Presentamos el caso clínico de un varón de 50 años de edad que consulta por presentar una enfermedad renal litiásica recidivante y una nefrocalcinosis. En la exploración clínica destacó una talla baja y un genu varo bilateral importante. Entre los datos bioquímicos se apreciaba una pérdida renal de fosfatos intensa con hipofosfatemia, una 25 OH vitamina D3 normal, una 1,25 OH2 vitamina D3 elevada y una hipercalciuria. La hormona paratiroidea (PTHi) se encontraba disminuida y en la ecografía renal se confirmó la existencia de una nefrocalcinosis bilateral grave, localizada en la médula renal. Además, se constató una insuficiencia renal crónica incipiente y una acidosis tubular renal incompleta, ambas secundarias a la nefrocalcinosis y no directamente relacionadas con la enfermedad basal. En el estudio molecular se encontró un cambio en homocigosis en el intrón 5 del gen SLC34A3 (NM_080877.2:c[448+5G>A]+[448+ 5G>A]). Sus tres hijos eran portadores de esta misma variante en heterocigosis y, aunque clínicamente estaban asintomáticos, dos de ellos tenían una hipercalciuria. Todos estos datos parecían indicar que el paciente presentaba un raquitismo hipofosfatémico hereditario con hipercalciuria (HHRH), secundario a una alteración en el cotransportador sodio-fosfato IIc (NaPi-IIc), localizado en el túbulo proximal. El HHRH se transmite de forma autosómica recesiva y es una forma muy rara de raquitismo hipofosfatémico. El diagnóstico y el tratamiento son fundamentales para evitar las secuelas óseas del raquitismo y la nefrocalcinosis. La distinción correcta con las otras formas de raquitismo hipofosfatémico tiene implicaciones en el tratamiento, ya que normalmente la administración aislada de suplementos de fósforo corrige todas las alteraciones clínicas y bioquímicas, excepto la pérdida de fosfato por la orina. El aporte exógeno de calcitriol, como se aconseja en otros raquitismos hipofosfatémicos, puede favorecer los depósitos renales de calcio y la aparición de nefrocalcinosis, así como empeorar su pronóstico.
We report a case of a male aged 50 years who consulted for renal disease recurrent lithiasis and nephrocalcinosis. The clinical examination showed external signs of rickets/osteomalacia and biochemical data as well as a severe loss of renal phosphate with hypophosphatemia, normal 25 OH vitamin D, high 1,25 OH vitamin D and hypercalciuria. Parathyroid hormone was low and renal ultrasound confirmed the existence of severe bilateral medullary nephrocalcinosis. They also found incipient chronic renal failure and incomplete renal tubular acidosis, both secondary to nephrocalcinosis and unrelated to the underlying disease. The molecular study found a change in homozygosity in intron 5 of gene SLC34A3 (NM_080877.2:c[ 448 +5G>A] + [ 448 +5G>A] ). His three children were carriers of the same variant in heterozygosis and although they were clinically asymptomatic two of them had hypercalciuria. All these data suggest that the patient had hereditary hypophosphataemic rickets with hypercalciuria (HHRH) secondary to an alteration in the sodium dependent phosphate cotransporter located in proximal tubule (NaPi-IIc). The HHRH is transmitted by autosomal recessive inheritance and is an extremely rare form of hypophosphatemic rickets. The diagnosis and treatment are essential to prevent bone sequelae of rickets and nephrocalcinosis. A correct differential diagnosis with other forms of hypophosphatemic rickets has implications on the treatment, as the management based only on phosphorus supplementation usually corrects all clinical and biochemical abnormalities, except for the loss of phosphorus in the urine. The exogenous supply of calcitriol, as advised in other hypophosphatemic rickets, may induce renal calcium deposits and nephrocalcinosis and worsens the prognosis.
