To the Editor,
Uncontrolled arterial hypertension (AHT) during pregnancy compromises correct gestation development. We describe the case of a 41-year-old pregnant woman who was referred to our unit after having suffered a miscarriage in the tenth week of gestation.
The patient had no personal or family history of interest, and ATH was detected in the eighth week of pregnancy. She visited the emergency department on several occasions due to metrorrhagia and asthenia, with blood pressure (BP) at around 160-170/100-110mm Hg. Alpha-methyldopa was prescribed at 500mg every 8 hours, gradually increasing doses but without adequately controlling AHT. In the tenth week of pregnancy, the patient had a miscarriage and was referred to the outpatient nephrology unit.
In the physical examination BP was 162/100mm Hg and heart rate (HR) 74 systoles. She had no distal oedemas or other data of interest.
Supplementary tests
1. Haemogram: normal.
2. Biochemistry: creatinine: 0.92mg/dl; glomerular filtration rate (GFR) calculated using MDRD-4 equation: 67ml/min; sodium: 140mEq/l; potassium: 3.3mEq/l; calcium: 9.7mg/dl; uric acid: 4.7mg/dl; GOT: 26IU/dl; GPT: 21IU/dl; LDH: 337IU/l; total bilirubin: 0.3mg/dl; normal coagulation, negative indirect Coombs test.
3. Venous gasometry: normal.
4. Urine: negative systematic and sedimentary tests, microalbuminuria/creatinine index: 8µg/mg; uricosuria: 0.3g/24h.
5. Chest X-ray: no pathological findings.
6. Electrocardiogram: sinus rhythm, no blockages or signs of ischaemia.
7. Funduscopy: normal.
8. Anatomopathological exam of the placenta: normal.
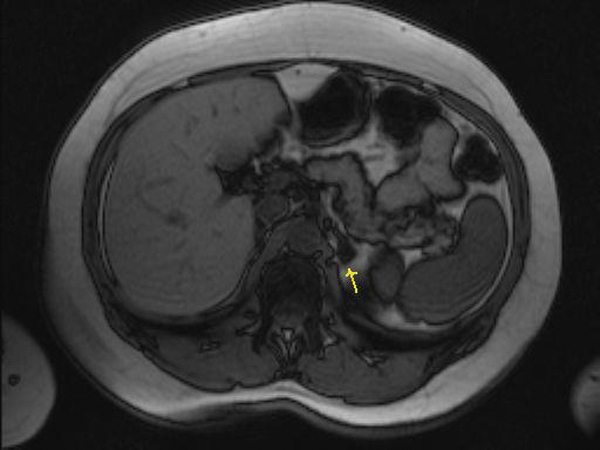
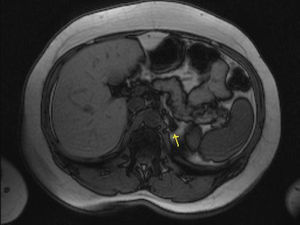
The abdominal ultrasound and renal Doppler scan were normal. Drug treatment was started with calcium antagonists and doxazosin, achieving better pressure control, although it was insufficient. A second analysis found plasma aldosterone of 1161pg/ml and urinary aldosterone of 22.68µg/24h, with a plasma renin activity at baseline of 0.6ng/ml/h and aldosterone/renin rate of 193.3. The remaining parameters (catecholamines in urine, thyroid hormones and plasma cortisol) were all normal. Given the suspected primary hyperaldosteronism (PHA), a saline overload test was performed and 2 litres of physiological saline solution administered over 4 hours. Previous treatment did not have to be modified, however, we do recommend suspending angiotensin-converting enzymes (ACE), angiotensin II receptor antagonists (ARA-II), beta-blockers and diuretics beforehand.1 Following the saline overload, aldosterone was not suppressed, being 27.6ng/dl (normal: <10ng/dl). PHA was confirmed as the cause of her secondary AHT and treatment with spironolactone was started, achieving better blood pressure control and relieving her asthenia. The examination was completed with a CT with contrast medium and magnetic resonance imaging, which revealed a 1cm-adenoma in the left suprarenal gland (Figure 1).
At present, BP is controlled with 50mg of spironolactone per day, and the patient is waiting for a left suprarenalectomy to avoid complications in future pregnancies.
This case illustrates the serious complications that are secondary to poorly controlled ATH during pregnancy, such as miscarriage, abruptio placentae, and delayed foetal growth, which is likely to be related to vasoconstriction and placental endothelial dysfunction.2 The differential diagnosis of ATH during pregnancy involves testing for essential hypertension, pregnancy-related ATH, pre-eclampsia or secondary aetiology.3
Essential ATH. It is difficult to diagnose it during pregnancy if the patient has not been diagnosed with ATH previously or has not had any BP readings. Pregnant patients diagnosed with chronic ATH present with BP equal or above 140/90mm Hg on two occasions before the twentieth week of the pregnancy, which continues to persist 6 weeks postpartum. Our patient claimed that she had no history of ATH and no lesions to the target organ were found due to ATH.
Pregnancy-related ATH. It is the main cause of hypertension during pregnancy,4 and appears during the second half of the pregnancy in patients that were previously normotensive. It is not usually associated with oedemas or proteinuria and BP normalises after the birth, although high BP levels can persist up to 10 days following delivery.
Pre-eclampsia. It is a pregnancy-related disorder, which develops from the 20th week. The patient has arterial hypertension and proteinuria above 0.3g/24h.5 Proteinuria may become apparent in advanced phases of the pregnancy, meaning that in principle, pre-eclampsia should not be ruled out when there is no sign of proteinuria, especially if ATH is diagnosed after 20 weeks of pregnancy, with headaches, oedemas or altered laboratory findings (thrombocytopaenia, altered hepatic enzymes, hyperuricaemia). New low calciuria levels has been reported to be an early pre-eclampsia marker.6 The patient in this case, had ATH before 20 weeks, no analytical alterations were found which would suggest pre-eclampsia.
Secondary ATH. Some authors recommend assessing metanephrine and normetanephrine levels and performing an ultrasound scan of the suprarenal gland for patients with recently diagnosed ATH.5 This is because a pheochromocytoma could be completely asymptomatic and fatal if not diagnosed before the birth. In our study, having dismissed previous essential ATH and pre-eclampsia, we investigated the possibility of secondary ATH, and finally diagnosed primary hyperaldosteronism from the supplementary tests mentioned above.
The treatment of choice for ATH secondary to PHA is eplerenone or spironolactone but both of them should not be used during pregnancy due to the potential feminising effect that aldosterone has on male foetuses.7 We have found very little evidence of eplerenone use during pregnancy.8 Alpha-methyldopa, labetalol and amlodipine can be used as alternative treatments. Surgery should only be indicated during pregnancy for cases that are refractory to conventional treatment9 or if patients have adenomas more than 4cm in diameter.9 New laparoscopic surgical techniques during pregnancy have lead to greater effectiveness and less surgical risk for the mother and the baby. The retroperitoneal approach has more advantages than the transperitoneal one, given that organ movement is more restricted during the surgical procedure and because it uses much lower intraabdominal pressure.10,11
To conclude, PHA diagnosis is very rare during pregnancy, but it must be taken into consideration because early treatment could reduce severe complications related to poor blood pressure control.
Figure 1. MR of left adrenal gland