Advance care planning (ACP) and the subsequent advance directive document (ADD), previously known as “living wills”, have not been widely used in Spain. The Ethics Group from the Spanish Society of Nephrology has developed a survey in order to investigate the opinion of dialysis patients regarding the ADD and end-of-life care. Patients received documentation explaining ACP and filled out a survey about their familiarity with and approval of the ADD. Seven hospital dialysis centres participated in the study for a total of 416 active dialysis patients. Questionnaires were distributed to 263 patients, 154 of which answered (69.2% completed them without assistance). The rates for ADD implementation (7.9%) and designation of a representative person (6.6%) were very low. Most of the patients clearly expressed their wishes about irreversible coma, vegetative state, dementia and untreatable disease. More than 65% did not want mechanical ventilation, chronic dialysis, tube feeding or resuscitation if cardiorespiratory arrest occurred. They reported that an ADD could be done before starting dialysis but most thought that it should be offered only to those who requested it (65% vs 34%). In conclusion, patients have clear wishes about end-of-life care, although these desires had not been documented due to the very low implementation of the ADD.
La implantación del proceso de planificación anticipada de cuidados y del documento de voluntades anticipadas (DVA) es escasa en España. Por este motivo, el Grupo de Ética y Nefrología de la Sociedad Española de Nefrología (S.E.N.) elaboró una encuesta para conocer la opinión de los pacientes en programa de diálisis sobre el DVA y otras situaciones relacionadas con el fin de la vida.
Los pacientes recibieron documentación explicativa sobre la naturaleza y significado del DVA y un cuestionario sobre su conocimiento y aceptación. Se recogió su punto de vista sobre diversos aspectos relacionados con el fin de la vida.
La encuesta se realizó en siete unidades de diálisis hospitalarias con un total de 416 pacientes en diálisis en activo. El cuestionario se entregó a 265 pacientes, 154 contestaron la encuesta, el 69,2% respondió sin ayuda. El grado de implantación del DVA era muy bajo (7,9%) y también la designación de representante (6,6%). Los pacientes tenían una idea muy clara sobre sus deseos ante situaciones como coma irresoluble, estado vegetativo, demencia irreversible y enfermedad grave no tratable y más de un 65% no deseaban que se les aplicaran ventilación mecánica, alimentación por sonda, diálisis o maniobras de resucitación en caso de parada cardiorrespiratoria. Muchos opinaron que el DVA podría hacerse antes de comenzar el tratamiento de diálisis, pero la mayoría consideró que sólo debería ofrecerse a aquellas personas que lo pidieran (el 65 frente al 34%).
En conclusión, los pacientes en diálisis tienen una postura bastante definida ante diversas situaciones asociadas con el fin de la vida, sin embargo esta voluntad no está reflejada documentalmente debido a la escasa implantación de los DVA.
INTRODUCTION
In spite of social and legislative initiatives for promoting personal autonomy in the realm of personal decisions regarding health, few advances have been made in recent years in the implementation of planning processes for end-of-life care. Very few health centres have developed an advanced care planning programme, and the percentage of patients that establish their final wishes, their position on cardiopulmonary resuscitation, or that have named a representative in case incapacitation is very low, with no substantial improvements in recent years.1-3
Advanced care planning (ACP) involves the development of a process that integrates information, communication, reflection, and decision-making, taking into consideration the cultural characteristics of the patient.4 ACP requires joint participation on the part of doctors, patients, family members, and, in the case of patient incapacity, a legal representative. The patient must understand the characteristics of his/her disease, the available treatment options, the prognosis, the consequences of refusing treatment, and the possibility of conservative or experimental treatments and palliative care. If all of this information is not shared and discussed, it is very difficult for the patient to make a correct decision.5 Composing an advance directive document (ADD) can be an important resource in many patients, such as those incapable of making decisions, those in which the start of dialysis is questioned, permanently unconscious patients, with severe and irreversible dementia, those incapable of cooperating with dialysis treatment or relating to others, with a short life expectancy due to terminal disease or end-stage pulmonary, liver, or heart disease, confined to their beds and requiring assistance for daily activity.6 The decisions made must be reflected in the patient’s clinical report and should be periodically reviewed and either confirmed or changed accordingly.7-9
In the American registry, between 15% and 25% of deaths in patients on dialysis are produced by removal from dialysis, this being the second cause of death,10 and only 6%-51% of patients have an ADD.11 In Spain, we have very little knowledge regarding the percentage of patients that die due to removal or refusal of dialysis treatment.12 We do have access to the data from the DOPPS study, in which 0.6% of patients indicated that they did not want cardiopulmonary resuscitation, and 0.3 out of 100 patients/year are removed from haemodialysis treatment. These values clearly do not reflect the current situation in our dialysis units.13 In the registry maintained by the Spanish Society of Nephrology (S.E.N.) from 2009 (unpublished data), 6.24% of patients died due to a psychological-social cause that led to withdrawal from treatment.
