Renal cortical necrosis (RCN) was first described in 1883 by Friedlander. It is an extremely rare cause of acute kidney injury and usually is irreversible.1 It is more prevalent in developing countries with deficient health systems. Usually there is extensive involvement of the cortex, but sometimes it is localized affecting focal areas. Renal cortical necrosis is observed in 2 peaks of age; first is in early childhood due to perinatal factors, and the second in women of reproductive age due to obstetric causes. Of the non-obstetric causes in the adult population, the most frequent etiology is septic shock.2
Here we present a case of a female, 21 y.o. from Venezuela with no previous relevant medical history who came to the emergency room for a 24h history of fever, headache, blurred vision and photophobia. Physical examination showed neck stiffness and petechia in upper extremities and abdomen. Cranial CT scan without relevant findings. Spinal tap showed biochemical changes compatible with bacterial meningitis. The severity of the clinical symptoms prompted admission to ICU. She developed a Waterhouse–Friedrichsen syndrome with multiorgan involvement. Blood cultures demonstrate the presence of Neisseria meningitidis group B.
The patient developed acute renal failure that required renal replacement therapy with hemofiltration. At that time a possible cause of the acute renal failure was immune allergic interstitial nephritis because eosinophilia was present that may have been related with the antibiotic therapy; therefore, steroid were given but without response. It was observed that the urine sediment had a large number of dysmorphic red blood cells, red cell casts, proteinuria of 0.9g/day and low circulating levels of complement (C3 50.9mg/dl and C4 11.6mg/dl). Blood tests of autoimmunity and serology were negatives. During ICU admission the patient had low urine output and required RRT.
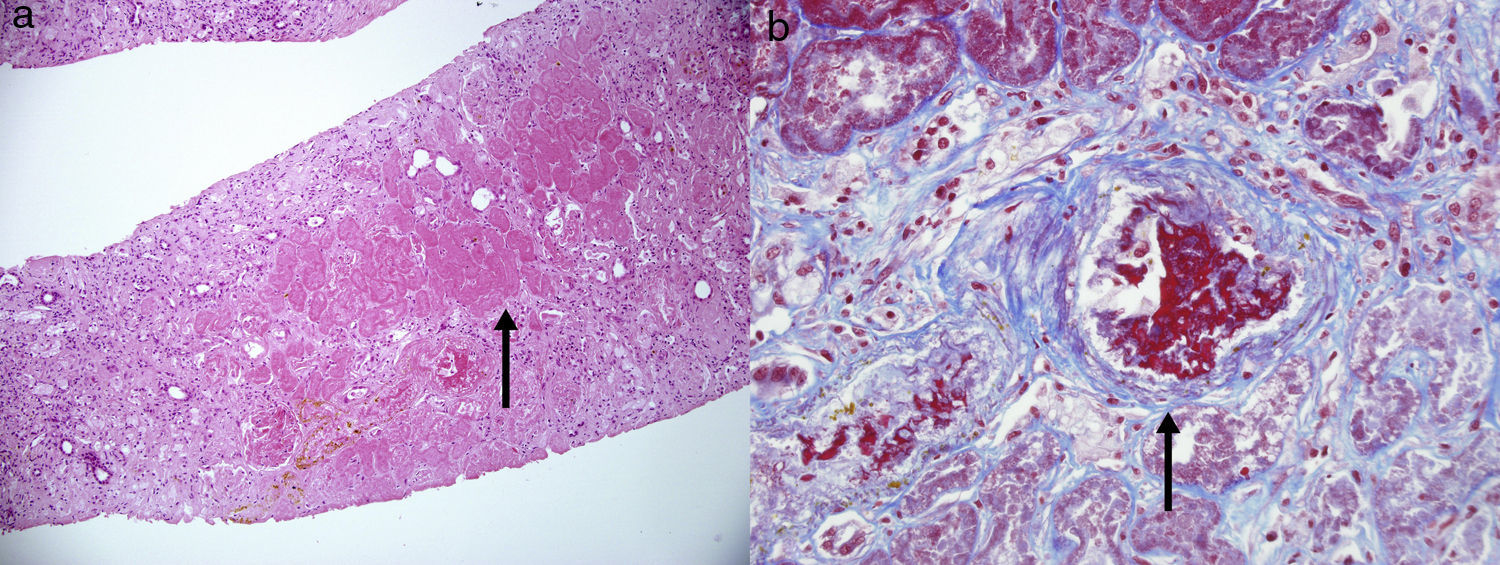
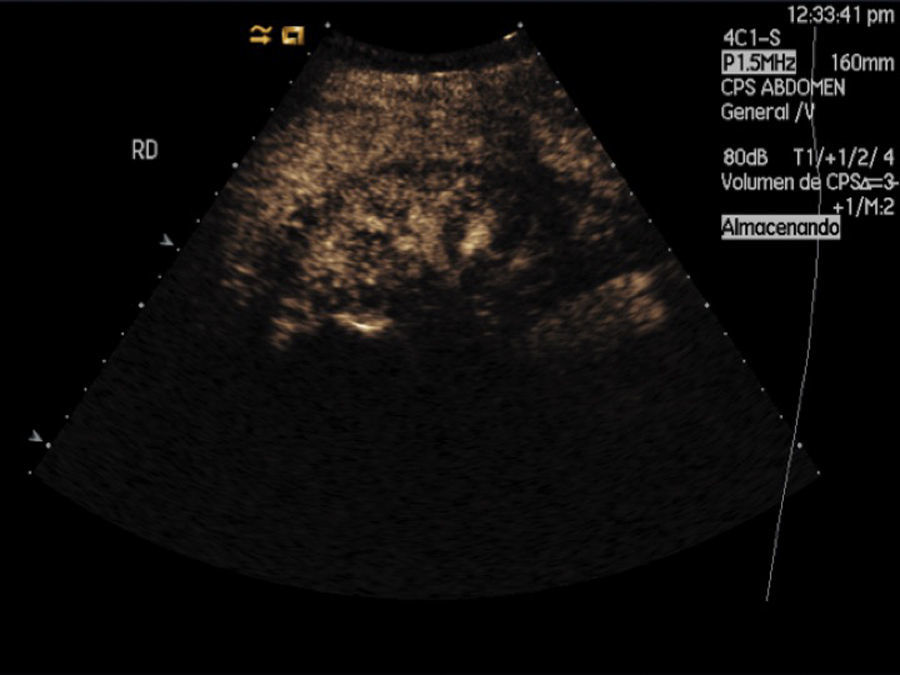
After clinical improvement the patient was transferred to the nephrology ward and a renal biopsy was obtained; there were 20 glomeruli all of them obsolete with multiple foci of cortical necrosis of isquemic origin that did not involve the subcapsular area and did not extend to the deeper areas of the kidney (Fig. 1A). Furthermore. There were many arterial thrombi at different stages of organization with onion like growth of the arterial wall suggesting thrombotic microangiopathy (Fig. 1B). A doppler ultrasound confirmed the diagnosis of cortical necrosis. The patient did not recover renal function and remained on regular dialysis (Fig. 2).