INTRODUCTION
There are several forms of hereditary hypophosphatemic rickets associated with a decrease in renal reabsorption of phosphorus.1-3.The majority of them are characterized by a 1,25 OH2 vitamin D3 inappropriately normal, or low and hypocalciuria, indicating that the underlying abnormality that produces them alters the renal transport of phosphorus and the production of calcitriol.1-3
The most prevalent familiar form is hypophosphatemic rickets linked to the X chromosome (XLRH), caused by mutations in the PHEX gene.1-3
Approximately 30 years ago a very rare variant was described, known with the name of hereditary hypophosphatemic rickets with hypercalciuria (HHRH). This one, unlike other forms of hypophosphatemic rickets, presents with elevated levels of 1,25 OH2 vitamin D3 , hypercalciuria and depressed parathyroid hormone (PTH).4-10
In this study we describe an adult male patient whose phenotypic characteristics and genetics correspond with a HHRH.
CLINICAL CASE
We present the case of a 50 year-old man evaluated in the Urology Department of our hospital, presenting a recurrent renal calculus disease since the age of 36. In total, he had formed 12 calculi with spontaneous expulsion of the last calculus a few weeks before visiting our unit.
Personal History: He refers that in the first years of his life he had a deformity of the lower extremities (BLE), with the right leg arched outward and the left one inward, which made him walk in an unusual way. As he did not improve, at the age of 13 he underwent surgery for BLE, subsequently improving his gait in a relevant way. In 1996 presented a multiple fracture in the left lower extremity in relation to a car accident, in which he underwent several surgical operations. He is currently awaiting a prosthetic knee replacement. He has received treatment with calcium orally for many years. In recent months high blood pressure has been detected, which has been treated first with enalapril and subsequently with amlodipine.
Family history: The patient has two brothers and three children (two boys and one girl), all of whom are healthy, without bone alterations. Their parents died, but he recalls that his father had a recurrent renal lithiasis, having been operated on several occasions.
Clinical examination: Weight: 67.2Kg. Size: 148cm. Low stature. Genu varum bilateral. No additional pathological findings.
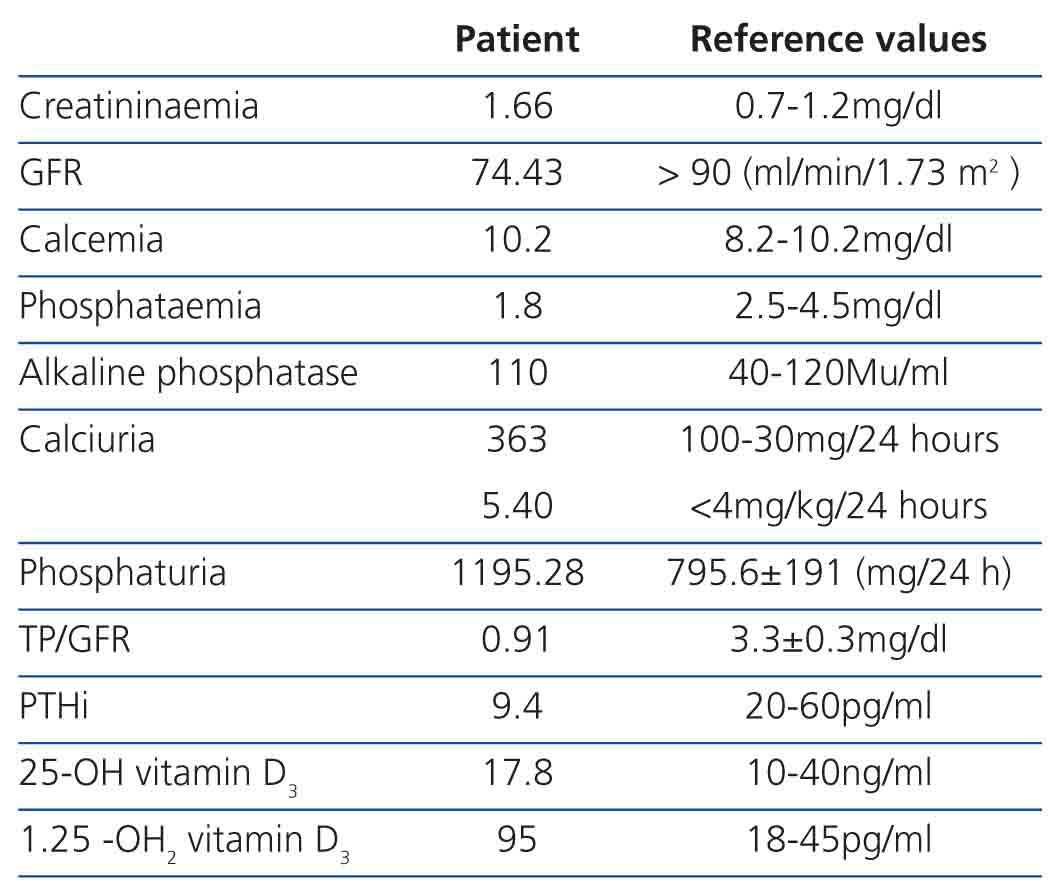
