Few studies have analyzed the freedom to choose their renal replacement treatment (RRT) modality in Spain. In a total of 673 patients with ACKD (stage 4 and 5) seen at the outpatient ACKD clinic of Hospital del Mar, Barcelona, Catalonia (Spain) from 2009 to 2020, we retrospectively compared immigrant and Spanish patients in order to analyze the impact of migration on RRT decision-making and its subsequent evolution in advanced CKD (ACKD) consultation and identifies the social and economic needs of this population. One hundred thirteen (16.8%) patients were immigrants and 560 were Spanish (83.2%). Migrants more frequently chose HD at a center (79.5%) than PD (12.5%) compared to Spaniards (HD 55.5% and 25% PD) despite being younger and more independent in basic and instrumental activities of daily living. Immigrant patients started RRT with lower eGFR (8.1 vs. 9.1 mL/min/1.73 m3) and after a shorter follow-up time in the ACKD consultation than the Spaniards (22 vs. 32 months). The language barrier was associated with a greater choice of center-based HD and active employment status favored the choice of PD. Spanish patients had a significantly higher relative risk of mortality compared with immigrant patients (HR = 3.27[95%CI:1.17−9.17], p = 0.024). However, after adjustment by age, this increased relative risk of mortality disappeared (HR 1.99[0.69–5.76], p = 0.206). Almost 60% individuals were not linked to social services. In conclusion, most immigrants in Barcelona choose center-HD versus DP despite being younger and more independent in basic and instrumental activities of daily living and being in a better condition than Spanish patients. Considering the socioeconomic and cultural needs of the immigrant population we serve is necessary to effectively reduce health inequities. Keywords: advanced chronic kidney disease, socioeconomic status, demographic factors, shared decision making, renal replacement therapy, peritoneal dialysis, conservative care, hemodialysis, renal transplantation, language barrier, social determinants of health, immigration, social determinants of health.
Son pocos los estudios que han analizado la libertad de elección de la modalidad de tratamiento renal sustitutivo (TRS) en España. En un total de 673 pacientes con Enfermedad renal crónica avanzada (ERCA) (estadios 4 y 5) atendidos en la consulta externa específica del Hospital del Mar, Barcelona, Cataluña (España) de 2009 a 2020, comparamos retrospectivamente pacientes inmigrantes y españoles para analizar el impacto de la migración en la toma de decisiones del TRS y su posterior evolución en la consulta de ERC avanzada (ACKD) e identifica las necesidades sociales y económicas de esta población. Ciento trece pacientes (16,8%) eran inmigrantes y 560 españoles (83,2%). Los inmigrantes eligen con mayor frecuencia la HD en un centro (79,5%) que la DP (12,5%) respecto a los españoles (HD 55,5% y 25% DP) a pesar de ser más jóvenes y más independientes en las actividades básicas e instrumentales de la vida diaria. Los pacientes inmigrantes iniciaron TRS con un FGe más bajo (8,1 vs. 9,1 ml/min/1,73 m3) y tras un tiempo de seguimiento en la consulta de ERCA más corto que los españoles (22 vs. 32 meses). La barrera del idioma se asoció con una mayor elección de HD en centros y el estatus laboral activo favoreció la elección de DP. Los pacientes españoles tuvieron un riesgo relativo de mortalidad significativamente mayor en comparación con los pacientes inmigrantes (HR = 3,27[IC95%:1,17−9,17], p = 0,024). Sin embargo, después del ajuste por edad, este mayor riesgo relativo de mortalidad desapareció (HR 1,99[0,69−5,76], p = 0,206). Casi el 60% de las personas no estaban vinculadas a los servicios sociales. En conclusión, la mayoría de los inmigrantes en Barcelona eligen el centro-HD frente a DP a pesar de ser más jóvenes y más independientes en las actividades básicas e instrumentales de la vida diaria y estar en mejores condiciones que los pacientes españoles. Es necesario considerar las necesidades socioeconómicas y culturales de la población inmigrante a la que servimos para reducir eficazmente las inequidades en salud.
According to the International Organization for Migration, international migration is expected to increase significantly, potentially reaching 405 million people by 2050.1 Globalization, economic pressures, climate change, environmental degradation, political violence and human rights violations are the main reasons driving of this movement.1,2
In July 2023, the population in Spain was 48.3 million people, of which 8.5 million (17.5%) were born abroad.3 In recent years, immigrants represent the majority of the new population in Spain.