A study was performed in 2007 at the Parc Taulí Hospital that constituted the first discussion of advance directives (AD) in our field of Spanish medicine.14 This study only reflected the current situation at one hospital in Catalonia, and still the reality in other health centres from other regions is unknown, and still we need to know the opinion of our patients regarding these important life questions. We health professionals need to know what are the values and wishes of our patients in order to be able to make respectful decisions.
With this objective, we developed a questionnaire to survey the various aspects of implementing an ADD and the values and wishes of patients in various nephrology services. Although this was a single gathering of information, we believe that our results reflect the current reality and should be disseminated among the health care professionals charged with the care of these patients. This study provides an overview in which one can observe that our patients have very clear opinions regarding fundamental life questions, but these are not adequately reflected in clinical histories.
This study involved several objectives. First and foremost: to investigate the level of patient familiarity with the ADD and what percentage of patients had composed the document or had named a legal representative verbally or in written form. Second: using the information obtained, to determine the demand for and acceptance of the implementation of an AD protocol in dialysis units. Third: to determine dialysis patient opinion on undergoing various type of treatment in the event of extreme health situations when they are incapable of making decisions. Finally, to analyse how the patient clinical situation, age, sex, time on dialysis, autonomy, capacity, family situation, and level of education all affect patient opinion regarding the ADD and patient attitudes regarding end-of-life care.
PATIENTS AND METHOD
We surveyed patients with stage V chronic kidney disease that were actively undergoing a dialysis programme (haemodialysis, peritoneal dialysis, or home haemodialysis) who were selected at hospitals or peripheral dialysis units. Hospitals were asked by the S.E.N. to participate through a corporate mail with an offer for participation sent to all member health centres. The necessary documents were sent to the interested hospitals. The survey was provided to the patients by the attending nephrologist.
These documents consisted of three separate parts.
1. Document I contained information explaining the nature and significance of the advance directive (Appendix 1). We highlighted the intention of making the ADD part of a complete process of information, participation, and continuous and updated decision-making in which patients and their families would participate. This process is known as advanced care planning. Composing an ADD, along with the process of informing and reflecting on the possible options and consequences, provides the opportunity to learn the values and wishes of the patient so as to be able to influence the future decisions he/she makes, while still respecting and facilitating patient autonomy. This document also explained the legal backing of ADD (Law 41/2002), patient rights to autonomy, health information, and clinical documentation. This law is in accordance with the ninth article of the Convention on Human Rights and Biomedicine of the Council of Europe, signed in Oviedo in 1997. The patient also received information regarding the procedure for formalising an ADD: content, legal requirements, and proceedings.
2. Document II was a questionnaire on familiarity with and approval of the ADD in patients on a dialysis programme and patient opinion regarding concrete situations that may necessitate making life decisions (Appendix 2). This questionnaire consisted of 14 questions (divided into several sections) which were answered as a yes, no, or no answer. The first group of questions explored patient familiarity with the ADD and formalisation level, level of communication with family members regarding end-of-life decisions, and the designation of a legal representative. This was followed by questions regarding the hypothetical wishes of the patient regarding medial decisions (mechanical ventilation, tube feeding, dialysis, and cardiopulmonary resuscitation) in the case of irreversible coma, permanent vegetative state, irreversible dementia, or severe untreatable illness. The final section of questions was directed towards the patient’s desire to compose an ADD, under what circumstances, and if all dialysis patients should be offered the opportunity to do so and when. We also asked if the patient had filled out the survey alone or if help was given.
3. Document III was a set of questions designed to evaluate the general situation and physical state of the patient at the time of responding the questionnaire, along with data regarding age, sex, time on dialysis and what type, and level of education (Appendix 3).
4. Finally, document IV was directed towards the attending nephrologists, and asked the number of patients that received dialysis at each unit, whether this treatment was given in a hospital or other setting, how many patients had been given the questionnaire, and how many had filled it out.
Statistical analysis
With the objective of using the responses from questions regarding patient desires for medical decisions, we decided to establish a scoring system that would allow for classifying patients into three categories: patients that desired limits to treatment efforts, patients that did not desire limitations, and patients that did not express their desires clearly. We quantified the reliability of this classification using Cronbach’s alpha (0.835). We then examined the relationship between the three categories of patient wishes and quantitative variables using ANOVAs, and with qualitative variables using chi-square tests. We used means and standard deviations for summarising quantitative variables, and proportions for qualitative variables.
We analysed all surveys in a central database using R software.
