The COVID-19 infection has caused an impact worldwide to the point of saturating health systems in several countries and being the most frequent and serious reason for consultation in the emergency room. Despite the fact that COVID-19 infection mainly affects the lungs, several studies have identified a high tropism of the virus for the renal parenchyma.1 The mechanism whereby nephropathy secondary to COVID-19 occurs is uncertain, since the damage may be directly related to viral infection or to kidney injury due to extracellular volume depletion, cytokine release, and activation of the renin angiotensin system.2 The most frequent renal lesions at the histological level are: acute tubular injury and collapsing glomerulosclerosis, because the virus could be directly or indirectly toxic in the podocyte.3
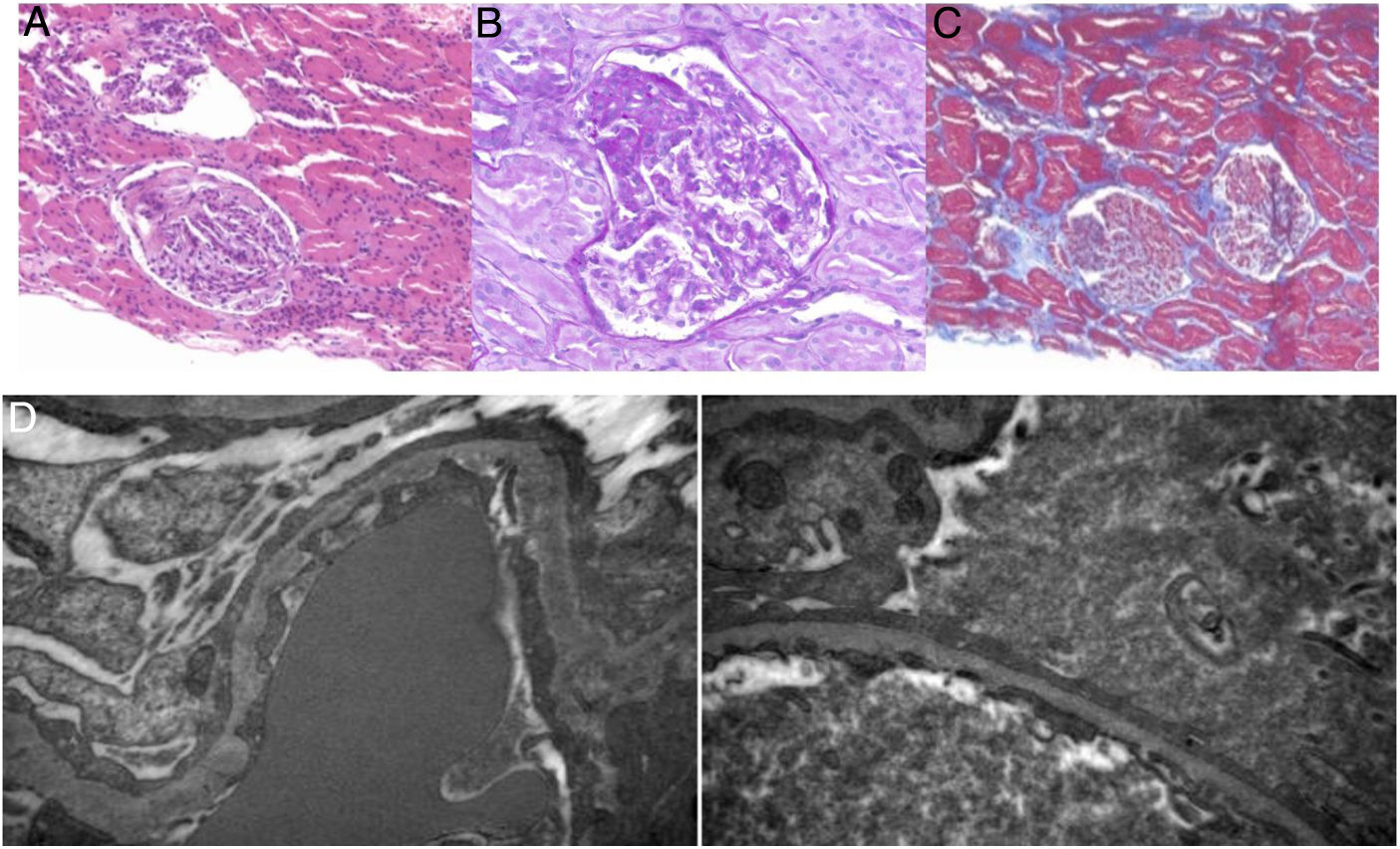
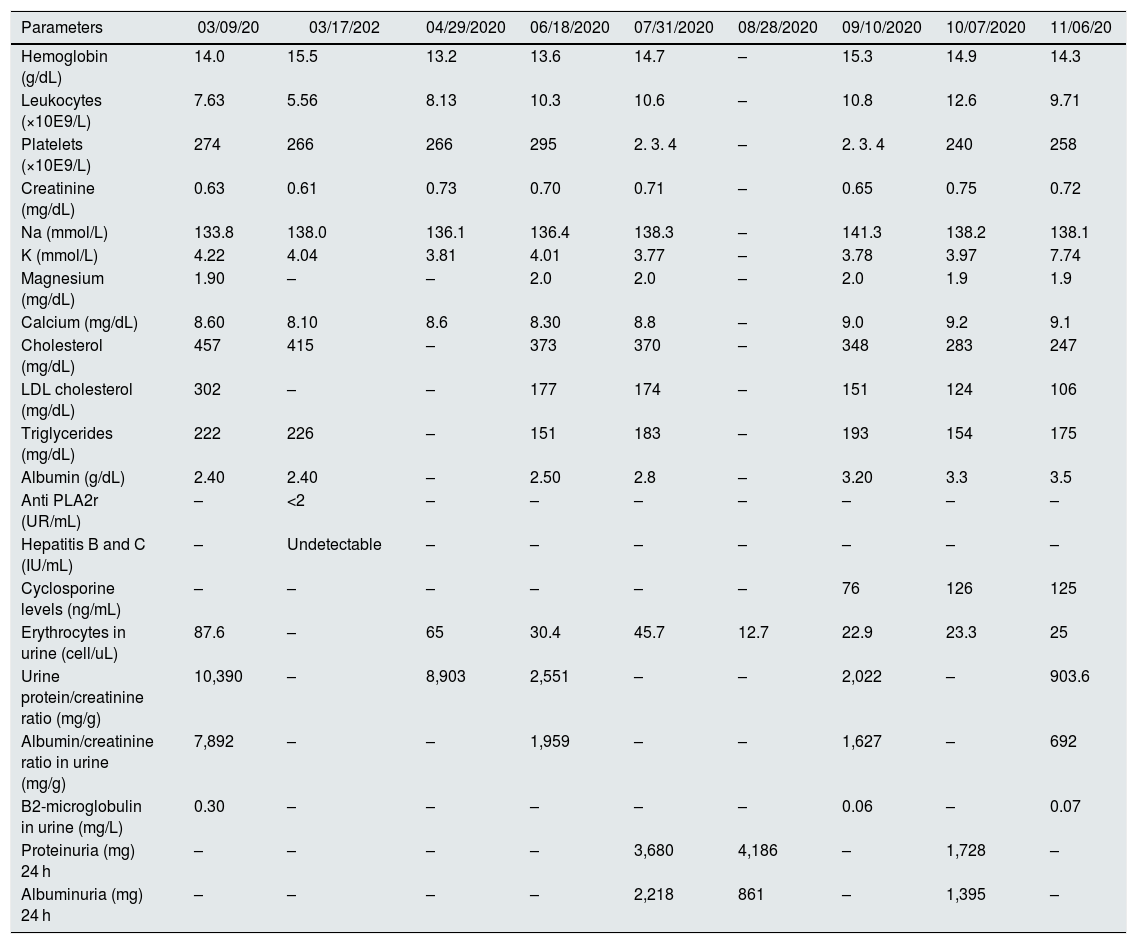
It is described the case of a 56-year-old patient with a 25-pack/year smoking history, hypertension, dyslipidemia, and anxiety-depressive syndrome. He attended the outpatient clinic due to nephrotic syndrome of two weeks duration (blood albumin 2.4 g/dL, urine protein/creatinine 10,390 mg/g with urine albumin/creatinine of 7892 mg/g) (Table 1) associated to dry cough and asthenia in the context of mild COVID-19 infection. Primary causes and autoimmune diseases were ruled out (Table 1). The chest and abdominal tomography did not show