Migration has enormous consequences on the daily lives of people who abandon their places of origin and is negatively associated with health risks and adverse outcomes.4,5 A worsening of the health of these subjects has been observed over time and between generations.6 The rapid growth of international migration and their heterogeneity pose a major challenge for public health equity policies, which require an analysis by health services of the new socio-demographic reality to avoid the danger of inequity in this area.7
Sociodemographic, economic and cultural determinants explain more than 75% of health outcomes.8 Migration should be positioned as a social determinant in its own right.9
Chronic kidney disease (CKD) is a progressive disease that affects more than 10% of the world’s population.10 It is more prevalent among the elderly, women and racial minorities, especially in low- and middle-income countries.10 It is not surprising that this entity and its associated morbidities particularly affect to the immigrant population.11
Few studies have analyzed the troubles and outcomes of immigrant patients with CKD in Spain12,13 and no research has been done on the preferences of this population with regard to the modality of renal replacement therapy (RRT).
The main objective of this study was to analyze the impact of being immigrant on RRT decision making and its subsequent evolution in the advanced CKD (ACKD) clinic. Particularly, the present work investigates the differences between country of origin or language and identifies the social and economic needs of this population.
MethodsPatients and designRetrospective cross-sectional observational study conducted in a group of 673 patients with ACKD (stages 4 and 5, estimated glomerular filtration rate [eGFR] < 30 mL/min/1.73 m2) followed at the ACKD outpatient clinic of the Hospital del Mar, Barcelona, Catalonia (Spain) from 2009 to 2020. All participants went through the same process. Patient inclusion in the ACKD consultation began with a nursing visit, which started the therapeutic decision-making process,14 and consisted of three consecutive sessions corresponding to three phases. In the first, the subject's values and preferences were explored by means of value cards labeled “important, somewhat important and very important”, from which he/she chose two “very important” (for example, if a patient selected “being independent” and “fear of blood and needlesticks” his/her most valued possible treatment option could be peritoneal dialysis [PD]). In a second stage, information on the different options available was given with audiovisual material. Finally, in a third deliberative stage, the individual decided on the RRT modality if he or she felt ready for it. Depending on their circumstances, participants could choose between different RRT options: hemodialysis (HD), PD, renal transplantation (RT) and conservative care (CC). At that time, our center did not have the possibility to offer home HD.
If the patient opted for PD, he/she was sent to a specific PD clinic with the responsible medical and nursing staff; to perform a clinical assessment to decide if the option was feasible. Absolute contraindications for PD were: the existence of moderate/severe mental deficiency without family or institutionalized support, psychosis, active severe depression or severe inflammatory bowel disease, active diverticulitis, intestinal ischemia or abdominal abscess. The remaining patients selected HD, living donor renal transplantation (LDKT) and conservative treatment (CT) remained in the ACKD clinic.
A comparative analysis was performed between immigrant and Spanish patients in relation to their choice of RRT and their subsequent evolution. A subanalysis of immigrants who chose HD or PD was performed, including the country of origin and language barrier, as well as the economic and social needs of this population.
The social workers accessed by telephone those immigrants of the ERCA clinic to obtain information about their social and economic situation.
VariablesDemographic and clinical data were obtained from the medical records. The variables recorded were: age, sex, etiology of CKD (glomerular and diabetic nephropathy), mean follow-up time of ACKD (months), level of dependence in basic activities of daily living (ADL), level of dependence in instrumental activities of daily living (IADL), socioeconomic level according to the mean income of the districts of the primary care centers, Spanish nationality vs. foreign nationality, country of origin, language barrier, eGFR at the start of the ACKD consultation, at the start of the selected RRT, chosen RRT (PD, HD, HT) or live transplant, and whether it was potential transplant patient in the opinion of the nephrologist.
Throughout the evolution in the ACKD follow up, we recorded death, the start of RRT or loss to follow-up and also the type of RRT and the causes that led to its initiation (eGFR <7 mL/min/1.73 m2, acute worsening of CKD, uremic symptoms or congestive heart failure), whether the RRT had been approached as emergency or it was programmed and whether HD was performed with catheter or with a functioning arteriovenous fistula. All patients who died in ESRD or were lost to follow-up were excluded from the final analyses.
