Objetivo: Estimar la calidad de vida en pacientes con enfermedad renal crónica, que no han recibido ni diálisis ni trasplante, y su asociación con factores de riesgo. Diseño: Estudio descriptivo transversal de una muestra representativa de pacientes de dos entidades promotoras de salud colombianas. Se aplicó el instrumento de medición de calidad de vida SF-36 y las puntuaciones se relacionaron con datos demográficos, clínicos y de laboratorio. Resultados: La mediana de edad fue 70 años, un 67% eran hombres, un 93% tenían hipertensión arterial y un 67% se encontraban en estadio 3. La medida de salud física de calidad de vida se vio más afectada que la medida de salud mental (Wilcoxon, p <0,001). Los dominios de función física, desempeño físico y dolor corporal se vieron menos afectados en hombres y en jóvenes. La salud física estuvo más relacionada con variables sociodemográficas y clínicas. Las personas con enfermedad renal crónica mayores de 65 años, mujeres y con diabetes presentaron una menor puntuación del componente físico. La salud mental tuvo un menor valor en las mujeres. Después de ajustar por edad, no se encontró asociación entre la tasa de filtración glomerular y la salud física. La calidad de vida es mejor en los hombres (p <0,001) y un 12,5% de la varianza de dicha diferencia se explica por la edad. Conclusiones: Los pacientes con enfermedad renal crónica sin diálisis ni trasplante presentan una mayor alteración de la calidad de vida que la población general, principalmente en el componente físico; las mujeres mayores de 65 años se vieron más afectadas.
INTRODUCTION
Chronic kidney disease (CKD) is a known public health problem due to its impact on quality of life in people of all ages,1,2 the rapid increase in its prevalence, and the ¿iceberg¿ effect caused by lack of knowledge of its true magnitude, due both to insufficient detection and under-recording of patients in early stages. In Colombia, terminal CKD is listed as a high-cost disease according to the social health care system,3 which uses insurance to make an EPS (healthpromoting entity) responsible for offering its subscribers dialysis and kidney transplant services.
The damage produced by CKD is rarely perceived by patients during early stages, which means that while alterations may exist, the patient may not be aware of their magnitude. Factors other than the disease may affect the perception and evaluation of quality of life and generate hard-to-control variations that modify how it is measured4.
World Health Organization defines quality of life as "individual perception of one's position in life within the context of cultural and value system in which they live and in relation to their objectives, expectations, standards and concerns".5 Different studies have examined the relationship between function and well-being in patients undergoing different types of treatment after the appearance of kidney failure,6-14 but there are not enough publications that explore the relationship between pre-dialysis renal function and quality of life.15 Until 2008, there were no publications on MEDLINE or LILACS regarding this topic in the context of Colombia.
Supported by scientific evidence, the KDOQI15 guidelines recommend evaluating function and well-being in patients with CKD from early stages on, using validated instruments including the Medical Outcomes Study 36 item short form SF-36, which was adapted to a Colombian cultural perspective.16
This study estimates quality of life in patients with CKD who subscribed to either of two health insurance companies in Medellin during 2008. It aims to provide scientific evidence as to the relationship between quality of life and CKD in early stages, thus contributing to designing effective, science-based interventions.
MATERIAL AND METHOD
We conducted a transversal descriptive study in a sample of CKD patients without dialysis or transplants to whom the SF-36 had been applied. The resulting quality of life scores were linked to demographic, clinical and laboratory variables which were obtained from the clinical history available from the insurers.
The eligible population was made up of 5,884 patients who met the following criteria: a) subscribing to a policy with either of the insurers in 2007 b) having been diagnosed with CKD according to the KDOQI guidelines effective for 2007 c) being older than 16 years and d) not having undergone dialysis or a kidney transplant.
The CKD diagnostic criteria according to the KDOQI guidelines were as follows:
- Creatinine clearance below 60ml/min* using MDRD if that method was recorded in the clinical history, or if not, using Cockcroft-Gault.15,17
- Proteinuria: > 150mg/24 hours*.
- Microalbuminuria > 30mg*.
- Urinalysis: more than three erythrocytes per HP field*.
- Abnormalities in imaging studies.
*During more than three months.
Since quality of life will be evaluated once more in these patients a year after recording these scores, we used a formula for a repeated-measurement design, proposed by Frison and Pocock in 199218 with following criteria: error type 1: 0.05, error type 2: 0.20 (power: 80%), a difference of 10 between the mean values of the two groups, standard deviation (SD) of 34 points for both group (higher SD observed in the validation of the SF-36 dimensions); the correlation between the baseline and follow-up measurements was set at 0.5.
