, connection and disconnection. For COVID -19 negative patients, the proportion of staff in the hemodialysis room was one nurse for every 4 patients and an auxiliary assistant for every 8 patients.
- a
Organization of the COVID-19 hemodialysis area
In our hemodialysis unit there is separate area with 7 dialysis positions in independent rooms that were reserved for Covid -19 patients
(this area was intended for HCV patients). It was started with 4 hemodialysis monitors and it was necessary to increase to 7 monitors on March 21 (day 18); and to 10 monitors from day 32. The last 3 monitors had to be located in the common hemodialysis room separated by nat least 2 m between them and with screens and more than 3 m from the rest of patients.
From the beginning there were two shifts of dialysis with positive outpatients and leaving 1–2 places empty for possible additional positive patients that cold be detected in the triage. If no new cases appeared in the triage, the positions were filled with patients admitted with COVID-19 who attended the scheduled day in the morning or afternoon shift depending on the clinical situation and the position available. Thus, based on initial planning, there has been a constant variation in the number of patients requiring daily adjustment in each shift to adjust to the continuous change in the number of patients.
Regarding protection measures in the area of positives / suspects COVID-19 patients, a distinction is made between the personnel with a direct action with patients and the "mirror" personnel who is in charge of facilitating the material, medical history management, medication preparation, etc. The PPE of direct action personnel includes : resistant surgical gown, waterproof apron, hat, leggings, FFP2 mask, double glove (a long one over the gown and a short one ), and glasses or facial mask, with a protocol for putting and removing PPE to avoid contaminationnwhich includes changing gloves between patients with hydroalcoholic solution hygiene before and after the change. In this area the proportion of personnel was modified to facilitate the care and decrease the risk of contamination: one direct care nurse every 3–4 patients, one «mirror» nurse every 6–8 patients and one assistant every 5–7 patients, who also have «mirror» functions. The variability of the proportion of personnel in this area is due to the necessary adaptation depending on the number of patients.
Due to the shortage of PPE, especially at the beginning of the pandemic, the professionals use the same PPE during the entire dialysis shift, except for changing gloves and hand hygiene between patients sessions and patient, and change of gown / apron / glasses if any fluid splashes occurred. During the first week of April the PPE supply improved, so if needed, in the middle of the shift the personnel switched from direct attention to the mirror and vice versa. Due to its scarcity, the FFP2 mask had to be used for several shifts (2 or 3), up to a maximum of 8 h of continued use and as long as it was not damaged or visibly contaminated; in addition, in all cases it surgical mask is used on top of the FFP2 with a double purpose: to protect the FFP2 from external contamination and avoid the transmission of drops by the professional if the FFP2 has a filter.
- b
Management of the patient under suspicion and diagnosis
During the initial days, in case of clinical suspicion of contagion, after completion of the dialysis the patients was transferred to the emergency room to be evaluated by internal medicine for o assessment and diagnosis. After March 13 (day 10), emergency service was collapsed and patients were entirely managed by Nephrology for diagnosis, admission and treatment.
In the event of clinical suspicion, we followed the algorithm presented in annex 4 of the additional material:
- -
Urgent lab work was requested : blood count, D-dimer, biochemistry including: GOT, GPT, LDH, lactate, C-reactive protein (PCR).
- -
Nasopharyngeal exudate for SARS-CoV-2 PCR, which was performed using VIASURE SARS-CoV-2 Real Time PCR Detection Kit
- -
Chest X-ray.
Any patient with suspicion is handled as if he was positive. If the PCR was positive, it is a confirmed case and continues dialysis as COVID-19; and if the result is negative the patient is reevaluated:
- -
If clinical suspicion based on analysis, clinical evolution and radiology is low, it was considered negative.
- -
If the diagnosis of clinical suspicion is high, it was considered a probable case, it continues to be handled as if it were positive and SARS-CoV-2 PCR is repeated. If it turns to be negative and after ruling out other possible diagnoses, clinical judgment prevails: it is considered as a probable case being managed as COVID-19 positive.