Measuring instrumentsDependence for basic activities of daily living (ADL): the Barthel scaleThe Barthel scale13 explores the degree of independence for ADLs. Those included in the original index are 10: eating, moving from chair and bed, personal grooming, going to the toilet, bathing/showering, moving (walking on a smooth surface or in a wheelchair), going up/down stairs, dressing, stool and urine control. The values of the Barthel scale ranges from 0 to 100, with five-point intervals for the original version. The closer to a score of 0, the more dependent he or she is; the closer it is to 100, the more independent. This information is obtained directly from the individual or his or her primary caregiver.15
Dependence on instrumental activities of daily living: the Lawton and Brody scaleThe Lawton and Brody scale16 explores independence in using the telephone, shopping, preparation of meals, cleaning, washing, traveling, taking medications and managing finances. It assigns them a numerical value 1 (independent) or 0 (dependent).
The final score is the sum of the value of all responses. It ranges from 0 (maximum dependence) to 8 (total independence). This information is obtained by asking directly to the individual or his or her primary caregiver.
Assessment of the socioeconomic statusSocioeconomic status was extrapolated according to the residence and district of the primary care center to which the patients belonged. The most recent information (2017) on the average income per district was extracted from official data, provided by the Barcelona City Council.17
The estimate used was the Family available Income per capita, which considers the income accessible for consumption and accumulated savings per person.
Subsequently, and with the aim of simplifying the analysis, we summarized and grouped the scores according to the socioeconomic level of the district in which they lived.18 In this way, the patients were classified into three socioeconomic level groups: low, medium-low and medium-high.
Sub analysis among immigrantsSocial workers retrospectively collected by telephone interview the social and economic situation of immigrants from whom data could be obtained. Some patients were lost for this analysis because information could not be collected (some had returned to their countries or could not be located). In others it was not possible to obtain complete information on some aspects.
The variables recorded were the following: housing (adequate vs. inadequate), administrative situation of the country (regular vs. irregular), economic situation (receiving between the minimum interprofessional wage [MIW] and 1.5 times or more than 1.5 times the MIW), from MIW to minimum contributory retirement income (MCRI), from MCRI to minimum noncontributory pension (MNCRI, no income); type of support (family, formal, institutions, informal (friends, neighbors, etc.) or none.
EthicsThis study followed the regulations of the European Union law on data protection and privacy for all persons within the European Union (GDPR/2018) and the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects.
Statistical analysisNumerical variables were described using the mean and standard deviation (SD), whereas categorical variables were defined with the number and percentage of subjects. Between-group comparisons were performed with Student's t-test for continuous variables and X2 or Fisher's exact (if expected counts were less than 5) for categorical variables. Kaplan-Meier estimation was used to evaluate over time survival in immigrant and Spanish populations. The log-rank test was used to calculate statistical differences between groups. Cox proportional hazards regression models were used to evaluate the relative risk of mortality between Spanish and immigrant patients from the onset of ACKD to the end of follow-up and from the end of follow-up to the date of definitive discharge from ACKD. The risk indices were estimated unadjusted and adjusted for the parameters: age, sex, and both together. All statistical analyses were performed using the statistical package R software version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
ResultsStudy populationA total of 673 patients with CKD stage 4 or 5 were seen in the ACKD clinic during the study period. There were 113 (16.8%) immigrants and 560 were from Spain (83.2%). The most frequent countries of origin of this population in this hospital in Barcelona were non-European countries: Pakistan (29%), Philippines (20.9%) and different Latin American nations (22.7%) followed by North Africa (11%).
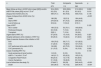
The characteristics of immigrant and Spanish patients were compared at the time of decision making and incorporation into the ACKD clinic (Table 1), and during the follow-up thereafter this and at the initiation of RRT (Table 2).
Comparison between immigrant and Spanish population at the time of decision making and start of ACKD clinic.