Supplementary examinations: Supplementary examinations: The baseline blood biochemical study carried out on the patient is shown in Table 1. In addition, he presented a uraemia of 55mg/dl (reference value [RV]: 10-50), a calcium-ion of 1.28mmol/l (RV: 1.12-1.35), and a magnesaemia of 1.8mg/dl (RV: 1.59-2.5). In the metabolic and renal function study carried out in 24-hour urine was as follows: glomerular filtration rate (GFR) discretely dropped from 74.43 ml/min/1.73m2; a phosphaturia of 1195.28mg/24 hours (RV: 795.6±191); a tubular reabsorption of phosphate (TRP) and a tubular reabsorption of phosphate per 100 of GFR (TP/GFR) much diminished, 51% (RV: 87.44±5.50) and 0.91mg/dl (RV: 3.30±0.3), respectively; and a hypercalciuria of 363mg/dl (RV: 100-300), and a mild glomerular proteinuria <0.3 g/24 hours. The β2-microglobulin and the α1-microglobulin in urine were normal, so that a tubular proteinuria was ruled out. The serum electrolytes, uric acid, and oxalate were normal both in blood and urine. Glycosuria was never detected. The study of amino acids in the blood and urine, clearance and the tubular reabsorption of each one of them were normal. The bicarbonataemia conducted in capillary blood was normal. The urinary pH was repeatedly alkaline, and citraturia was at the lower limit of the normal range, being of 399mg/24 hours (RV: >320mg/24 hours).
In order to rule out an incomplete renal tubular acidosis, an acidification test is carried out after an oral overload of ammonium chloride according to the previously described.11 In the maximum moment of blood acidification, the urinary pH was maintained above 5.5 (RV: 4.89±0.24 ) and the maximum levels of the titratable acidity, ammonium and net excretion of hydrogen ions did not reach the normal values, being 18.28Eq/min/1.73m2 (RV: 43.12±10.21 ), 19µEq/min/1.73m2 (RV: 63,80±19,54) and 36µEq/min/1,73m2 (RV: 107.17±28.18 ), respectively (analytical standard of incomplete distal renal tubular acidosis). An oral calcium overload was carried out after seven days of a diet free of calcium and salt, according to the protocol described above.12 Before the calcium overload, while fasting and after the hypocalcaemia diet, the quotient calcium/creatinine in isolated urine was 0.17mg/mg. After the overload, this ratio rose above the normal range, being of 0.23mg/mg. The intact PTH (iPTH) remained diminished and the 1,25 OH vitamin D high (analytical standard of idiopathic hypercalciuria type III of Pak with gastro-intestinal absorption of calcium and increased secondary to a loss of renal phosphorus). In the radiologic study carried out repeatedly (plain abdominal radiography, ultrasound and intravenous renal urography), showed a very important nephrocalcinosis medullary bilateral.