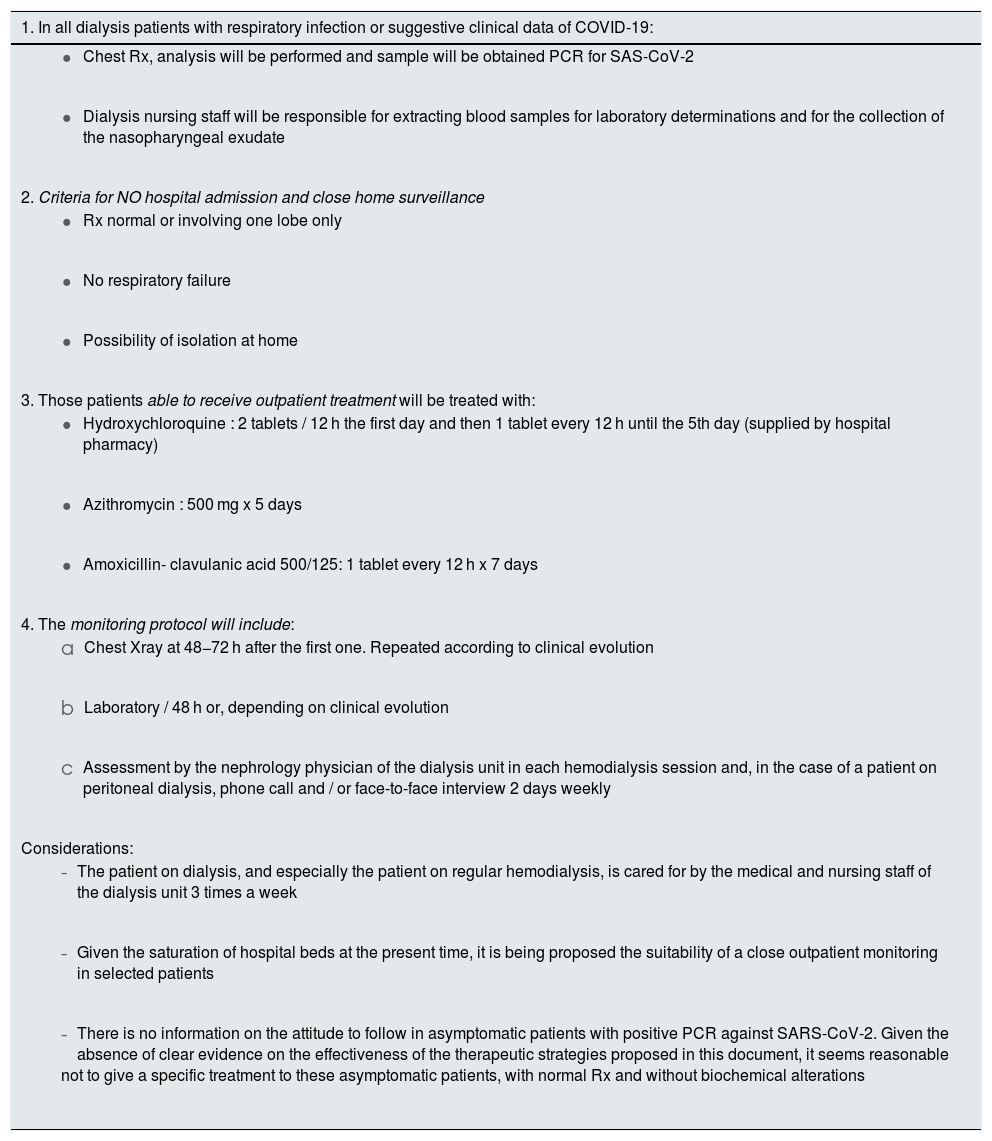
Different management protocols were created in the hospital. The first of them with criteria of admission and treatment is from March 14 (day 11). At the beginning of the pandemic, treatment included lopinavir / ritonavir ( Kaletra ®) and hydroxychloroquine ( Dolquine ®) and at the time of the present communication the recommended drugs are hydroxychloroquine and azithromycin depending on the duration of clinical symptoms, and in the last week (day 34) it has been advised an increase in the dose of anticoagulants. One more specific protocol was developed on March 24 (day 21), on how to handle COVID-19 hemodialysis patients with criteria of admission and need for treatment, a protocol based on the hospital protocol and one from the Ministry of Health7; such a protocol was changed and adapted, since up to now there is no evidence on the efficacy of any specific treatment in the general population and there is even less evidence in the dialysis population (Table 2). In COVID-19 patients in whom it is decided follow-up as outpatient, the tests are repeated at the discretion of the responsible hemodialysis doctor. They were evaluated during the regular hemodialysis sessions and by phone calls the days that do not come for dialysis. Depending on the evolution, the possibility of admission would be reconsidered, meanwhile the patient is followed with analytical and radiological parameters weekly. When symptoms disappears and / or the complementary data are normal the nasopharyngeal exudate is repeated. If negative, during the following 14 days the patient continues in isolation at home and in the COVID-19 area of the dialysis unit. If it is positive, it is repeated weekly.
