Albuminuria is an indicator of sub-clinical organ damage and a marker of cardiovascular risk and renal disease. A percentage of hypertensive patients develop albuminuria despite being under chronic suppression of the renin-angiotensin system (RAS). We previously identified urinary metabolites associated with the development of albuminuria. In this study, we searched for metabolic alterations which reflect different levels within the condition of normoalbuminuria.
Patients, materials and methodsUrine from 48 hypertensive patients under chronic RAS suppression was analyzed. They were classified according to the albumin / creatinine ratio (ACR) into 3 groups: Normoalbuminuria (<10 mg / g); Normal-high (10–30 mg / g in men, or 20−40 mg / g in women); and moderately high albuminuria (microalbuminuria, 30−200 mg / g or 40−300 mg / g, respectively). The metabolome was analyzed by mass spectrometry and a correlation analysis was performed between altered metabolite levels and ACR.
ResultsOxaloacetate, 3-ureidopropionate, guanidoacetate and malate show significant variation between the normo and micro groups. Additionally, these metabolites are able to differentiate between patients in the normo and high-normal range. A significant correlation between metabolites and ACR was found. Observed variations point to alterations in the energy metabolism already in patients with albuminuria in the high-normal range.
ConclusionsThe association between the molecular panel consisting of 3-ureidopropionate, oxaloacetate, malate and guanidoacetate and different levels of albuminuria is confirmed. A metabolic fingerprint was also identified showing variations within the condition of normoalbuminuria allowing an earlier molecular stratification of patients.
La albuminuria es un indicador de daño orgánico subclínico y un marcador de riesgo cardiovascular y de enfermedad renal. Un porcentaje de pacientes hipertensos desarrollan albuminuria a pesar de estar bajo supresión crónica del sistema renina-angiotensina (SRA). Previamente identificamos metabolitos en orina asociados al desarrollo de albuminuria. En este estudio, investigamos alteraciones metabólicas que reflejen distintos niveles dentro de la condición de normoalbuminuria.
Pacientes, materiales y métodosSe analizó la orina de 48 pacientes hipertensos con supresión crónica del SRA. Se clasificaron según el cociente albúmina/creatinina (ACR) en 3 grupos: normoalbuminuria (<10 mg/g); normal-alta (10−30 mg/g en varones, o 20−40 mg/g en mujeres) y albuminuria moderadamente elevada (microalbuminuria: 30−200 mg/g o 40−300 mg/g, respectivamente). El metaboloma se analizó mediante espectrometría de masas y se realizó un análisis de correlaciones entre los niveles de los metabolitos alterados y ACR.
ResultadosOxalacetato, 3-ureidopropionato, guanidoacetato y malato muestran una variación significativa entre los grupos normo y micro. Además, estos metabolitos son capaces de diferenciar entre los pacientes normo y normal-alta. Igualmente se observó correlación significativa entre el nivel de los metabolitos identificados con el nivel de ACR. Las variaciones observadas señalan una alteración del metabolismo energético ya en pacientes con albuminuria en el rango normal-alta.
ConclusionesSe confirma la asociación del panel molecular constituido por 3-ureidopropionato, oxalacetato, malato y guanidoacetato con distintos niveles de albuminuria. Así mismo, se ha identificado una huella metabólica capaz de mostrar variación dentro de la condición de normoalbuminuria, lo que permite una estratificación molecular más temprana de los pacientes.
Hypertension is one of the diseases with the highest prevalence worldwide.1 A 30–40 % of the adult population is hypertensive. One of the first-line of treatment for its control is the chronic inhibition of the renin angiotensin system (RAS inhibition) as monotherapy or in combination with other antihypertensive drugs, with proven efficacy in reducing blood pressure. However, a remarkable percentage of controlled hypertensive patients develop albuminuria (16.1% at 3-year follow-up).2 Albuminuria is the clinical expression of a complex and multifactorial pathophysiological process which is associated with increased cardiovascular risk.3,4 Although the only presence of albuminuria may not be predictive of chronic kidney disease progression,5 there is evidence of an association between changes in albuminuria levels and the development or aggravation of kidney disease.6–8
Albuminuria indicates that there is a subclinical organ damage. The development of albuminuria is a continuous process and as such its consequences on cardiovascular risk and kidney damage must be considered.9 Previous studies have shown that the association between the development of albuminuria and cardiovascular events begins at urine Albumin/creatinine ratio (ACR) level within the normal range of albuminuria, with values as low as 4.4 mg /g10; 6.6 mg/g11 or, in any case with values below 10 mg/g.12 Particularly, the risk of developing cardiovascular disease in diabetics increases by a factor of 10 if albuminuria increases from 10 to 30 mg/d13 and, in the general population, an increase of 5−10 mg / L is associated with a 29% higher risk of mortality from cardiovascular disease.14 In the same line, it predicts the development of hypertension in the high-normal range (<30 mg / g)15 and chronic kidney disease in non-diabetics.7,8
The greatest difficulty in the application of prevention strategies is that it is not possible to anticipate which subjects will develop albuminuria. One of the main reasons is that the underlying molecular mechanisms are not fully understood. The value of urine analysis in the study of cardiovascular disease has been widely demonstrated.16–19 Specifically, in previous studies we have identified urine molecular markers associated with the condition of albuminuria that point to alterations in the immune response, coagulation system, inflammatory response, vascular remodeling and oxidative stress as the main biological processes involved in the development of albuminuria.20–22 In this work we explore the existence of a differential metabolomic profile in subjects classified according to their ACR level in: a) <10 mg / g (normal); b) 10−30 mg / g in men or 20−40 mg / g in women (normal-high); c) 30−200 mg / g or 40−300 mg / g, in men and women respectively (micro). Thus, patients can be separated into those that are not expected to develop albuminuria (normal) and those who are likely to develop albuminuria (normal-high). We analyzed the previously identified metabolic footprint to investigate whether there is metabolic variation associated with an early or incipient albuminuria condition in order to stratify cardiorenal risk at the molecular level and thus better adapt the therapeutic strategy in these patients.