Genetic Study: The molecular study carried out on the patient (polymerase chain reaction and bi-directional sequencing), we found a change in homozygous in intron 5 of the SLC34A3 gene (NM_080877.2:c. [448 +5G>A] + [448 +5G>A]). The in silico analysis did not resolve the benignity or pathogenicity of the variant, so we proceeded to study the segregation of this in his three sons, showing that all three had the same change in the SLC34A3 gene in heterozygosis (carriers). We were not able to carry out the study of the messenger RNA (mRNA). The metabolic and renal function study of the three children was normal, except that the two boys only had mild hypercalciuria.13.14
DISCUSSION
HHRH was first described in 1985 by Tieder et al. in a Bedouin family, expounding the cases of six affected members.4 This is a very rare process that is transmitted in an autosomal recessive manner and is manifest from childhood. Patients with this disease have rickets, bone deformities, short stature, muscle weakness and bone pain. The condition is characterized by secondary hypophosphatemic rickets/osteomalacia to excessive loss of renal phosphate and at an elevation of 1,25 OH2 circulating vitamin D3, as a response to the hypophosphatemia. Consequently, hypercalciuria appears, due to an increase in gastrointestinal absorption of calcium and phosphorus, with depression of parathyroid function. Hypercalciuria and elevated levels of 1.252 OH vitamin D 3 are precisely those that differentiate the HHRH from other forms of rickets/hypophosphatemic osteomalacia.2,15,16 As a result of the hypercalciuria, it can originate a nephrocalcinosis or lithiasis, as well as a kidney failure.
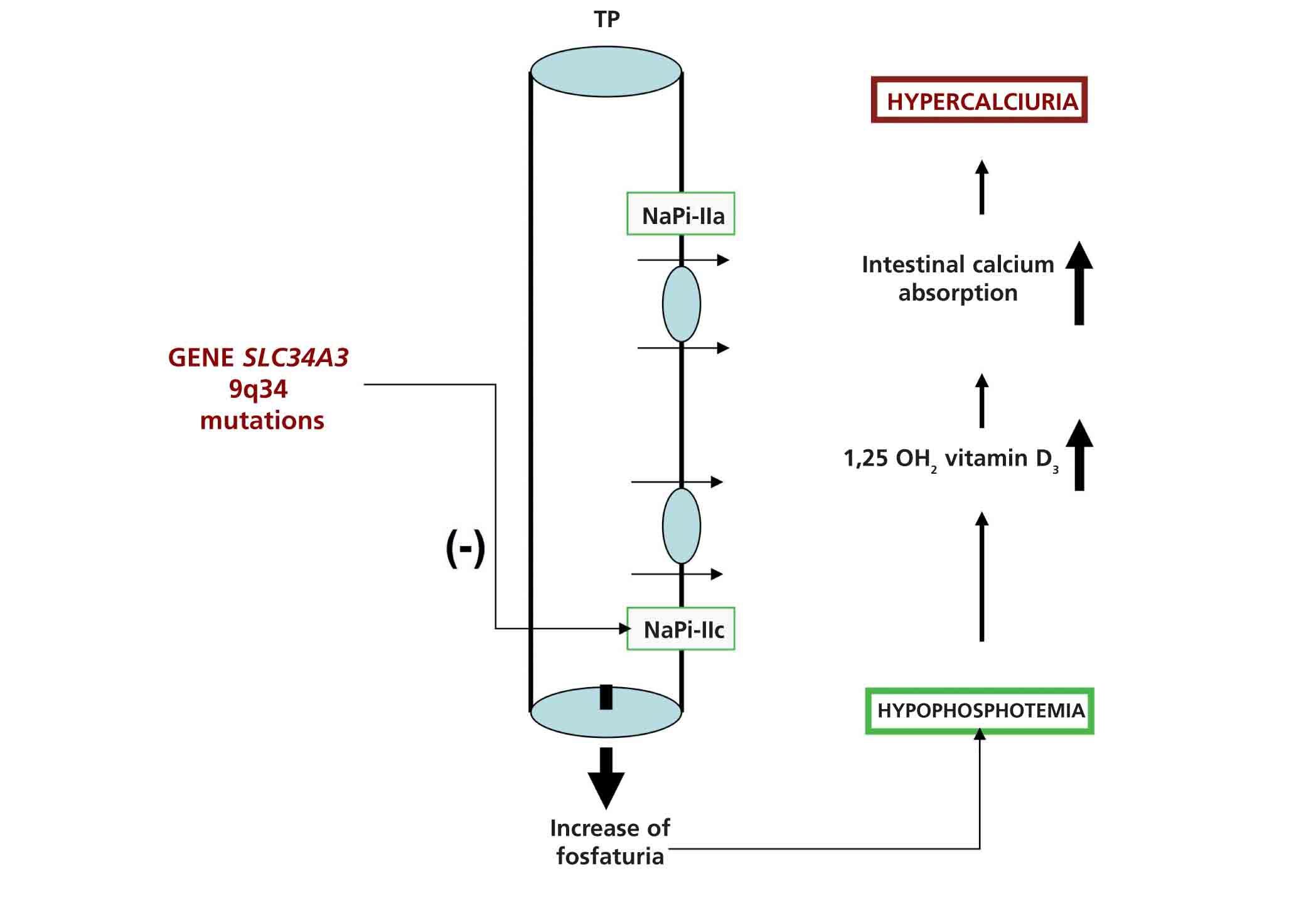
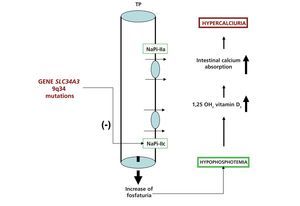
It has recently been published that HHRH (OMIM#241530) is due to mutations in the SLC34A3 gene, located in the chromosomal locus 9q34 that encodes the sodium-phosphate cotransporter IIc (NaPi-IIc), which is expressed in the apical membrane of renal proximal tubular cells and that normally regulates the reabsorption of phosphate filtering, under the control of the PTH and fibroblast growth factor (FGF23). Function-loss mutations in SLC34A3 cause increased phosphate excretion at proximal level, characteristic of the disease2,10,13 which can give rise to different phenotypic changes (Figure 1).17,18