| n | Total | Immigrants | Spaniards | p | Missing values |
|---|---|---|---|---|---|
| 673 | 113 | 560 | |||
| Age (mean [SD] | 69.9 (14.1) | 57.1 (15.2) | 72.5 (12.3) | <0.001 | 1 |
| Male (%) | 419 (62.3) | 75 (66.4) | 344 (61.4) | 0.378 | 0 |
| Glomerular Nephropathy (%) | 55 (8.2) | 17 (15.0) | 38 (6.8) | 0.006 | |
| Diabetic Nephropathy (%) | 149 (22.1) | 29 (25.7) | 120 (21.4) | 0.387 | 0 |
| Estimated Glomerular Filtration Rate (mean [SD]) mL/m/1.73 m2 | 20.9 (6.9) | 19.1 (7.7) | 21.3 (6.6) | 0.002 | 0 |
| Dependence on instrumental activities of daily living (mean [SD]) | 6.0 (2.1) | 6.8 (1.9) | 5.8 (2.2) | <0.001 | 63 |
| Dependence on basic activities of daily living (mean [SD]) | 91.8 (13.3) | 96.7 (7.4) | 90.8 (14.0) | <0.001 | 64 |
| Socioeconomic level (%) | <0.001 | 0 | |||
| Low (%) | 216 (32.1) | 63 (55.8) | 153 (27.3) | ||
| Intermediate (%) | 175 (26.0) | 19 (16.8) | 156 (27.9) | ||
| High (%) | 144 (21.4) | 10 (8.8) | 134 (23.9) | ||
| Outside area (not valuable) | 138 (20.5) | 21(18.6) | 117 (20.9) | ||
| Choice of renal replacement therapy (%) | <0.001 | 1 | |||
| Peritoneal Dialysis | 156 (23.2) | 14 (12.5) | 142 (25.4) | ||
| Hemodialysis | 400 (59.5) | 90 (79.6) | 310 (55.5) | ||
| Conservative Treatment | 113 (16.8) | 6 (5.4) | 107 (19.1) | ||
| Transplant (from donor) | 3 (0.4) | 3 (2.7) | 0 (0.0) | ||
| Suitable for transplant (%) | 322 (48.2) | 89 (78.8) | 232 (42) | <0.001 | 5 |
SD: Standard Deviation; ACKD: Advanced Chronic Kidney Disease.
Comparison between the immigrant and Spanish population during the course of the consultation for advanced chronic kidney disease (ACKD) and at the time of initiation of renal replacement therapy (RRT).
| n | Total | Immigrants | Spaniards | p |
|---|---|---|---|---|
| 673 | 113 | 560 | ||
| Mean follow-up time in ACKD clinic (mean [SD])-months | 30.4 (29.0) | 22.9 (26.6) | 31.9 (29.2) | 0.002 |
| eGFR FGe (mean [SD]) mL/m/1.73 m2 | 9.2 (3.9) | 8.1 (2.9) | 9.5 (4.2) | 0.010 |
| Dropout from ACKD clinic (%) | 499 (74.1) | 90 (79.6) | 409 (73.0) | 0.178 |
| Cause of dropout from ACKD clinic (%) | <0.001 | |||
| Death | 196 (39) | 12(13.3) | 184 (44.6) | |
| Start of RRT | 276 (54.9) | 67 (75.3) | 209 (50.5) | |
| Lost of follow up | 32 (6.4) | 11(12.2) | 21(5.1) | |
| Type of RRT | 0.125 | |||
| HD in center | 199 (72.5) | 53 (79.1) | 146 (69.9) | |
| Peritoneal Dialysis | 52 (18.8) | 7 (10.4) | 45 (21.5) | |
| Transplant | 25(9.1) | 7 (10.4) | 18 (8.6) | |
| Urgent start of RRT (%) | 67 (24.6) | 13 (19.4) | 54 (26.3) | 0.327 |
| Hospital admission at the initiation of RRT (%) | 60 (25.3) | 13 (22.4) | 47 (26.3) | 0.681 |
| Type of vascular Access at the initiation of HD | 0.077 | |||
| AVF | 159 (79.5) | 38 (71.7) | 121 (82.3) | |
| CVC | 41 (20.5) | 15 (28.3) | 147 (73.5) | |
| AVF performed at the start of HD% | 164 (82) | 40 (75.5) | 124 (84.4) | 0.110 |
| CVC permanent (%) | 21 (10.5) | 5 (9.4) | 16 (10.9) | 0.500 |
| Cause of starting RRT (%) | 0.144 | |||
| Acute worsening of renal function | 14 (5.2) | 2 (3.0) | 12 (5.9) | |
| eGFR < 7 mL/min/1.73 m2 | 140 (51.7) | 35 (52.2) | 105 (51.5) | |
| Congestive Heart Failure | 66 (24.4) | 12 (17.9) | 54 (26.5) | |
| Uremic Symptoms | 51 (18.8) | 18 (26.9) | 33 (16.2) | |
| Lost of follow from the study (%) | 274(40.7) | 26 (23) | 248 (44.3) | <0.001 |
| Death | 242 (36.0) | 16 (14.2) | 226 (40.4) | <0.001 |
CVC: central venous catheter; SD: standard deviation; AVF: Arteriovenous fistula; eGFR: estimated glomerular filtration rate; HD: hemodialysis.