Material and methodsSelection of patientsPatients were recruited from the Hypertension Unit of the Hospital 12 de Octubre in Madrid. A total of 48 hypertensive patients with blood pressure controlled with chronic suppression of the RAS for a minimum of 2 years were selected. Those patients with secondary hypertension were excluded from the study. Patients with and without diabetes mellitus between 45 and 70 years of age were included. The study was performed according to the recommendations of the Declaration of Helsinki and was approved by the Ethics Committee of the Hospital 12 de Octubre, with the prior signed informed consent of the patients.
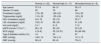
Subjects were classified according to the ACR value into 3 groups: normal (N), individuals with ACR < 10 mg / g, of whom, according to the ROADMAP study, it is known that they will not develop albuminuria23; normal-high (NA), individuals with ACR = 10−30 mg / g (men) or 20−40 mg / g (women) and microalbuminuria (M), individuals with ACR = 30−200 mg / g or 40–300 mg / g, in men and women respectively. The clinical guidelines use a cut-off point of ACR =30 mg / g between albuminuria and moderately elevated albuminuria as a general classification criterion.24 For women, the cutoff point has been slightly increased to 40 mg/g,25 considering that the urinary excretion of creatinine is influenced by muscle mass. Table 1 collects the clinical characteristics of the subjects included in the study.
Clinical characteristics of the patients included in the study.
| Normal (n = 22) | Normal-high (n = 17) | Microalbuminuria (n = 9) | |
|---|---|---|---|
| Age (years) | 57 ± 9 | 64 ± 5 | 65 ± 3 |
| Gender (% male) | 59 | 76 | 66 |
| Cholesterol (mg/dl) | 179 ± 38 | 166 ± 29 | 154 ± 29 |
| Triglycerides (mg/dl) | 110 ± 33 | 125 ± 59 | 122 ± 32 |
| HDL cholesterol (mg/dl) | 54 ± 16 | 53 ± 16 | 50 ± 7 |
| LDL cholesterol (mg/dl) | 102 ± 31 | 88 ± 30 | 91 ± 26 |
| Uric acid (mg/dl) | 5 ± 1 | 6 ± 2 | 7 ± 2 |
| eGFR (ml/min/1.73 m 2 ) | 86 ± 16 | 85 ± 20 | 93 ± 22 |
| ACR (mg/g) | 4 (3−6) | 22 (18−31) | 85 (44−99) |
| Type II diabetes mellitus (%) | 18 | 24 | 67 |
| SBP (mmHg) | 140 ± 14 | 144 ± 14 | 141 ± 19 |
| DBP (mmHg) | 85 ± 8 | 83 ± 8 | 79 ± 5 |
| Antihypertensive treatment (%) | |||
|---|---|---|---|
| ACEI | 18 | 18 | 67 |
| ARA | 41 | 65 | 33 |
| Diuretics | Four. Five | 47 | 22 |
| α-blockers | 18 | 0 | 22 |
| β-blockers | 32 | 29 | 33 |
| Calcium channel blockers | 41 | 71 | 78 |
ACR is expressed as median (interquartile range). The rest of the variables are expressed as frequencies or as mean ± standard deviation.
ACR: albumin / creatinine ratio; ARA: angiotensin receptor antagonist; eGFR: estimated glomerular filtration rate; ACEI: angiotensin- converting enzyme inhibitors; PAD: diastolic blood pressure; PAS: systolic blood pressure.