In studies of patients with HHRH it has been shown that by simply using a phosphate salt supplement orally all the clinical, biochemical analytical and radiographic features of the condition may be corrected except for the excessive loss of renal phosphate. This suggests that hypophosphatemia, in the absence of alterations in the of vitamin D metabolism, play an important role in bone metabolism.6.8
On the other hand, since the nephrocalcinosis is probably linked to the hypercalciuria, the administration of calcitriol, calcium or the failure of the treatment with the phosphorus supplementation can promote renal deposits of calcium and overshadow the prognosis in these patients.6.8
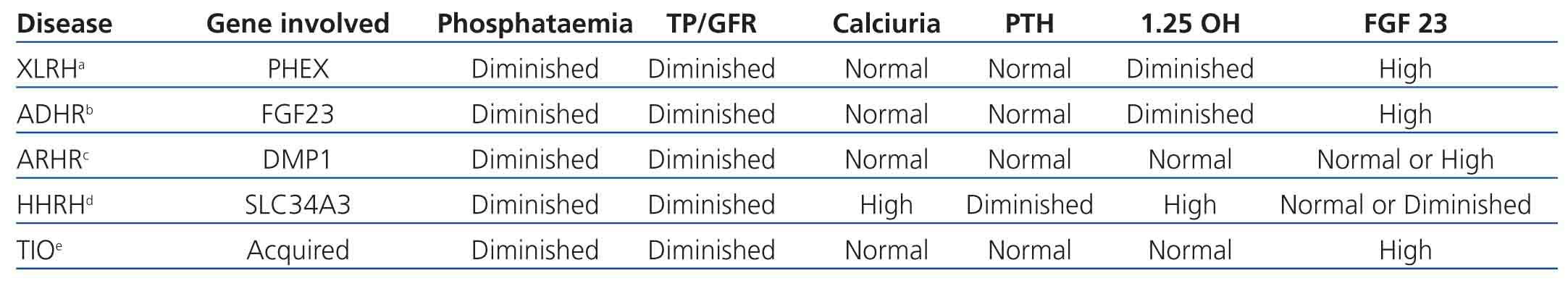
Currently it is considered that there is a bone-kidney axis in which multiple genes are involved and which regulates the metabolism of phosphorus and the mineralization of bone matrix. The main exponent of this axis is FGF23, the first phosphatonin that was discovered and that is produced by the osteocytes. The NaPi-IIc, together with other proteins such as PHEX, MEPE and DMP1, participate in the regulation of the axis (Table 2).2.3,19,20
The patient described in this study met all the clinical and laboratory characteristics compatible with HHRH. Rickets/hypophosphatemic osteomalacia and to the diminished tubular reabsorption of phosphate associated with an elevation of the 1,25 OH2 circulating vitamin D3 and a hypercalciuria. This ruled out XLRH, which is the most common form of hereditary hypophosphatemic rickets that is due to inactivating mutations in the gene PHEX (OMIM# 307800) and where the PTH is normal and the 1,25 OH2 vitamin D3 abnormally low for the phosphatemia levels.3.15,20 For the same reason, three more forms of hypophosphatemic rickets could also be ruled out: tumour-induced hypophosphatemia, which is secondary to various phosphatonins secreted by benign tumours of mesenchymal origin (SFRP-4, MEPE, FGF-7)20; the autosomal dominant hypophosphatemic rickets, which is a form of hypophosphatemic rickets very rare with variable penetrance, biochemically similar to XLRH and due to mutations in the gene FGF23 (OMIM# 193100),21 and autosomal recessive hypophosphatemic rickets (OMIM# 241520), caused by mutations in the gene DMP1.20 Finally, the absence of a tubular proteinuria also ruled out Dent's disease, an X chromosome-linked entity caused by mutations in the CNCL5 gene encoding the electrogenic Cl-/H+ exchanger of the chloride channel family, which is expressed in endosomes of the proximal tubular epithelium and also show hypercalciuria (Table 2).22