Immigrant patients were significantly younger (57.1 vs. 72.5 years) and independent than Spaniards, lived more frequently in districts of low socioeconomic status (55.4 vs. 27.5%). They had a higher proportion of glomerular disease (15 vs. 6.8%), were more transplantable as per the judgment of the nephrologist (79.5 vs. 41.8%), and joined the ACKD clinic with lower eGFR (19 vs. 21 mL/min/1.73 m3). Regarding RRT options, immigrants more frequently chose HD at a center (79.5%) than PD (12.5%) as compared to Spaniards (55.5% HD and 25% PD) (Table 1).
Comparison between immigrant and Spanish patients with advanced chronic kidney disease at the time of initiating renal replacement therapy and their evolutionRegarding subsequent follow-up in the ACKD consultation and at the start of RRT (Table 2), immigrant patients started RRT with lower eGFR (8.1 vs. 9.1 mL/ min/1.73 m3) and after a shorter time of follow-up time than Spaniards (22 vs. 32 months). Death was more frequent in Spaniards (44.7%) than in immigrants (12.4%) and loss to follow-up was higher in the immigrants (12.4%) than in Spaniards (4.8%). After a median follow-up of 18 months (interquartile range [IQR] 8.1–35.1), immigrant patients had better survival than Spaniards (82.2 vs. 45.4%, log-rank = 0.01). Unadjusted Cox regression analysis revealed that the spaniards had a significantly higher relative risk of mortality as compared with immigrants, both at the end of ACKD follow-up (hazard ratio [HR] = 2.03 [confidence interval {IC} 95%: 1.13–3.64], p = 0.018) and at the time of definitive discharge (HR = 3.27 [95% CI:1.17−9.17], p = 0.024). After adjustment for age, this higher relative risk of mortality disappeared, both at the end of ACKD follow-up (HR = 1.08 [95% CI:0.59−1.96], p = 0.807) and at the time of definitive discharge (HR = 1.99 [95% CI:0.69−5.76], p = 0.206) (Fig. 1).
Univariate estimate of patient survival according to Kaplan-Meier comparing Spanish and foreign populations, and results of the Cox regression analysis of the unadjusted relative risk of mortality and adjusted by the parameters age, sex and both (time on RRT, all patients).
A) Results from the start of ACKD clinic to the end of follow-up.
B) Results from the end of ACKD follow-up to the date of definitive discharge.
ACKD: advanced chronic kidney disease; RRT: renal replacement therapy.
The characteristics of the 103 immigrant patients who could undergo a complete study by social workers are shown in Table 3. Of these, the majority chose HD in a center (86%) vs. PD (13.5%). The factors associated with the choice of technique were: baseline nephropathy (diabetic nephropathy more frequently opted for HD in centers), degree of dependence on IADLs (more independent patients chose PD), socioeconomic level of the health district (if it was low, they selected more HD in centers and, if it was high, more decided PD), country of origin (South American patients opted for PD and Filipinos and/or Pakistanis mostly chose HD in centers). Finally, the language barrier was related to a greater choice of HD and active employment status favored PD. Regarding the social needs detected, almost 60% of the people were not linked to social services, 10% had no social support, 31.6% had no resources or earned less than 400 euros/month, 78% were unemployed and 27.4% did not have reasonable housing.
Characteristics of immigrant patients according to the technique of choice.
