Antecedentes: Existe información insuficiente sobre los factores que influyen en las pérdidas proteicas peritoneales (PPP) durante el tratamiento con diálisis peritoneal (DP). En particular, se desconoce el efecto que la modalidad de DP y otras condiciones de prescripción pueden tener sobre esta variable. Método: Siguiendo un diseño prospectivo y observacional, analizamos el efecto de las condiciones de prescripción de DP sobre las PPP en 24 horas (variable principal) en una cohorte de pacientes incidentes en DP. La estrategia de análisis incluyó análisis estadístico mediante modelos mixtos multinivel y estimaciones estandarizadas del transporte proteico peritoneal durante pruebas de equilibrio peritoneal seriadas, con el fin de ajustar para desigualdades en las características de las poblaciones manejadas con diferentes pautas de prescripción. Resultados: Estudiamos 284 pacientes, 197 en DP continua ambulatoria (DPCA) y 87 en DP automática (DPA) al inicio de seguimiento. Ambos grupos mostraron diferencias significativas en sus características clínicas y de función peritoneal. Las estimaciones seriadas de las PP de 24 horas mostraron valores marginalmente más altos en DPCA, permaneciendo esencialmente estables durante el seguimiento. El análisis multivariante identificó a la DPCA (B = 888,5 mg, intervalo de confianza 95%: 327,5/1448,6), el volumen total de dializado infundido (B = 275,9 mg/l, 153,9/397,9) y la ultrafiltración diaria (B = 0,41 mg/ml, 0,02/0,80) como predictores independientes de las PPP de 24 horas. El modelo también mostró tendencia a disminución en las PPP con el tiempo en DP. Conclusiones: Las características individuales de transporte peritoneal de proteínas son el principal determinante de las PPP en 24 horas. La pauta de cambios largos (DPCA) asocia mayores PPP que la de cambios cortos (DPA), aunque esta diferencia se compensa en la práctica por la correlación positiva entre PPP y volumen infundido. Ultrafiltración y tiempo en diálisis son predictores secundarios de PPP en 24 horas.
Background: There is a deficit of information regarding the factors that influence peritoneal protein excretion (PPE) during PD therapy. In particular, the effects of the modality of PD and other conditions of the dialysis prescription remain unclear. Method: This prospective, observational study analysed the effects of prescription characteristics on 24-hour PPE (study variable) in a cohort of patients starting PD. Our statistical analysis included a multi-level mixed model and standardised estimations of peritoneal protein transport during serial four-hour peritoneal equilibrium tests in order to control for disparities in the characteristics of patients managed on different regimens. Results: We evaluated 284 patients, 197 on CAPD and 87 on automated PD (APD), at the start of PD treatment. The two groups differed in terms of clinical characteristics and peritoneal function. Univariate, serial estimates of 24-hour PPE were marginally higher in CAPD patients, and remained essentially stable over time in both groups. Multivariate analyses identified CAPD (B=888.5mg, 95% CI: 327.5/1448.6), total dialysate volume infused per day (B=275.9mg/Ll; 153.9/397.9) and ultrafiltration (B=0.41mg/mL; 0.02/0.80) as independent predictors of 24-hour PPE. The model also revealed a minor trend for a lower 24-hour PPE as time on PD increases. Conclusions: The individual characteristics of peritoneal protein transport are the major determinants of 24-hour PPE. The use of CAPD as the dialysis modality is associated with higher PPE rates than the APD technique, although this difference is counterbalanced by a direct correlation between PPE and the volume of dialysate infused per day. Ultrafiltration and time on dialysis also act as minor independent predictors of PPE during PD therapy.
INTRODUCTION
Peritoneal protein excretion (PPE) is an undesired consequence of peritoneal dialysis (PD) that contributes to a varying degree to malnutrition1 and other complications inherent to this technique.2-4 Scarce information is available regarding the factors that affect the magnitude of PPE in daily clinical practice, apart from the expected correlation with general peritoneal transport characteristics.5-8 It is unclear what sort of effect the conditions of the dialysis prescription, and the modality of PD in particular, have on this parameter. Previous attempts to clarify this issue have been limited by the notable disparities between the populations compared. The type of peritoneal transport will also influence the prescription provided, including the decision between continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis (APD). Stratified multivariate analysis techniques aid in adjusting for these variables, but the use of peritoneal creatinine transport for this purpose is inadequate, since this variable provides little predictive value for peritoneal protein transport.9,10
We present the results of an observational study involving a large cohort of incident patients on PD, with the primary objective of establishing the influence of prescription characteristics (including modality of PD) on PPE during a 24-hour period, taking advantage of the standardised measurements of peritoneal protein transport taken during serial peritoneal equilibrium tests (PET).