Our patient had an incomplete renal tubular acidosis, clearly reflected in the acidification test. Patients with hypercalciuria and nephrocalcinosis are known to present abnormal renal acidification capacity and acidosis as a consequence of nephrocalcinosis. The renal failure present in our patient also was secondary to the nephrocalcinosis, rather than directly related to the SLC34A3 mutation.23-25
The molecular study showed a homozygotic change in intron 5 of the SLC34A3 gene (NM_080877.2:c[ 448 +5G>A] + [ 448+ 5G>A] ). The fact that the three healthy children of the patient presented the same sequence variation in the SLC34A3 gene in heterozygosis and that the two boys presented hypercalciuria would suggest that the genetic alteration detected being was the cause of hypophosphatemic rickets. A mutation located also in intron 5 (NM_080877.2:c.448 +1G>A), which was very close to the variant found in our patient, has been recently described.17
In conclusion, we present a patient with hypophosphatemic rickets that, according to the clinical symptoms, the biochemical signs and genetic study, is compatible with HHRH. Early diagnosis and treatment are essential for preventing bone sequelae of rickets and nephrocalcinosis. The correct distinction with the other forms of hypophosphatemic rickets has implications in the treatment, since the isolated administration of phosphorus supplements corrects all clinical and biochemical alterations, except the loss of phosphate in the urine. The contribution of exogenous calcitriol as recommended in other cases of hypophosphatemic rickets, can favour renal deposits of calcium and the emergence of nephrocalcinosis, as well as worsen their prognosis.
Molecular study conducted at the Institut für Humangenetik des KlinikuMs rechts der Isar der Technischen Universität München. Direcktor: Univ. Prof. Med. Th. Meitinger POLIKLINIK.
Conflicts of interest
The authors state that they have no potential conflicts of interest related to the contents of this article.
Table 1. Biochemical parameters of the patient with HHRH
Table 2. Types of hypophosphatemic rickets, genes and biochemical characteristics of each one of them
Figure 1. Schematic representation of the reabsorption of phosphorus in the apical membrane of proximal tubule and the biochemical consequences of the mutations with loss of function in the gene SLC34A3.