We obtained a minimum sample size of 137 patients per health-promoting entity for a total of 274. Anticipating the difficulty in contacting patients due to high rates of mobility, we used 50% oversampling to obtain a final sample of 411. Of this number, we were able to contact 293, which guaranteed the desired representative sample. Of the 118 remaining patients who could not be interviewed, the reasons were as follows: wrong telephone number in the clinical history (43 [36.4%]); subjects refused because they were busy (33 [28%]); residence outside of a certain geographical area (17 [14.4%]); met exclusion criteria (14 [11.9%]). Only 11 patients, representing 9.3% of those who were not interviewed, were excluded due to concomitant illness or death.
The information was gathered by medical students with knowledge of diagnostic criteria and the handling of instruments for a pilot study. The SF-36 survey was administered in a personal and supervised environment after obtaining patients¿ informed consent. Once it was completed, it was verified for proper use. The selected patients were undergoing tests by general physicians in order to manage their conditions having to do with cardiovascular risk, and by internal medicine specialists and nephrologists to manage the CKD according to the policies of the responsible insurers.
To calculate SF-36 dimensions, we used a formula to transform the ordinal scale for the items into the corresponding number of points from 0 to 100.20 We also calculated the summary measurements for the physical health components (PCS1) and mental health components (MCS1) respectively. Each of these two components includes four SF-36 dimensions as follows: PCS1: physical functioning (PF), role-physical (RP), body pain (BP) and general health (GH). MCS1: vitality (V), social functioning (SF), emotional role (ER) and mental health (MH). To calculate these values, we considered the method used in a reproducibility study for the different summary measures from the SF-36 to evaluate quality of life in schizophrenia patients.21
The statistical analysis of qualitative variables was carried out using proportions. Quantitative variables were analysed using measurements of position, central tendency and dispersion. The summary measures for quality of life were compared to one another using the Wilcoxon test in order to establish statistical differences between the physical and mental components. In the study, we used the Mann-Whitney U test; however, we also applied the Student t-test in order to compare our results with those in the literature.
When relating the PCS1 and the MCS1 to gender and comorbidities, we used the chi-square test of independence, and Fisher¿s exact test wherever anticipated values were below 5. When relating the CKD stage with other variables, we used the chi-square trend test. To observe the association between quantitative variables, we calculated the Spearman correlation coefficient in the case of nonnormal variables, and later evaluated their significance by means of a statistical hypothesis test.
The relationship between the glomerular filtration rate (GFR) and the PCS1 was studied and adjusted by age by means of stratified analysis with the Mantel-Haenszel and Breslow Day tests.22,23 Lastly, we constructed an explicative analysis of covariance model (ANCOVA) to account for the PCS1¿s variation percentage per gender, explained by age, once the suppositions required for this type of model were verified. SPSS software version 15.0 was used for data analysis.
RESULTS
General characteristics and estimated quality of life
The interviewed patients were between the ages of 18 and 98 years and the age distribution was not normal (Kolmogorov-Smirnov, p < 0.001).
In the responses to questions on the SF-36 in the ¿physical functioning¿ dimension, we observed a significant limitation on participating in intense physical activity such as running or lifting heavy objects (item 3a) in 55.3% of the 293 interviewed patients. For all other evaluated activities, rated from moderate, such as washing up or moving a table, to the least physically demanding, such as bathing or getting dressed, most of the responses indicated that there were no limitations (items 3b-3j).
For the ¿role-physical¿ dimension in the previous four weeks, two thirds of the participants had not experienced any problems with completing their work or other normal daily activities due to their physical health (items 4a-4d). During the last month, 31.7% of the participants did not experience any sort of pain (item 7), and for 56.7%, the pain did not interfere with normal work (item 8).
¿General health¿ was considered to fall between average and good by 76.7% of the participants (item 1). 48.1% considered it to be completely false that they fell ill more easily than other people (item 11a); likewise, 54.3% of patients expressed that, in general terms, they were as healthy as any other person (item 11b). Furthermore, one third did not believe that their current state of health would get worse (item 11c), and 51.9% rated their state of health as excellent (item 11d).
57.7% stated that they always or nearly always felt full of vitality (item 9a) and a similar percentage expressed that they were very energetic (9e). About half of the patients stated that they never or almost never felt exhausted (9g) or tired (9i).
When evaluating quality of life through the ¿social functioning¿ (items 6 and 10), two thirds of the subjects stated that during the last four weeks their social life had not been affected in any way, and that they had been able to carry out normal activities with their families, friends, neighbours and others.