Multiple cortical foci of ischemic necrosis that did not involve the subcapsular area and did not extend to the deeper areas of the kidney (arrow). (b) Arterial thrombi at different stages of organization with onion like growth of the intima of the arterial wall suggesting thrombotic microangiopathy (arrow).
Renal cortical necrosis is caused by the injury of that small arteries that supply blood to renal cortex. This arterial injury can be triggered by an endothelial lesion in a situation of severe renal isquemia or disseminated intravascular coagulation (DIC).3 In 1991, Chervu et al. reported the first two cases of meningococcal sepsis with renal cortical necrosis. Meningococcal sepsis is more frequent in young adults and it is associated to a high mortality. To improve the prognosis it is important to make the diagnosis soon so treatment with antibiotics can be started early. The meningococcus, like other gram-bacteria, stimulates the release of cytokines that mediate vasodilatation, reduction of cardiac output, platelet aggregation and disseminated intravascular coagulation (DIC).
Waterhouse–Friderichsen Syndrome is an acute hemorrhagic necrosis of the suprarenal glands that in most cases is secondary to meningococcal sepsis. More than 75% of these patients develop a petechial rash. The treatment includes antibiotics and steroids. Plasma exchange has been used to remove bacterial endotoxin and cytokines such as TNF-alpha and interleukin-1. Agraharkar et al.4 reported a case of a 20 y.o. patient with meningococcal sepsis that received plasmapheresis during the first 24h producing DIC improved and less requirement of vasopressors drugs.
In summary, renal cortical necrosis is not a frequent cause of acute kidney injury but it has a very bad outcome. The early diagnosis, with image and histology, may change the prognosis of the disease.
Please cite this article as: Rodríguez PM, Morales E, Sánchez Á., Milla M, Martínez MA, Praga M. La necrosis cortical: una causa infrecuente de fracaso renal agudo pero con un pésimo pronóstico. Nefrologia. 2017;37:339–341.