Criteria for managing of a patient on hemodialysis with a diagnosis of COVID-19, performed according to the recommendations of the Ministry of Health and the Infanta Leonor University Hospital.
| 1. In all dialysis patients with respiratory infection or suggestive clinical data of COVID-19: |
|---|
|
|
| 2. Criteria for NO hospital admission and close home surveillance |
|
|
|
| 3. Those patients able to receive outpatient treatment will be treated with: |
|
|
|
| 4. The monitoring protocol will include: |
|
|
|
| Considerations: |
|
|
|
It should be added that at the time of diagnosis, all those patients who can be discharged home are asked whether they can comply with measures of isolation. If that is the case they are given written instructions on how to do it and they are given surgical masks and gloves to improve home isolation when living with others.
One doctor takes care of the outpatients during the morning and another doctor during the afternoon. A third doctor is in charge of admissions and consultations helping other doctors who attend COVID-19 patients in the hospital.
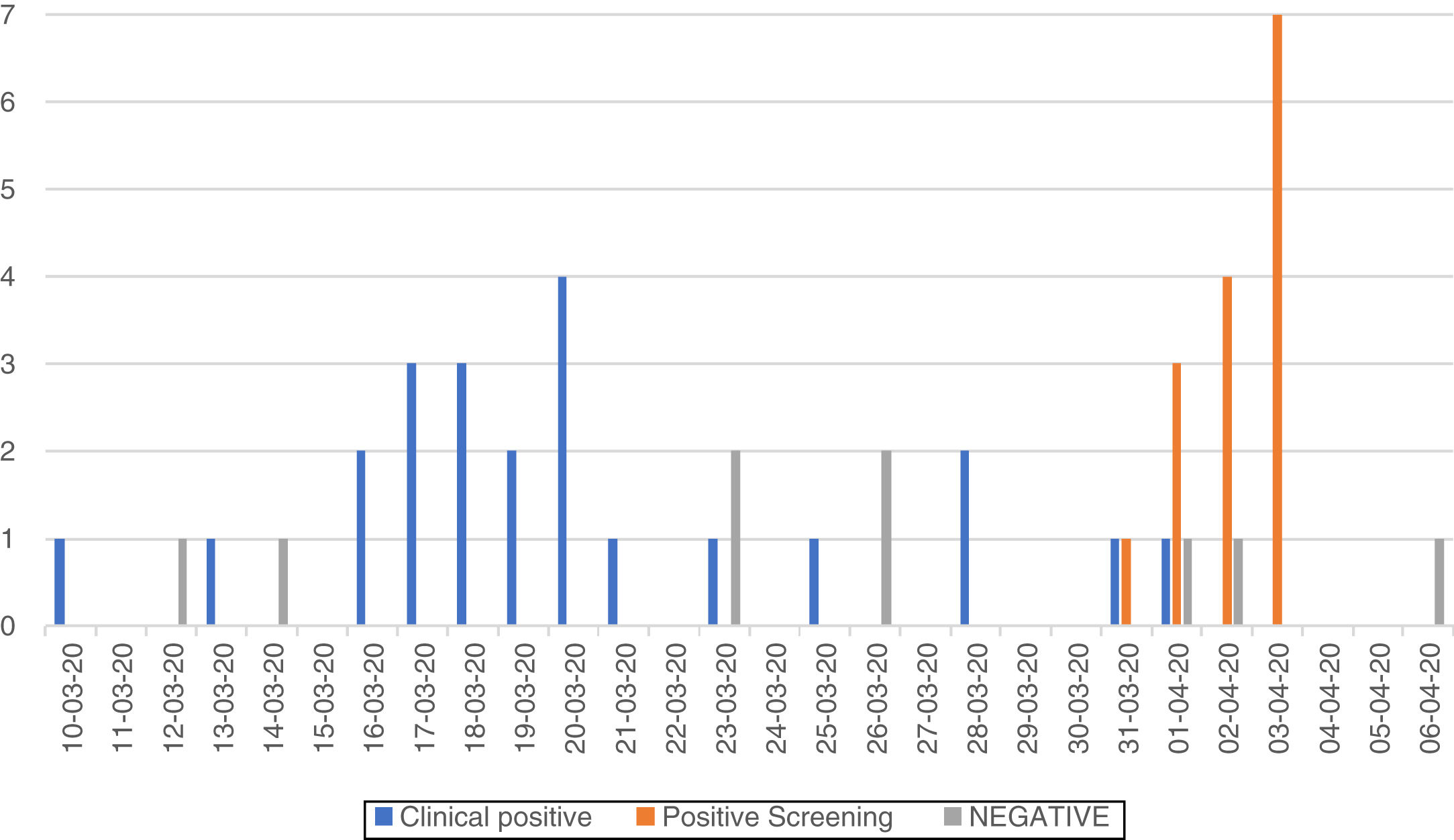
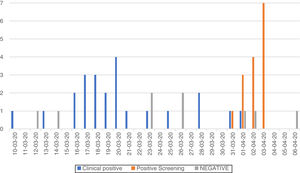
Description of symptomatic casesFrom March 10 to April 8, there were 37 PCR-SARS-CoV-2 analysis performed in 31 patients. The initial test was performed because clinical suspicion, although in 5 patients the test was repeated (in one 3 times) when negative but with clinical, biochemical data or radiological findings suggestive of Covid -19. In 2 of these patients ended up being positive and 3 negative. A total of 21 patients were PCR-SARS-CoV-2 positive. Also, there was a patient with negative SARS-CoV-2 PCR, but with clinical compatible of infection that was considered a probable case of COVID-19. Therefore the total number of COVID-19 patients with symptoms (confirmed microbiologically or not) were 22 (24% of the total number of patients being dialyzed in the Unit). Fig. 1 shows the cases detected every day.