More than 70% of the participants responded that their ¿roleemotional¿ had not affected either their work or other normal daily activities in the past four weeks, whether because of the time dedicated to these tasks (item 5a) or because of the care they require to fulfil them (item 5c). When evaluating ¿mental health¿, we observed that the frequency of responses indicating a perceived state of nervousness (item 9b) or feeling down (item 9c), or discouraged and sad (item 9f) was very low in the last month. More than a third of the patients stated that they always felt happy (item 9h), and the same percentage felt calm and peaceful (9d). When evaluating ¿changes in health¿ after comparing the general current state of health with that recorded a year ago, 42.7% felt no different.
Relating quality of life to socio-demographic and clinical variables
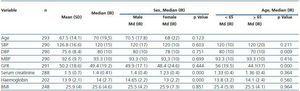
None of the clinical markers presented a normal distribution except for haemoglobin; the median glomerular filtration rate (GFR) was related to stage 3 CKD, which was the most common stage, and there was a significantly different tendency with a larger proportion of patients in advanced stages for the group aged 65 and older. Women showed significantly lower median creatinine serum values; haemoglobin was at a clinically normal average level, and the median body mass index was in the overweight range. (Table 1).
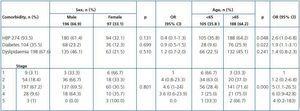
The most frequent comorbidity was arterial hypertension, although the mean recorded blood pressures were not abnormal. Two thirds of the patients presented dyslipidaemia concomitant with CKD, and one third had diabetes mellitus (DM). DM and HBP were more prevalent in patients older than 65 years, and there were no statistically significant differences between the sexes. (Table 2).
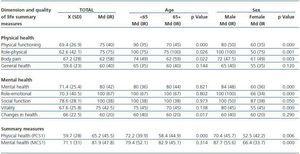
Upon analysing dimensions and summary measures we found a better level of quality of life in role-emotional and social functioning; body pain, general health and changes in health were rated lower by patients. The summary measure for physical health was more affected than that for mental health.
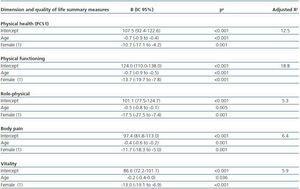
The medians for physical functioning, role-physical and body pain dimensions by gender and age were higher in younger men. Mental health dimensions only presented significant differences by gender, as they were lower in women. (Table 3).
The summary measure for physical health was more related to socio-demographic and clinical variables than the mental health summary measure was. CKD patients older than 65, females and those with DM scored fewer points for quality of life on the physical health summary measure.
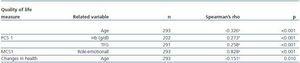
We found a close correlation between the mental health summary measure and the role-emotional dimension which was not affected by collinearity between the two (Variance Inflation Factor: 4.7. Tolerance: 0.2). GFR has a moderate negative correlation with serum creatinine and age, and a slight positive correlation with the physical health summary measure. This last was also negatively correlated with age, and positively with haemoglobin levels. (Table 4).
Relationship between GFR and the age-adjusted quality of life physical component
Patients with a GFR below 60 were 1.8 times more likely of having a physical health score below 65 than those who presented a GFR greater than or equal to 60. Diabetes mellitus and dyslipidaemia were ruled out as possible confusion variables for this association. When the relationship under study was adjusted for age, we found that none of the ORs obtained from the strata was significant (< 65 years: OR = 2.39, p = 0.055 95%, CI = 0.97- 5.91; and > 65 years: OR = 1.03, p = 0.944, 95% CI = 0.42- 2.53), and furthermore, no significant differences were found among the strata (Breslow Day, p = 0.193). The adjusted OR (1.58) lost statistical significance (Mantel-Haenszel, p = 0.149, 95% CI: 0.84- 2.95). Age acted as a positive confounder in the relationship between GFR and the PCS1.
Quality of life adjusted by gender and age
The ANOVA for the PCS1 accounted for the statistical differences between men and women, and in addition, the ANCOVA enabled adjustment of this value for gender and age, once the homocedasticity assumptions were verified (Levene p = 0.988) and linear relationship assumptions (F age: p < 0.001, sex: p = 0.001), which showed a sex-based difference in the summary measure for quality of life which was explained by age in 12.5% (corrected R2). This means that for each year-long increment in age for CKD patients in the study, there is a decrease of 0.66 points in the quality of life physical component score, and 10 points for omen older than 65.
When we analysed the physical functioning dimension, variation by gender was explained by age in 19% of subjects, while in the role-physical and body pain dimensions, age accounted for less than 7% of variation by gender. (Table 5).
DISCUSSION
This study included 293 patients, nearly 90% of whom were in stages 1, 2 and 3 unlike in other studies such as that of the Renal Research Institute (RRI) where the largest groups studied were in stages 3, 4 and 5.24
A larger proportion of male patients (67%) is a trait that is also present in other studies, such as the African American Study of Kidney Disease and Hypertension Trial Study Group (ASSK) in which 61.2% of the population was male,25 and in Fukuhara¿s study of the Japanese pre-dialysis population which was 67% male.26With regard to age, most of the studies show populations with an average age above 50 years: in the AASK study the mean age is 54.5 years, in the RRI study, 60.7 years, and in the Japanese study, the difference is nearly 10 years; in all cases, our population is older, although it is classed in earlier stages.