lesions suggestive of neoplasia or metastasis. Renal biopsy showed unspecified variant focal segmental glomerulosclerosis not otherwise specified (FSGS NOS) (Fig. 1), SARS-CoV-2 polymerase chain reaction (PCR) study in frozen tissue from kidney biopsy was negative. Furthermore, electron microscopy did not reveal COVID-19 viral particles. The temporal sequence of clinical events and negative autoimmune laboratory results made the diagnosis of focal segmental glomerulosclerosis (GFyS) associated with COVID-19, for which treatment with prednisone at 60 mg per day was started. After 12 weeks and given the persistence of proteinuria, cyclosporine 100 mg every12 h was added gradually increasing to 125 mg every 12 h. Likewise, corticoid dose was progressive decreased to 20 mg per day with a reduction in urine protein/creatine and urine albumin/creatinine of 903.6 mg/g and 661 mg/g, respectively.
Evolution of laboratory parameters of the patient with focal and segmental glomerulosclerosis due to COVID-19.
| Parameters | 03/09/20 | 03/17/202 | 04/29/2020 | 06/18/2020 | 07/31/2020 | 08/28/2020 | 09/10/2020 | 10/07/2020 | 11/06/20 |
|---|---|---|---|---|---|---|---|---|---|
| Hemoglobin (g/dL) | 14.0 | 15.5 | 13.2 | 13.6 | 14.7 | – | 15.3 | 14.9 | 14.3 |
| Leukocytes (×10E9/L) | 7.63 | 5.56 | 8.13 | 10.3 | 10.6 | – | 10.8 | 12.6 | 9.71 |
| Platelets (×10E9/L) | 274 | 266 | 266 | 295 | 2. 3. 4 | – | 2. 3. 4 | 240 | 258 |