Epidemiological characteristics, symptoms, lab results and radiological images are shown in Table 2. Lymphopenia was present in 11 patients (50%), saturation of O2 <95% in 4 patients. Out of the 21 patients, 9 (43%) were admitted to the hospital at the time of diagnosis, 6 due to clinical situation (insufficiency respiratory or radiological involvement) and 3 for epidemiological reasons (adequate isolation could not be performed as an outpatient basis). One patient was diagnosed of Covid-19 during hospital admission for another reason. Currently 3 patients remain still admitted (one of them for epidemiological reasons); 6 patients died and the rest have been discharged or continue outpatient treatment. Median period of admission in days has been 14 (6–20) days for patients that were finally discharged and 92–12 days for deceased patients. The admission period has been longer in those admitted for epidemiological reasons, 17 and 20 days, with PCR SARS- Positive CoV-2 and minimal clinical, biochemical and radiological involvement.
Regarding treatment, as mentioned before, the drugs and decisions have been changing rapidly.
Six patients (27.3%) were treated with hydroxychloroquine, 6 (27.3%) with lopinavir / ritonavir + hydroxychloroquine, 8 (36.4%) with azithromycin + hydroxychloroquine, 1 (4.5%) with azithromycin + hydroxychloroquine + amoxicillin / clavulanate and one patient refused to be treated.
The 6 deceased patients as compared with those discharged or hospitalized admitted, were older 80.6 (15.3) vs. 62.2 (20.6) years (p < 0.04) (Table 3). A 77.3% of patients with symptoms came to the hospitalin collective transport. In fact, the turn of T-T-S afternoon with the highest proportion of Covid 19 patients and the 11 patients were transported collectively by ambulance.
General data of patients COVID-19 diagnosed by clinical symptoms or detected by screening.
