A good function of vascular access is essential to achieve effective dialysis. Periodic determination of the blood flow (BF) of the arteriovenous fistula (AVF) is the best method to assess the function the vascular access.1 There are numerous articles in the literature that analyze the impact of demographic characteristics of patients on the prevalence of AVF,2–4 however there are few that evaluate factors that could affect the blood flow and in those published, the results are not conclusive. The location of the AVF and diabetes mellitus have been reported as the main factors affecting the function of the AVF. Others, such as age, gender, blood pressure, associated cardiovascular comorbidity, etc., may affect the function of the AVF but not in a significant manner.5,6 We have searched different analytical parameters that may be related to BF of the AVF of young patients; we only found in a published article a relationship of BF with the PTH levels, in such a way that higher levels of PTH were observed in patients with higher BF. Medications except those related to coagulation, do not seem to affect the BF of the AVF.7
Most patients on dialysis have a positive phosphorus balance, so they will need additional treatment with binders to avoid hyperphosphatemia.8
The objective of our study was to assess which factors influence the function of the vascular access estimated by flow measurement by dilution with saline using ultrasound (Transonic monitor). We analyzed 132 patients in a chronic hemodialysis program. The variables studied were the following: demographic (age, sex, body mass index), associated comorbidity (hypertension, diabetes mellitus, ischemic heart disease, heart failure, peripheral vascular disease), those related to vascular access (type and BF of AVF), analytical data (anemia and calcium-phosphorus metabolism) and treatment (antihypertensive medication, erythropoietin stimulating agents, statins, binders, vitamin D, etc.), all at the time of the last BF measurement of the AVF. We divided the population into 2 groups: patients with BF<600ml/min and patients with BF>600ml/min.
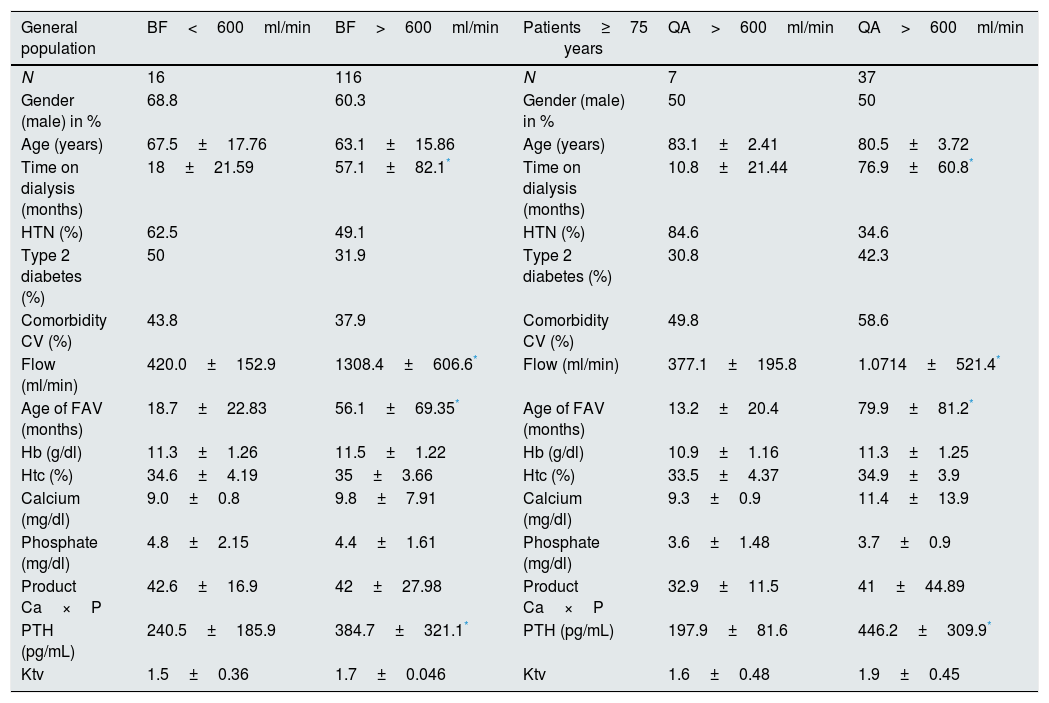
Of the total population, 61% were male, with an average age of 64.6 years; 124 patients had autologous and 8 prosthetic AVF; 116 (88%) had BF>600 and 16 (12%) BF<600ml/min. It should be noted that those with QA<600 had a lower PTH and with a higher percent of patients on calcium containing phosphate binders. The years of AVF in place were moderate, as it was the time on dialysis. In the rest of the variables studied, statistically significant differences were not observed (Table 1). In the multivariate analysis, (1) the dose of calcium binder (OR: 3.31, p<0.05) and (2) the age of the AVF were determinant (Table 1) (OR: 0.97, p<0.05) (Fig. 1).