| Creatinine (mg/dL) | 0.63 | 0.61 | 0.73 | 0.70 | 0.71 | – | 0.65 | 0.75 | 0.72 |
| Na (mmol/L) | 133.8 | 138.0 | 136.1 | 136.4 | 138.3 | – | 141.3 | 138.2 | 138.1 |
| K (mmol/L) | 4.22 | 4.04 | 3.81 | 4.01 | 3.77 | – | 3.78 | 3.97 | 7.74 |
| Magnesium (mg/dL) | 1.90 | – | – | 2.0 | 2.0 | – | 2.0 | 1.9 | 1.9 |
| Calcium (mg/dL) | 8.60 | 8.10 | 8.6 | 8.30 | 8.8 | – | 9.0 | 9.2 | 9.1 |
| Cholesterol (mg/dL) | 457 | 415 | – | 373 | 370 | – | 348 | 283 | 247 |
| LDL cholesterol (mg/dL) | 302 | – | – | 177 | 174 | – | 151 | 124 | 106 |
| Triglycerides (mg/dL) | 222 | 226 | – | 151 | 183 | – | 193 | 154 | 175 |
| Albumin (g/dL) | 2.40 | 2.40 | – | 2.50 | 2.8 | – | 3.20 | 3.3 | 3.5 |
| Anti PLA2r (UR/mL) | – | <2 | – | – | – | – | – | – | – |
| Hepatitis B and C (IU/mL) | – | Undetectable | – | – | – | – | – | – | – |
| Cyclosporine levels (ng/mL) | – | – | – | – | – | – | 76 | 126 | 125 |
| Erythrocytes in urine (cell/uL) | 87.6 | – | 65 | 30.4 | 45.7 | 12.7 | 22.9 | 23.3 | 25 |
| Urine protein/creatinine ratio (mg/g) | 10,390 | – | 8,903 | 2,551 | – | – | 2,022 | – | 903.6 |
| Albumin/creatinine ratio in urine (mg/g) | 7,892 | – | – | 1,959 | – | – | 1,627 | – | 692 |
| B2-microglobulin in urine (mg/L) | 0.30 | – | – | – | – | – | 0.06 | – | 0.07 |
| Proteinuria (mg) 24 h | – | – | – | – | 3,680 | 4,186 | – | 1,728 | – |
| Albuminuria (mg) 24 h | – | – | – | – | 2,218 | 861 | – | 1,395 | – |
Histology of the renal biopsy.