| Screening (n = 15) | Symptomatic (n = 22) | |
|---|---|---|
| Mean (SD) [range] | ||
| Age ( years) | 67.2 (20.7) (17−100) | 68.2 (14.2) (44−90) |
| Sex (M / M) | 14/8 | 9/6 |
| Hemodialysis Shift | N (n.◦ patients) (%) | |
| M.V.F. morning | 5 (22.7) | 3 (20) |
| M.V.F. afternoon | 2 (9.1) | 7 (46.7) |
| T.T.S morning | 3 (13.6) | 1 (6.7) |
| T.T.S afternoon | 9 (40.9) | 2 (13.3) |
| 2 days | 2 (9.1) | 2 (13.3) |
| Admitted | 1 (4.5) | |
| Transport | N (n.◦ patients) (%) | |
| Ambulance | 17 (77.3) | 8 (53.3) |
| Own vehicle | 4 (18.2) | 7 (46.7) |
| Clinical data | N (%) | |
| Fever | 16 (72.7) | 0 |
| Cough | 10 (45.5) | 0 |
| Dyspnea | 3 (13.6) | 0 |
| Myalgia | 3 (13.6) | 0 |
| Pharyngeal pain | 1 (4.5) | 0 |
| Diarrhea | 0 | 0 |
| O2 saturation | 95.7 (2.6) [91−100] | 96.3 (1.3) [94−99] |
| Biochemical data | Mean (SD) [range] | |
| Lymphocytes (103 /µL) | 919 (403.2) | 1125 (553.8) |
| [200−1,900] | [200−2,600] | |
| D-dimer (µg / L) | 2,361.1 (2822) | 2598 (2930) |
| [390−10,820] | [390−12.140] | |
| LDH (U / L) | 205.6 (86.4) [35−372] | 155.4 (64.4)[13−247] |
| GPT (U / L) | 36.9 (43.2) [10−212] | 21.8 (9.6) [9−41] |
| GOT (U / L) | 43 (48.1) [10−206] | 23.3 (24.5) [7−99] |
| C reactive protein (mg / L) | 46.6 (53.6) [1−173] | 12 (10.5) [2−35.5] |
| Lactate (mmol / L) | 1.8 (0.5) [1.35−3.06] | 2.3 (0.7) [1.2−3.8] |
| Radiological findings | N (%) | |
| Normal | 3 (13.6) | 8 (53.3) |
| Focal opacity | 4 (18.2) | 3 (26.7) |
| Faint opacity focal | 2 (9.1) | 0 |
| Interstitial patternfocal or diffuse | 4 (18.2) | 3 (20) |
| Patternalveolus-interstitialfocal or diffuse | 8 (36.4) | 0 |
| Others | 1 (4.5) | 0 |
The high incidence of infection in our area made us suspect that there were a high number of asymptomatic infected patients. Thus PCR-SARS-CoV-2 was performed to all patients who remained to be screened that were handled as negatives cases.
As of March 31 (day 28), 61 PCR were performed in 59 patients (2 tests were repeated because the results were not conclusive i). All nasopharyngeal exudates were performed at the time of triage, before entering the dialysis room and by the same nurse.
Fifteen patients (25.4% of the screening) were positive. If the result was positive, they were notified by telephone and were informed about the mandatory home isolation and avoid collective transportation to attend the hemodialysis session. All these patients were asymptomatic and no fever or other symptoms when they came to their scheduled session. In the first session, when already isolated, blood biochemistry and chest x-ray were requested. The administration of drugs was decided in individual bases. The results of the COVID-19 patients are shown in the Table 3. Lymphopenia was present in 46.7%, and only one with O2 saturation <95% required admission 2 days after screening and was discharged after 6 days. Regarding treatment, 6 were not treated, 8 have been treated with azithromycin + hydroxychloroquine and one patient has also received amoxicillin / clavulanic.
Staff of the hemodialysis unit. ReorganizationThe staff of the nephrology service includes 9 physicians; in the dialysis unit there are 22 nurses, 11 auxiliary staff and 2 for administrative work (one per shift). In the event of symptoms, the had to contact with the occupational risk prevention office to have a PCR performed. The results of the PCR (performed only on symptomatic patients) and temporary sick leave (TSL) have been:
- -
Administrative: one, positive PCR and TSL (50% of administrative).
- -
Physicians: 3, all negative PCR and one TSL (11.1% of the physicians).
- -
Nurses: 4, all negative PCR, 3 TSL (18.1% of nurses).
- -
Auxiliaries: 6, 3 with positive PCR, 4 TSL (36.3% of auxiliaries).
Only one of them required hospital admission for severe pneumonia. Thus, 9 (20.4%) of the staff were diagnosed of Covid-19 either by PCR or by clinical, biochemical data or radiological.
Preventive measures for protection of administrative staff were the placement of screen and separation of 1 m from the visitor as well as the general recommendations of prevention. Changes in PPE protection carried out by auxiliary and nursing staff have been explained already.
As for the medical staff, 3 of the doctors were assigned to atend COVID-19 patients in the general area of hospitalization. The rest of the doctors covered the dialysis unit, hospitalization and consultations, phone calls to patients with advanced chronic kidney disease (ACKD) and outpatients clinic, and they ordered the necessary laboratory controls.
Nursing has been devoted almost exclusively to treatment of hemodialysis patients, and phone follow-up of patients with ACKD, on peritoneal dialysis and home hemodialysis. Only one nurse remained in the short term hospital stay which was restricted to one day per week, to care for ACKD patients who require a close follow-up or for outpatient treatments that cannot be delayed.