| n | Total | Hemodialysis | Peritoneal dialysis | p |
|---|---|---|---|---|
| 103 | 89 | 14 | ||
| Age (mean [SD]) years | 56.6 (15.1) | 57.5 (14.1) | 51.0 (20.4) | 0.134 |
| Male sex (%) | 69 (67.0) | 62 (69.7) | 7 (5.0) | 0.251 |
| Glomerular nephropathy (%) | 16 (15.5) | 11 (12.4) | 5 (35.7) | 0.065 |
| Diabetic nephropathy (%) | 29 (28.2) | 29 (32.6) | 0 (0.0) | 0.028 |
| Estimated glomerular filtration rate (mean [SD]) mL/m/1.73 m2 | 18.8 (6.8) | 18.6 (6.6) | 20.1 (7.8) | 0.451 |
| Dependency on instrumental activities of daily living (mean [SD]) | 6.8 (1.9) | 6.6 (1.9) | 7.8 (0.6) | 0.037 |
| Dependency on basic activities of daily living (mean [SD]) | 97.0 (7.2) | 96.6 (7.7) | 99.7 (1.4) | 0.149 |
| Country of origin (%) | 0.001 | |||
| Pakistan and partners | 31 (30.1) | 31 (34.8) | 0 (0.0) | |
| North Africa | 10 (9.7) | 9 (10.1) | 1 (7.1) | |
| South and Central America | 24 (23.3) | 15 (16.9) | 9 (64.3) | |
| Philippines | 20 (19.4) | 19 (21.3) | 1 (7.1) | |
| Europe | 11 (10.7) | 8 (9.0) | 3 (21.4) | |
| Others | 7 (6.8) | 7 (7.9) | 0 (0.0) | |
| Language barrier (%) | 43 (41.7) | 42 (47.2) | 1 (7.1) | 0.011 |
| Suitable for transplant (%) | 83 (80.6) | 72 (80.8) | 11 (78.6) | 1.000 |
| Living donor option (%) | 8 (7.8) | 1(1.1) | 7 (50.0) | <0.001 |
| Socioeconomic status (%) | 83 | 74 | 9 | <0.001 |
| Low (%) | 55 (66.3) | 54 (73.0) | 1 (11.1) | |
| Intermediate (%) | 18 (21.7) | 14 (18.9) | 4 (44.4) | |
| High (%) | 10 (12.0) | 6 (8.1) | 4 (4.4) | |
| Adequate housing (%) | 58 (72.5) | 49 (72.1) | 9 (75.0) | 1.000 |
| Adequate administrative situation (%) | 74 (97.4) | 64 (97.0) | 10 (100.0) | 1.000 |
| Active worker (%) | 17 (23.3) | 11 (17.5) | 6 (60.0) | 0.011 |
| Economic remuneration (%) n | 71 | 61 | 10 | 0.068 |
| No income | 22 (31.0) | 20 (32.8) | 2 (20.0) | |
| Minimum interprofessional wage (MIW) at 1.5 MIW | 14 (19.7) | 9 (14.8) | 5 (50.0) | |
| >1.5 times the MIW | 3 (4.2) | 3 (4.9) | 3 (30.0) | |
| From MIW to minimum noncontributory pension (MNCRI) | 18 (25.4) | 15 (24.6) | 0 (0.0) | |
| From MNCRI to mínimum contributive pensión (MCRI) | 14 (19.7) | 14 (23.0) | 0 (0.0) | |
| Types of support (%) n | 81 | 69 | 12 | 0.563 |
| Family | 54 (66.7) | 44 (63.8) | 10 (83.3) | |
| Formal or institutions | 17 (21.0) | 16 (23.2) | 1 (8.3) | |
| Informal or friends or neighbors | 2 (2.5) | 2 (2.9) | 0 (0.0) | |
| No support | 8 (9.9) | 7 (10.1) | 1 (8.3) |
SD: Standard Deviation.
67 immigrant patients started RRT during follow-up (13 started urgently and 54 started on a scheduled basis) (Table 2). No differences were found regarding country of origin (24 from Pakistan and associates [35.8%]; six from North Africa [9.0%]; 12 from South America [17.9%]; 11 from the Philippines [16.4%]; nine from Europe [13.4%]; five from others countries [7.5%]; p = 0.43) or language barrier (27 [40.3%]; p = 0.43). Among immigrant patients who opted for HD (53), those with a language barrier (25) were more likely to initiate HD with a central venous catheter (CVC) (5 [20.0%]) than those who spoke and understood Spanish (0 [0%]; p < 0.04).
DiscussionThe main finding of the present study is that there are significant differences in the choice of dialysis technique between immigrants and Spaniards renal patients. The majority of immigrants opted for in-center HD vs. PD despite satisfying the requirements generally associated with the choice of the home technique: being younger and more independent in ADLs and IADLs, and being in a better condition to be transplanted than Spaniards. From this, it can be deduced that there must be other reasons linked to migration that influence decision making in ACKD beyond the physical conditions of the patients.