RESULTS
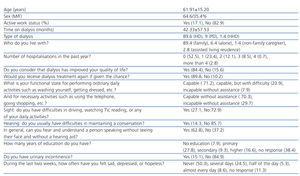
We performed the survey during the second quarter of 2010 at seven different hospital dialysis units that served a total of 416 active dialysis patients. The questionnaire was administered to 265 patients: 154 of them filled it out (58.11%) and 69.2% indicated that they had responded the questions without help. Patient characteristics at the time of the survey are summarised in Table 1. The patients surveyed had a mean age of 61.91±15.20 years, were mostly men (64.5±35.4%), not actively employed (82.1% vs 17.1%), and mean time on the dialysis programme of 42.33±57.53 months. The representation of each type of dialysis within the study sample was similar to the proportions recorded in the S.E.N. registry (89.6% on haemodialysis, 9% on peritoneal dialysis, and 1.4% on home haemodialysis). The majority of patients lived with their families (88%), 6.3% lived alone, 1.4% lived with a non-family caregiver, and 2.8% lived in assisted living residencies. These patients had a high rate of comorbidity and were frequently hospitalised (23.4% had been hospitalised once, 12.1% twice, 8.5% three times, and 0.7% four times within the last year). The level of patient autonomy in performing everyday activities was limited: 20.9% carried out daily activities with difficulty, and 7.9% required assistance. The same was true for activities necessary for daily functioning (using the telephone, grocery shopping, cooking, cleaning, etc.): 29.7% were incapable of carrying out these activities without assistance. A high rate of patients had visual and auditory deficits that were not ameliorated using glasses (27.1%) or that required hearing aids (37%). Only 15.1% of patients had urinary incontinence, although this result is not particularly relevant in patients with chronic kidney disease (CKD) on long-term dialysis treatment, as they probably have little residual diuresis. The patients resisted answering questions regarding their level of education, and 38% did not respond to this question. The patients had a positive perception of their time on renal replacement therapy, and considered that dialysis had improved their quality of life (84.4% vs 15.6%). Also, 89.1% affirmed that they would undergo dialysis treatment again if necessary. An interesting result was the high rate of patients that professed symptoms of sadness, depression, and loss of hope. The patients also indicated that they had felt depressed at some point for several days (27.4%), more than half of the day (5.9%), or almost every day (9.6%).
The percentage of patients that had an ADD was very low (7.9%), and even fewer patients had formalised a document in front of a notary (5.3%) or considered that they had expressed their wishes in front of witnesses (6.6%). A higher percentage of patients (60.9%) indicated that they had empowered another person to represent their wishes in the case of loss of ability for communication, and 40% of patients had given this person the capacity for making decisions. The patients surveyed also indicated that they had a close relationship with the person that represented them and that this representative had a good understanding of their wishes (70%). This person was the patient’s partner in 58% of cases, and another family member in 38.8%. The patients expressed little trust in delegating this responsibility to other people in their lives such as doctors, friends, priests, etc.
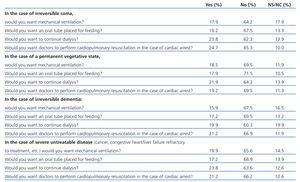
A large percentage of patients had expressed their wishes regarding the measures to be taken in the case of a permanent coma that would require assisted ventilation (40%) in a verbal statement to their representative. The patients had a very clear idea regarding their wishes in situations such as irreversible coma and vegetative state, and over 65% did not wish to undergo mechanical ventilation, tube feeding, continued dialysis treatment, or resuscitation in the case of cardiac arrest (Table 2). The same desires were expressed in the case of irreversible dementia and severe, untreatable disease, which are situations in which most patients desired limited and only non-aggressive treatment. By analysing the patient opinion variable, grouping those individuals with the same response to two or more questions (Table 3), we observed that none of the following independent variables: demographic characteristics, social/work status, the type of or time spent on dialysis, the level of comorbidity as measured by the number of hospitalisations in the past year, or the presence of depression, the level of education had any effect on this variable. We only observed a correlation with visual deficit (P<.006), auditory deficit (P<.006), and the presence of urinary incontinence (P<.01). This reflects a high level of concordance among responses, which were quite uniform and independent of the patient’s situation at the time of the survey.
In spite of the fact that the majority of patients were very clear as to their wishes, the expression of these desires in a written document was very rare. When the patients were asked if they would like to compose an ADD, half said yes (54%), but 43.7% said no. The same proportion of patients considered that an ADD should be composed before starting dialysis treatment (51.6% vs 48.4%), although the majority also considered that this option should only be offered to patients that ask for it (65% vs 34%).