POPULATION AND METHOD
Study design
Ours was a prospective and observational study examining a cohort of incident patients on PD treated at our hospital between January 2000 and June 2010. The inclusion criteria used were: minimum of two months on dialysis treatment with no registered cases of peritonitis and availability of initial 24-hour PPE measurements and during the first PET. The primary study variable was the magnitude of PPE in PD effluent during a 24-hour period. The primary adjustment variable was an estimate of peritoneal protein transport during a standard PET using a 2.27% glucose solution. We also examined standard demographic, clinical, and laboratory parameters in order to obtain adjusted estimates.
At our hospital, traditional PD solutions were used until May 2008. After this point, all patients were treated using solutions with low concentrations of glucose degradation products.
The study protocol was in accordance with the ethical criteria required for observational studies at our hospital as well as the Helsinki Declaration.
Laboratory methods and secondary calculations
Blood levels of haemoglobin, glucose, urea, creatinine, albumin, and cholesterol were estimated using a standard auto-analyser. Glucose and creatinine levels in the dialysate fluid and urea and creatinine levels in urine samples were measured using procedures specifically designed for the same auto-analyser. Plasma C-reactive protein (CRP) was measured using an immunoturbidimetric test (Roche Diag., Mannheim, Germany). We also used a modified colorimetric test (pirogalol red) to measure total protein content of urine samples and peritoneal effluent. In a previous study,10 we showed this to be an appropriate technique that is not affected by sample storage or by high concentrations of glucose present in the dialysate.
We used universally accepted procedures for performing PET. Glomerular filtration rate was estimated as the mean 24-hour clearance rates of urea and creatinine. Mean daily ultrafiltration rate (UF) and blood pressure were compiled from the registries of daily values recorded by the patients themselves.
Strategy of analysis
We compared the temporal progression of 24-hour PPE between patients treated with CAPD and those treated with APD until the end of the second year of follow-up, using both strategies of intention to treat and final treatment. Results were similar under both approaches, and the results presented in this article are derived from final treatment strategies. We also monitored longitudinal differences in demographic and clinical parameters, peritoneal function, prescription, and optimisation of treatment, searching for univariate correlations with 24-hour PPE. However, our primary objective was to analyse how the conditions of peritoneal dialysis prescriptions affected the primary study variable, taking into account possible temporal variation in PPE and the change produced to the PD prescription (including the modality of dialysis) during the follow-up period.
Statistical analysis
Numerical variables are presented as mean ± standard deviation or median and range, as appropriate. Univariate comparisons were performed using Student’s t-test, ANOVA, and Mann-Whitney and Wilcoxon tests (numerical variables) and chi-square distribution (categorical variables). We also calculated correlations between numerical variables using Spearman’s test. We used a generalised linear model with repeated measures to analyse univariate tendencies over time, both for 24-hour PPE and for PPE during serial PETs.
We also performed a multivariate analysis using multi-level mixed linear models, selecting variables using forwards stepwise selection. The effect of patient heterogeneity was adjusted for as a random effect, while the covariates analysed were adjusted for as fixed effects. Serial measurements of PPE during PET, which represented the individual characteristics of peritoneal protein transport over time, were included systematically in all models tested. We also analysed the potential effects of cardiovascular events (only those that required hospitalisation) and peritonitis during the follow-up period, as well as for the potential effects of treatment with angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARB) on the progression of PPE over time. Associations between the study variables and PPE were estimated using beta coefficients (with 95% confidence intervals [CI]) in the fixed effects section of the statistical models. We also analysed interaction terms. Finally, we used Bayesian (BIC) and Akaike’s information criteria (AIC) to compare maximum likelihood models.
We used SPSS (v.18.0) and Stat (v.11) statistical software for all statistical analyses.
RESULTS
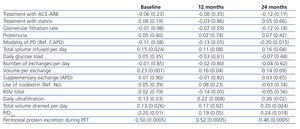
Of the 313 patients evaluated, 284 complied with the study inclusion criteria. Table 1 summarises the general characteristics of the study population at the start of PD. Fifteen patients (5.3%) suffered at least one cardiovascular event during the first 6 months, 24 (8.5%) between months 6 and 12, and 49 (17.3%) during the second year of the follow-up regimen. The cumulative incidences of peritonitis were 59 (20.8%), 45 (15.8%), and 26 (9.2%), respectively. Table 2 demonstrates the parameters for prescription and treatment optimisation compiled during the follow-up period. Only two patients had dry-day regimens at the start of PD, and four others were prescribed dry days at some other point during follow-up. The majority of the differences observed were expected, but surprisingly, PPE during serial PETs was consistently higher in patients on CAPD, while small solute transport (P/D creatinine at 4 hours [P/Dcrea]) was higher in patients treated with APD, although this difference was only significant in baseline measurements (Table 2).