As in this study, other publications have also shown that immigrant patients from developing countries are different from the native population, for example, due to younger age, etiology of renal failure (more frequently glomerular), late remission (lower eGFR in immigrants on arrival at the ACKD clinic and at the start of RRT), and more frequent loss of follow-up in the clinic due to trips of patients to visit their countries of origin.19
In our study, the probability of immigrants initiating PD was significantly lower than that of native Spaniards, in contrast to other studies carried out in Canada in which, after controlling for sociodemographic data and comorbidities, East Asians and Indo-Asians were more likely to opt for PD than the white native patients.20 In our work, subjects with a language barrier who lived in a district of associated to low socioeconomic status, such as Filipinos or Pakistanis, were more likely to choose HD in a center than PD. In contrast, immigrants from South American countries without a language barrier were the most likely to choose PD than HD.
In Spain, currently it is not known the actual percentage of patients immigrants followed in nephrology clinics, undergoing dialysis or kidney transplants. The fact is that this variable is not usually included in CKD registries. In the present study, 16% of all patients seen in the CKD clinic throughout 11 years were immigrants and the most frequent countries of origin were not from the European Union. Considering that the in Cataluña the adult population is 6.5 million people, 15.8% are from another region and it is the second autonomous community in number of immigrants, after Madrid, which is the first21; thus the number of immigrant patients seen in nephrology clinics does not seem to be insignificant. The only available data is from a cross-sectional study of the HD population in Madrid in November 2003, in which the percentage of immigrants was 9.3%,12 which is lower than that found in our advanced CKD clinic in Barcelona, also taking into account that 20 years have passed since the publication of this work and during the last years the immigrant population has increased considerably.
There are significant differences between countries of origin and the choice of technique. Immigrants from Pakistan and the Philippines were more likely to choose in-center HD than PD, they had a higher proportion of language barrier and diabetic nephropathy, and lived in lower socioeconomic districts (74% of Pakistanis and 95% of Filipinos) than the rest. A recent study assesses the prevalence of cardiovascular risk factors and cardiovascular disease among Asian immigrants in Catalonia.22 This study found that the prevalence of cardiovascular risk factors such as type 2 diabetes, hypertension, hyperlipidemia and obesity is much higher in the immigrant population from South Asia (Pakistan, India and Bangladesh) as compared to natives and those from China and the Philippines.23 In addition, the use of Shabu-crystal (methamphetamine) by the Filipino population is a fact and it is present in healthcare activity and probably influences the self-care capacity of this population in home-based techniques.24 Cultural misunderstandings between physicians and patients, as well as language barriers, may contribute to disparities in the quality of care. In this context, the design of culturally and linguistically appropriate health strategies and decision-making support tools is of utmost importance.23
Despite the effort to offer all techniques to all patients, the question remains as to what extent the final decision is motivated by the influence of health professionals or by the patients themselves, and whether there are barriers that can be corrected with a different approach towards this population. It is possible that health professionals have been more reluctant to offer a home dialysis program to some immigrants, with economic difficulties or language barriers, in the event of a possible failure of the technique.
As in other studies,25 we observed a higher survival rate for immigrant patients on dialysis as compared to natives in an urban setting in Spain. This is explained by the younger age of immigrants at the start of the ACKD clinic compared to natives, since when adjusting the Cox analysis for age, the survival advantage of the immigrant population is lost.
The older age and comorbidity (higher prevalence of diabetes mellitus) of Spaniards compared to immigrants probably also have an influence on the greater choice of conservative therapy (CT) by the Spanish population (19.1 vs. 5.3%, respectively) and the higher mortality. We cannot rule out the influence of cultural factors on the reduced choice of CT by immigrants.
The main limitations of this study are the observational/retrospective nature of the analysis, the fact that it is performed in a single center, the lack of home HD among the techniques offered and the cross-sectional design of the study, which means that the results are limited to associations and not causality. Although there is a possibility that the average income of the health districts may differ from the personal income of the individual, it is a widely used indirect measure.17,18 Another limitation is that some factors that have been related to the choice of RRT in ACKD, such as the degree of comorbidity, frailty, lifestyle, distance to the center, educational level and verbal or written information about the modality or family support, have not been analyzed in this study.
In summary, most immigrants in Barcelona choose HD at the center vs. PD despite being younger and more independent in ADL and IADL, and being in better conditions than Spanish patients. The socioeconomic conditions and cultural needs of the immigrant population we serve must be taken into account in order to effectively reduce health inequities. The influence of non-medical factors on dialysis decision-making needs to be addressed, and this requires the involvement of an interdisciplinary team that includes social workers.
FundingThis study was conducted without funding.