Comparison of the variables analyzed in the general population and in the population over 75 years of age.
| General population | BF<600ml/min | BF>600ml/min | Patients≥75 years | QA>600ml/min | QA>600ml/min |
|---|---|---|---|---|---|
| N | 16 | 116 | N | 7 | 37 |
| Gender (male) in % | 68.8 | 60.3 | Gender (male) in % | 50 | 50 |
| Age (years) | 67.5±17.76 | 63.1±15.86 | Age (years) | 83.1±2.41 | 80.5±3.72 |
| Time on dialysis (months) | 18±21.59 | 57.1±82.1* | Time on dialysis (months) | 10.8±21.44 | 76.9±60.8* |
| HTN (%) | 62.5 | 49.1 | HTN (%) | 84.6 | 34.6 |
| Type 2 diabetes (%) | 50 | 31.9 | Type 2 diabetes (%) | 30.8 | 42.3 |
| Comorbidity CV (%) | 43.8 | 37.9 | Comorbidity CV (%) | 49.8 | 58.6 |
| Flow (ml/min) | 420.0±152.9 | 1308.4±606.6* | Flow (ml/min) | 377.1±195.8 | 1.0714±521.4* |
| Age of FAV (months) | 18.7±22.83 | 56.1±69.35* | Age of FAV (months) | 13.2±20.4 | 79.9±81.2* |
| Hb (g/dl) | 11.3±1.26 | 11.5±1.22 | Hb (g/dl) | 10.9±1.16 | 11.3±1.25 |
| Htc (%) | 34.6±4.19 | 35±3.66 | Htc (%) | 33.5±4.37 | 34.9±3.9 |
| Calcium (mg/dl) | 9.0±0.8 | 9.8±7.91 | Calcium (mg/dl) | 9.3±0.9 | 11.4±13.9 |
| Phosphate (mg/dl) | 4.8±2.15 | 4.4±1.61 | Phosphate (mg/dl) | 3.6±1.48 | 3.7±0.9 |
| Product Ca×P | 42.6±16.9 | 42±27.98 | Product Ca×P | 32.9±11.5 | 41±44.89 |
| PTH (pg/mL) | 240.5±185.9 | 384.7±321.1* | PTH (pg/mL) | 197.9±81.6 | 446.2±309.9* |
| Ktv | 1.5±0.36 | 1.7±0.046 | Ktv | 1.6±0.48 | 1.9±0.45 |
Both in the general population and in patients >75 years, the time in dialysis, the flow and age of the AVF, as well as the PTH levels, were higher (p<0.05) in AVF with BF>600ml/min vs <600ml/min. The difference between PTH levels is more pronounced in the population >75 years old. Serum calcium levels were higher in the subgroup of AVF with BF>600ml/min, without reaching statistical significance. No statistical differences were observed in the rest of the parameters analyzed.
Medication analyzed: ESA, ACE inhibitors, statins, antiaggregants, anticoagulants, sevelamer, calcium containing phosphate binders, cinacalcet, lanthanum.
The intake of calcium containing phosphate binders was greater in patients with QA-C <600ml/min than >600ml/min. These differences are accentuated in the subgroup of patients aged >75 years. In the rest of the medication analyzed no significant differences were found.
ESA: erythropoietin stimulating agents; ACE inhibitors: angiotensin-converting enzyme inhibitors; Lanthanum: lanthanum carbonate.
The study was repeated including only patients older than 75 years obtaining the same results as in the general population: time on dialysis, age of the AVF and lower PTH levels in those patients with AVF of BF<600/ml/min and in this patients, the high percentage on calcium containing phosphate binders was remarkable (85.7%). The rest of the variables studied were not significant (Table 1). By multivariate analysis, in this population the dose of calcium containing phosphate binders was the only determinant of having low BF in the (OR: 34.8, p<0.05) (Fig. 1).
The literature is scarce in terms of articles that relate the BF of the AVF with the patient's medication,7 even more so when it comes to relating BF and phosphate binders. There are studies that show an improvement in survival in dialysis patients treated with non-calcium binders as compared with calcium containing phosphate binders9; although other studies restrict the improvement of survival patients over 65 years of age.10 Based on the results obtained in our study, we can conclude that treatment with phosphate binders containing calcium could have a negative effect on the function of AVF as shown by a low BF. This effect seems to be more evident in patients older than 75 years, which should lead us to evaluate whether it is appropriate the use of calcium containing phosphate binders in this population.
Please cite this article as: Merino García E, García Cortés MJ, Biechy Baldán MM, Ortega Anguiano S, Polaina Rusillo M, Sánchez Perales MC. Valoración del flujo de la fístula arteriovenosa en pacientes en tratamiento con quelantes con calcio. Nefrologia. 2018;38:321–323.