A) Hematoxylin-eosin (10×). B) PAS (periodic acid Schiff) (60×). C) Masson's trichrome (4×). Focal and segmental sclerosis is evidenced in one of 11 glomeruli, tubular atrophy and mild and focal interstitial edema, mild lymphocytic infiltrate, arteries are preserved. D) Electron microscopy shows renal cortical tissue containing a glomerulus. The ultrastructural study shows diffuse effacement of the podocyte processes with 70%–80% pedicellar fusion, differentiation, vacuolization and villous transformation of the podocyte cytoplasm. Findings consistent with focal segmental glomerulosclerosis (10,000–20,000×).
The treatment of FSGS associated to COVID-19 is unknown. Cyclosporine is an immunosuppressant that suppresses interleukin 2 (IL-2) transcription by blocking the activity of calcineurin.4 At low doses, cyclosporin reduces viral load preventing cytokine storm and maintaining the pH within appropriate ranges which prevents ischemia-reperfusion injury.4 Also, cyclosporine inhibits viral replication by blocking the cyclophilin functions of the virus and directly inhibiting RNA-nsp12-dependent RNA polymerase.5
In a recent study, a cohort of 40 patients with glomerulonephritis and COVID-19 infection has shown that they have a higher rate of mortality and acute kidney injury as compared to the control group.6 The use of angiotensin converting enzyme inhibitors (ACEI) and/or immunosuppressive treatment do not increase the risk of death and patients with low serum albumin should be monitored.6 Also, a case of COVID-19 infection has been described in a patient with hypocomplementemic urticarial syndrome and anti-neutrophil cytoplasmic antibody-myeloperodoxodasse (ANCA-MPO) vasculitis on hemodialysis receiving treatment with omalizumab. The patient presented an asymptomatic COVID-19 infection, so the mild course of the infection could be attributable to the background treatment with omalizumab.7 Sharma et al. report 10 patients with severe pneumonia due to COVID-19 who underwent a kidney biopsy due to acute kidney injury, proteinuria and hematuria and define acute tubular necrosis as the most frequent histological involvement (n = 5), despite the fact that all the patients were positive for the SARS-CoV-2 nasopharyngeal smear, they were unable to identify viral particles in electron microscopy of kidney tissues.8 In agreement, Magoon et al. described two cases of focal segmental glomerulosclerosis of collapsing type with podocyte involvement confirmed by renal biopsy with no evidence of virus particles in electron microscopy; both cases showed risk genotypes of the apolipoprotein 1 (APOL1).9 Kissling et al. also described a case of a 63-year-old patient with COVID-19 pneumonia and AKIN 3 ( acute kidney injury network ) with nephrotic syndrome and severe proteinuria; renal biopsy evidenced collapsing type focal segmental glomerulosclerosis with vacuolization of podocytes and absence of virus particles in electron microscopy.10
In summary, this letter presents the case of a patient with a NOS variant focal segmental glomerulosclerosis associated with COVID-19 treated with corticosteroids and cyclosporine with a partial clinical response. Future studies are necessary to improve the diagnosis and subsequent treatment of nephropathies associated with COVID-19.
Please cite this article as: Román JL, Vergara A, Agraz I, García-Carro C, Bermejo S, Gabaldón A, et al. Glomeruloesclerosis focal y segmentaria asociada a infección por COVID-19. Nefrologia. 2022;41:706–708.