Changes in the type of PD administered were relatively common, and involved switching from CAPD to APD in 43 cases and switching from APD to CAPD in 4. Table 3 shows the primary univariate correlations between 24-hour PPE and variables of treatment optimisation and prescription. The primary study variable was also significantly correlated with baseline Charlson comorbidity index (r=0.16; P=.006) and CRP (r=0.15; P=.014). Univariate analyses based on intention to treat and based on final treatment (Table 2, Figure 1) tended towards higher 24-hour PPE in patients on CAPD, although the difference only reached statistical significance after 24 months. On the other hand, univariate analyses with repeated measures showed no significant long-term changes for PPE during PET or in a 24-hour period, neither in the overall group nor based on modality of PD or the presence/absence of peritonitis during the first year of follow-up.
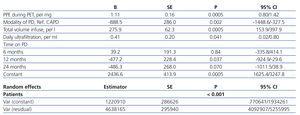
The multi-level mixed models (Table 4) identified CAPD (vs. APD), total volume infused in 24 hours, and daily UF as independent predictors of 24-hour PPE, after adjusting for standardised peritoneal protein transport (PPT). Total volume drained acted in the models as a surrogate for infused volume and UF (B=297.9; 95% CI: 203.6/292.3; P<.0005). All variables included in the final model had a significant impact on both AIC and BIC with the exception of daily UF, suggesting that this variable has little practical influence on 24-hour PPE. We detected no significant interaction terms between the variables in the final model except for a minor interaction between PPE during PET and total volume infused (B=-0.18; 95% CI: -0.6/-0.01; P=.039), which we ignored in order to give greater clarity to the presentation of our results. No other variables related to clinical results, optimisation of treatment, or prescription (Table 3) were independently correlated with 24-hour PPE. In particular, cardiovascular events (B=-149.9; 95% CI: -969.5/669.7; P=.72), peritonitis (B=389.0; 95% CI: -117.6/895.7; P=.13), and treatment with ACE/ARB (B=-17.6; 95% CI: 443.2/407.9; P=.94) all failed to show a time-dependent correlation with 24-hour PPE.
The multivariate analysis showed tendencies towards decreased PPE during follow-up, although this effect only reached statistical significance after 12 months (Table 4). We performed a stratified statistical analysis in order to rule out the possibility that this effect might be the consequence of an earlier exit from PD in patients with a greater rate of 24-hour PPE. The analysis showed slight and non-significant tendencies towards increased rates of late exit from PD (24 months) in patients in the first and fourth quartile of PPE results taken during PET.
DISCUSSION
PPE is correlated with general characteristics of peritoneal transport in each individual. However, the use of estimators of small solute transport as a marker for proteins is quite unreliable, since despite the fact that the correlation between PPE and P/Dcrea is statistically significant, it is far from being unequivocal.9,10 This limitation is logical, given the fact that different pathways are used for peritoneal transport of proteins and of small solutes.11 If we wish to perform an adjusted evaluation of the effect of other factors on 24-hour PPE, there is no specific marker available for the characteristics of peritoneal protein transport. In previous studies, we showed that a standardised estimate of protein transport during PET is useful for this objective.10,12
Several studies have explored the possibility of using common demographic and clinical markers of peritoneal protein transport in patients on PD. Advanced age, diabetes, cardiovascular comorbidity factors, obesity/overweight, residual renal function, proteinuria, and plasma CRP are some of the most frequently cited factors.8-14 A comprehensive evaluation suggests that PPE is associated with cardiovascular disease, supporting the hypothesis that this serves as a marker for large peritoneal pore disorders, and indirectly, for endothelial dysfunction.15,16 In fact, some studies have demonstrated an association between PPE at the start of PD and mortality while on PD.9,12 In our study, we observed a univariate association between PPE and Charlson comorbidity index and plasma CRP, although the correlation disappears after adjusting for peritoneal protein transport during PET.
Very few studies have examined the influence of the conditions of the PD prescription on 24-hour PPE. Kathuria et al.5 compared PPE in patients treated with CAPD and nocturnal intermittent PD (NIPD), observing no consistent differences between the two modalities, even after stratifying patients based on peritoneal transport of small molecules (P/Dcrea). On the other hand, Heaf et al.15 observed lower PPE values during NIPD than in patients on APD with wet day. In a smaller study, Westra et al.17 observed relatively high levels of PPE in nine patients treated with APD. Both an increase in the number of cycles administered and a longer duration of treatment appear to be associated with higher PPE.17 However, the design of this study, which lacked a control group on CAPD, does not allow for drawing clear conclusions based on these results.