The first morning urine was collected, centrifuged to remove cell debris, and stored at −80 °C until analysis. Quantitative analysis of metabolites was performed using liquid chromatography coupled to mass reaction spectrometry in selected reaction monitoring mode (SRM-LC-MS / MS). This methodology was selected as “method of the year” by the journal Nature Methods 2012.26 Based on previous studies in our laboratory, metabolites were extracted from the urine after elimination of the protein fraction by organic precipitation.27,28 The supernatant was filtered and analyzed on a QQQ6460 Triple Quadrupole Mass Spectrometer (Agilent Technologies) coupled to a liquid chromatography binary system (1200 series, Agilent Technologies) controlled by the Mass Hunter program (v4.0 Agilent Technologies).
Statistical analysisThe signal corresponding to each metabolite was integrated using the Mass Hunter Acquisition Data Qualitative Analysis B.04.00 program ( Agilent Technologies), and the peak area was obtained. A non-parametric Mann-Whitney statistical analysis was performed, with a 95% confidence level and previous detection of outliers using the ROUT method (Q value = 5%). For the analysis of correlations, a non-parametric Spearman correlation test was used, all using the GraphPad Prism program (version 6.01).
Results and discussionOxalacetate, guanidoacetate and 3-ureidopropionate show lower levels in the group of individuals with microalbuminuria (M) than in those with normoalbuminuria (N). However, Malate levels are higher in M than in N (Fig. 1). These data confirm previous observations in patients with albuminuria developed during the 3-year follow-up prior to sampling (albuminuria de novo) or already present previously (maintained albuminuria).22 It should be noted that these 4 metabolites are capable of differentiating between N patients and those in the NA albuminuria range, and therefore allow for earlier molecular stratification of patients.
The correlation between the urine metabolites levels and the ACR values for each patient was performed. There was a statistically significant correlation in all cases (Fig. 2).
Albuminuria has been associated with an increase in oxidative stress.29 Oxidative stress is caused by a dysregulation in the production and metabolism of reactive oxygen species; the cycle of tricarboxylic acid participates in this regulation. The changes observed in the levels of oxalacetate and malate in patients with albuminuria in the high-normal range and microalbuminuria again point to energy metabolism as a key element in the management of hypertensive patients.30 The guanidoacetate is an intermediate in the metabolism of proline and arginine and creatine precursor, a substrate of creatine kinase. This enzyme has been linked to a failure of antihypertensive treatment, without knowing in detail what are the mechanisms that may mediate this effect.31 In addition guanidoacetate has been proposed as a marker of kidney injury since it is reduced in the urine of transplant patients with normal kidney function.32 Therefore, the alterations of these metabolic processes, indicate an early dysregulation of energy metabolism and the metabolism of arginine and proline in patients with albuminuria in the normal-high range.
A limitation of the present study is the difference in some of the baseline characteristics of the clinical groups, particularly in regard with the percentage of diabetic individuals. Although a greater presence of diabetes mellitus is expected in the group of subjects with microalbuminuria, it would be of interest to evaluate in a larger cohort of only non-diabetic subjects the observed metabolic variations to determine with more precision the degree of contribution of diabetes.
ConclusionsIn this study we have confirmed the association of the levels of the metabolites 3-ureidopropionate, oxalacetate, malate and guanidoacetate with different degrees of albuminuria. For the first time, a molecular fingerprint (metabolic panel) capable of showing variation within the normoalbuminuria condition has been identified being able to distinguish subjects with ACR < 10 mg / g or higher. This fact is noteworthy in that it represents a tool with enormous potential in the therapeutic management of hypertensive patients with ACR levels considered "non-pathological" and who therefore do not receive special medical care. However, these are the patients who would benefit most from early intervention, as they are at increased risk of cardiovascular or kidney disease.
FinancingCarlos III Health Institute-FEDER Funds (PI16/01334, PI13/01873, PI17/01193, PI17/01093, IF08/3667-1, CPII15/00027, CP15/00129, PT13/0001/0013, PRB3 (IPT17/0019 ISCIIIS-GEFI/ERDF), REDinREN (RD16/0009)), Research Aid from the SENEFRO Foundation and the Conchita Rábago Foundation from Jiménez Díaz.
Conflict of interestsThe authors declare that they have no conflict of interest.
To Lucía Guerrero, Luisa Fernández and María Cruz Casal, from Hospital 12 de Octubre.
Please cite this article as: Santiago-Hernandez A, Martinez PJ, Martin-Lorenzo M, Ruiz-Hurtado G, Barderas MG, Segura J, et al. Perfil metabolómico diferenciador asociado a la condición de normoalbuminuria en la población hipertensa. Nefrologia. 2020;40:439–445.