Current situationAt the time of submission of the present manuscript we had 31 COVID-19 positive patients. The last death was on April 2 and the patients admitted or outpatients are in a stable situation. The same dynamics of triage, separation and prevention measures continue. All patients are followed with PCR-SARS-CoV-2. If the result is negative it was decided, together with preventive medicine, to maintain isolation at home and in the unit for 14 additional days as long as the clinical symptoms do not persist; although these measures could vary if other diagnostic tests were available.
Final comments and reflectionsThe main reason for this communication is to expose the day by day incidents in a homodialysis unit during the first weeks of the COVID-19 pandemic providing the information we consider relevant. At the present time, there are already published different recommendations,8–10 but here the reality is exposed of a unit that has had to go ahead, generating answers to the problems that arose every day.
The essential issue that we want to highlight is the high incidence of COVID-19 infection in our area, emphasizing that the 40% of those infected were asymptomatic and were detected by screening. This data forces to consider that it is necessary to pursue the diagnosis of all patients using PCR-SARS-CoV-2 alone or in combined with serologies. This measure is not indicated in the different protocols published during March and April, however we consider it is of great utility in order to prevent the spread of the virus as most of the patients have had contact with each other. In fact, we found a shift grouping of cases, and that the majority used community transport, which increases transmission between patients and reinforces the need screening, possibly with closer follow-up in those that share transportation. Taiwan experience11 advocates for being proactive in quickly diagnosing and isolating infected as it has been done in our hospital. Also the published Chinese experience advocates screening, but in its case they do it through chest CT9 and only more advanced diagnoses steps include PCR and serology. In our environment, such approach is not feasible, being easier and, from our point of view, more useful, the evaluation of exudate that determines who can spread the disease. Other points we want to comment are:
- 1
The incidence in our population is much higher than communicated in the Chinese or Italian groups12 that reported around 16%.
- 2
We have a high index of suspicion, so the presence of moderate fever or minimal symptoms is considered suspected case and PCR is performed. Among our patients we have not found gastrointestinal symptoms as reporteds in the Chinese series or by the SEN registry.13
- 3
Many of the infected patients did not require hospital admission, this is different from the SEN registry that shows a 81% of admissions of hemodialysis patients. WE did not have ICU admission. Only one of was considered for ICU admission because the age (65 years ), but finally was not admitted because significant cardiovascular pathology.
- 4
Our percentage of deaths is similar to that quoted in the aforementioned Wuhan article, although in our population all died from COVID-19, except one patient who had advanced lung cancer with a limited therapeutic effort due to the general deterioration.
- 5
We cannot make any claims about effectiveness of the various treatments, since there were different treatments applied and with different criteria. Although there are several protocols proposed,14 the effectiveness has not been demonstrated. Urgent reflection is the needed to have unified protocols to learn which treatment is the best.
- 6
Regarding the findings in the staff, we believe it is the first communication that addresses this aspect essential for the operation of the dialysis units in this moment, and that has caused a high number of TSL a short space of time. Most exudates performed were negative and the diagnosis was made based on the clinical symptoms, with the appearance even of pneumonias with PCR negative. It is impossible to ignore the need for personnel particularly the specialized hemodialysis nursing staff and it is important to consider how it would affect work performance having to isolate ourselves, although this fact must be put in the balance with the possibility that we are infected and, therefore, contributing to disease dissemination ; therefore, in our opinion, screening of staff with PCR or antibodies would be desirable. The fact that 20% of staff has had an TSL related to COVID-19 suggests that there may be asymptomatic carriers also spreading the virus.
First, it is necessary to diagnose symptomatic and asymptomatic patients and the sooner the better, by PCR and serology.
Second is that the situation requires great organizational flexibility that enables quick responses. It is essential to have cohesive staff motivated by the care of patients. That team is developing the present work.
Conflict of interestsNone.
Perez-Villar, MI, Romero R, Rodriguez-Suarez E, Ramos A, Liébana B, Vinagre G, Ruiz S., Herrera E, Quesada MT, Saenz AJ, Diaz de Argote P, Garcia-Martinez P, Bermejo MB, Sánchez-Fernandez N, Martinez-Gonzalez M, Cerrajero R, Bernabé M, Rojas V, Martínez-Dios I, Conejo D, Rodriguez-Presa P, Varona Y, Muñoz-Blazquez R, Sanz-Martinez D, Montoro JJ, Aviles AI.
Please cite this article as: Albalate M., Arribas P., Torres E., Cintra M., Alcázar R., Puerta M. et al. Alta prevalencia de COVID-19 asintomático en hemodiálisis. Aprendiendo día a día el primer mes de pandemia de COVID-19. Nefrologia. 2020;40:279–286.