DISCUSSION
In spite of legislative efforts and Societies’ bioethics initiatives for establishing a legal and cultural framework in Spain that would facilitate the implementation of ADD, the level of familiarity with and dissemination of AD is very limited in the general population. The existence of hospital protocols for facilitating patient decision-making regarding end-of-life procedures would be useful for patients and at the same time would help health professionals and family members in making correct decisions.
ACP not only implies composing an ADD, but also the implementation of a more complex process that requires active participation on the part of patients and family members after receiving sufficient training and information for making the right decisions. This process should have a defined methodology and objectives, and be actively supported by the entire staff responsible for attending to the patient at the health institution (including health and non-health workers). We are not surprised by the scarce familiarity with the ADD in our patients, since this trend is visible in the general population and is exacerbated by the lack of ACP.
In spite of the lack of a written AD, many patients indicated in the survey that they had maintained conversations with close ones regarding aspects of end-of-life care (generally close family). However, in most cases, these desires are not clearly explicit, have not been specifically expressed, and a representative for the patient has not been appointed. This situation is clearly appreciable in normal clinical practice when decisions regarding end-of-life care fall upon a family member that feels impelled to decide for an incapacitated family member without having a clear notion of the patient’s desires, and without a designated representative that has been conferred this responsibility in an AD.
In spite of the lack of AD documentation, our patients have a clear idea of their wishes and expectations, as well as their position regarding certain life-threatening situations in end-of-life care. In the survey, most patients expressed their wish not to receive aggressive medical treatment in the case of severe incurable disease or when incapable of making decisions. The existence of an ADD is important for incompetent patients, and it is more probable that patients that have expressed their desires in written form have their final wishes respected (96.2% vs 1.9%).15,16
Although patients generally appreciated their dialysis treatment and did not regret having started renal replacement therapy, they were clear that they did not want to continue receiving dialysis regardless of the situation. These results contrast with those from Davidson in Canada,17 which indicated that 61% of patients regretted having started dialysis and that they started treatment because of the desires of their doctors and family members rather than for personal wishes. Moreover, less than 10% stated that they had discussed end-of-life care with their nephrologist in the last 12 months. The Spanish law of patient autonomy clearly states that the patient’s wishes must be respected, both regarding the choice of treatment and the option to modify or suspend treatment. Survey results show that many daily clinical practice situations could be simplified or optimised if the patient’s desires were clearly explicit.
We cannot underestimate that there is certain level of resistance to composing an ADD, possibly due to unfamiliarity, but also due to distrust of the consequences. There may be suspicion that doctors would show less interest or would not provide necessary and effective treatments if a previous written document established limitations to the treatment that the patient wants to receive. This is one aspect that would be clearly improved by the implementation of a regulated ACP. Even so, we must still respect the desires of patients that do not want to be informed or express their wishes for end-of-life care, and the survey shows that there are discrepancies in patient opinion as to when it is appropriate to compose an ADD. The vast majority of patients considered that it should only be offered to those that expressly ask for it.
Patient opinion regarding limiting the care they will receive is sometimes determined by the patient’s values, previous experiences and testimonies, and the personal expectations for suffering and quality of life. Since all of these factors influence patient decisions, each individual is unique in his/her expectations and motivations, and so we cannot establish any patterns for defining types of patients, nor demographic or comorbidity variables that are associated with a given position. In a previous study performed in Catalonia,13 older patients were more prone to requesting limitations to treatment, but there were no differences observed based on sex, comorbidity, level of education, language, or underlying nephropathy. Other authors have described a greater percentage of do not resuscitate orders in some groups (elderly, institutionalised, and higher comorbidity patients),12 and in patients of different race.3 In our patients, we only observed a slight tendency to limit care in patients with greater sensory deficit, but no correlations were observed with comorbidity. Although a high percentage of patients indicated depressive tendencies, they were not more frequent among the most severe patients (measured as the number of hospitalisations in the past year) or with the length of time on dialysis, which was considered favourably by most patients. The presence of depressive tendencies was not associated with a more favourable position towards limited care either.
In conclusion, the awareness and implementation of the ADD is very limited in our dialysis units, which indicates the need to establish ACP protocols. Our patients, in spite of not having explicitly written out their wishes, were very clear with regard to the use of aggressive treatment methods for end-of-life care. Nephrology departments must develop abilities and protocols for training and informing all parties involved in this process, as well as collecting and storing the information regarding the last will of patients. As such, for those patients that desire it, we may facilitate the making of correct decisions that respect the patient’s wishes in the case of loss of autonomy.
Acknowledgements
We would like to thank Francisco Rodriguez Salvanés and Lorena Vega Piris at the methodology unit of the research institute of the Hospital Universitario de la Princesa for their assistance in the statistical analysis of the data.
Table 1. Patient characteristics at the moment of the survey
Table 2. Opinions on interventional therapies for certain pathologies
Table 3. Relationships between patient characteristics and response variables