The creatinine levels we found were different from those in other publications. The average value in the Japanese study was 4.5mg/dl, much higher than our own, which could be explained by the criteria used for diagnosing CKD. According to KDOQI criteria, many patients can be diagnosed with CKD with no need of having high creatinine values, whereas in Fukuhara¿s study, creatinine > 1.5mg/dl was the only diagnostic criterion.26 Similarly, we found differences in the related diseases, highlighting that HBP had a higher prevalence than DM, unlike what occurs in the North American population.
With regard to quality of life, CKD patients without dialysis or transplants state that their physical condition is affected more than their mental condition. Upon comparing our results with results from AASK and other previous studies with different populations such as African-Americans with and without hipertension,27 a sample from the general population in the United States,28 hypertensive patients29 and patients on dialysis in the HEMO study,30 we find that each of the dimensions and the PCS1 were substantially higher in the AASK study compared with patients in the HEMO study. However, we found no significant differences between the MCS1 values for these same studies. These results concur with studies that have shown how SF-36 is sensitive for detecting changes in quality of life secondary to progressing renal damage, and how patients are capable of maintaining mental well-being despite a decrease in physical wellbeing.31
It is possible to state that estimated quality of life in CKD patients without dialysis or transplant is lower than that found in studies of the general healthy population,but higher than the values expressed by patients undergoing dialysis. Research on transplant patients32 shows similar results to those in our own study, except for the «vitality» and «body pain» dimensions. In the first case, we observe a better score in patients without dialysis, and in the second, a better score for patients with kidney replacement therapy.
Compared with the healthy Colombian population,33 patients in our study have a lower score in the physical component dimensions, but no such variation occurs in the mental component dimensions. And if we use other studies applied to the healthy Spanish population as a reference,34 the physical component is still the one that decreases the most in the study population with CKD. Likewise, we see similar behaviour in the results when compared to the worldwide tendency for CKD patients in pre-dialysis stages. One example is the literature review by the Sociedad Española de Nefrología (Spanish Society of Nephrology)35 on the quality of life studies in CKD patients without kidney replacement therapy, which concludes that the physical aspects are affected more than mental and social aspects.
On this subject, we must cite some studies36-38 which concluded that it was important to include a physical conditioning programme specifically designed for patients on dialysis, since the physical component is the one with the most significant deterioration. This recommendation could also apply to pre-dialysis patients.
Age plays a very important role in regard to quality of life, as it is negatively associated with physical functioning, rolephysical, body pain and general health dimensions, and with the summary measure for physical quality of life; this statement coincides with the information we reviewed.25,34,39,40 With regard to gender and quality of life measures, we find that women with CKD are in poorer condition, as was also shown by previous studies.25,26,34 The result of the ANCOVA model concurs with the linear regression model found in the Australian population study in which the scores for all physical component measures decreased as age increased.39
Sex and age are important factors in the evaluation of quality f life for patients with renal damage. This may be taken into account when designing programmes intended to manage kidney disease in such a way as to affect the population at the most risk for decreased quality of life; this population is female, particularly those older than 65 or having a GFR of less than 60ml/min/1.73m2.
One of this study¿s limitations is the fact that in some cases, clinical data from the clinical history was taken as much as 3 months before the date on which the SF-36 was filled out. Furthermore, we recognise a possible selection bias due to people not filling out the survey for illness-related reasons, which could produce underestimation of the decrease in quality of life; the patients with the most severe conditions would not have been included.
Lastly, we must gather more evidence to identify changes in the estimated quality of life of CKD patients in early stages. Since there is an alteration from the disease¿s initial phase, it is possible to evaluate the impact of interventions to preserve renal function and decrease complications, and therefore, to improve quality of life in this population.
Table 1. Distribution of socio-demographic and clinical characteristics by age and sex in CKD patients without dialysis or transplant. Medellín, 2008
Table 2. Distribution of comorbidities and stages in CKD patients without dialysis or transplant, according to age and sex. Medellín, 2008
Table 3. Distribution of dimensions and summary measures from the SF-36 by age and sex in CKD patients without dialysis or transplant. Medellín, 2008
Table 4. Correlation between quality of life summary measures and the age and clinical characteristics of CKD patients without dialysis or transplant. Medellín, 2008
Table 5. Age- and sex-adjusted ANCOVA models for quality of life in CKD patients without dialysis or transplant. Medellín, 2008