In our study, patients on CAPD had different peritoneal protein transport characteristics (estimated during serial PETs) than patients on APD (Table 2). This difference alone could explain why the simple analysis of 24-hour PPE showed the tendency for higher levels in patients on CAPD than in those on APD (Table 2). On the other hand, the univariate tests for repeated measures detected a notable stability in PPE during PET and as measured over 24 hours, which is in agreement with the results from previous studies.8 The multi-level mixed models (Table 4) showed that the conditions of the prescription of PD can also influence 24-hour PPE. Both total infusion volume and daily UF were directly and independently correlated with the primary study variable. UF can be considered as a simple complementary metric to infused volume, but the possibility of a specific effect of this variable on peritoneal protein transport is a controversial subject. Recent authors have shown a direct correlation between these two variables,8,10 whereas a previous study by Waniewski et al.18 showed that UF can be directly and inversely correlated with PPE, depending on the category of peritoneal transport that the patient falls under, with practically neutral effects when analysing the total population treated with PD. The lack of a significant impact of UF on AIC and BIC in the multivariate analysis suggests scarce clinical relevance for this variable.
The use of CAPD was associated with higher 24-hour PPE values than APD, after adjusting for the characteristics of peritoneal protein transport (PET) and total volume infused. The significance of this finding is unclear, and we cannot rule out that it is the product of a residual bias derived from an incomplete adjustment for other factors in the analysis. The use of APD, based on shorter and more frequent cycles, could be the cause of slightly but significantly lower PPE values, given the accumulation of infusion and drainage times. The impact of this factor should not be so important if we assume that peritoneal protein transport is linear during exchanges, in contrast to the pattern of small solute transport.19 We should also point out that other studies have suggested that peritoneal protein excretion could be faster during the first hour of dialysis18 and then assume a linear pattern as the session progresses. If this were true, we might even expect greater PPE in the short exchanges typical of APD. However, this phenomenon is probably the result of both the mixture of residual volume, which is rich in proteins, with the recently infused dialysate, and the phenomenon of proteins being drawn from the interstitial space into the peritoneal cavity during the early stage of each exchange. Either of these effects could be relevant during long-duration dialysis sessions (such as those performed in CAPD), but only during the first of a series of short exchanges (such as in APD).
Our study did involve certain limitations, including a non-randomised assignment of patients to the different modalities of PD. In addition, a portion of our study patients switched PD modalities during the follow-up period, mostly from CAPD to APD, and membrane dysfunction could prompt some of these changes. The multivariate strategy and time-dependent statistical analysis were designed to compensate for these potential biases. In addition, our hospital does not routinely administer NIPD, which impedes our ability to draw valid conclusions with respect to this modality of APD. Finally, the majority of patients were treated using traditional PD solutions. However, a recent short-term study at our hospital demonstrated similar PPE rates in patients treated with traditional or biocompatible solutions.20 Our study also presents qualities that provide substantial robustness to our conclusions. First, the study population was quite large, allowing for drawing conclusions based on significant results. The available clinical information was also quite complete, and the study design allowed for both cross-sectional and longitudinal comparisons. Finally, the availability of standardised estimates of peritoneal protein transport in serial PETs allowed for the use of this variable in order to adjust for the expected heterogeneity among individual characteristics of peritoneal transport, particularly when comparing between patients on CAPD and those on APD.
To conclude, the individual characteristics of peritoneal protein transport represent a basic determining factor for 24-hour PPE in patients on PD, but the conditions of the dialysis prescription also can influence this variable. The CAPD modality is associated with greater PPE than APD, although this difference is compensated by the direct association between PPE and total volume infused (which tends to be greater in CAPD). Daily UF and time on PD were secondary independent markers of PPE in patients on PD.
Conflicts of interest
The authors declare that they have no potential conflicts of interest related to the contents of this article.
Table 3. Univariate correlations between treatment prescription and optimisation and 24-hour peritoneal equilibrium test
Table 1. General characteristics of the study groups at the start of peritoneal dialysis
Table 2. Variables for treatment prescription and optimisation
Table 4. Predictors for 24-hour peritoneal protein excretion. Multi-level mixed model. Best model
Figure 1. Peritoneal protein excretion in 24 hours in patients treated with continuous ambulatory peritoneal dialysis or automated peritoneal dialysis during the follow-up period (according to treatment type)