Antecedentes: La biopsia renal (BR) es una técnica fundamental en el estudio de las enfermedades renales. Es también el procedimiento más agresivo por su morbimortalidad, por lo cual resulta fundamental conocer sus complicaciones. Objetivos: El objetivo de nuestro estudio fue cuantificar las complicaciones de la BR percutánea en nuestro centro. Métodos: Se realizó un estudio retrospectivo de todos los pacientes a los que se les realizó una BR percutánea de riñón nativo entre enero de 1992 y diciembre de 2008. Hasta el año 2004 usamos una aguja semiautomática de 18 Gauges (G) y desde esa fecha, de 16 G. Se realizó, además, un estudio prospectivo desde enero de 2009 hasta enero de 2010. Se analizaron: edad, sexo, indicación de biopsia, diagnóstico histopatológico, hipertensión arterial (HTA), creatinina sérica, GFR-MRD-4, proteinuria y hemoglobina previa y posterior a la biopsia. Definimos complicaciones menores como: descenso de la hemoglobina mayor de 1 g/dl y como complicaciones mayores la necesidad de transfusión, cirugía, nefrectomía, arteriografía, embolización o muerte. La BR fue realizada por el equipo de nefrología con control ecográfico y retirando el tratamiento antiagregante. Resultados: El número total de biopsias realizadas en los últimos 18 años ha sido de 867. En el estudio retrospectivo, desde enero de 1992 hasta diciembre de 2008, se realizaron 797 biopsias renales. La edad media de los pacientes fue de 46,8 ± 19,1 años y el 60,7% de ellos eran hombres. Sólo observamos seis complicaciones mayores (0,75%). Tres de los pacientes que las presentaron habían sido sometidos a trasplante hepático, presentaron complicaciones hemorrágicas, dos de ellos precisaron embolización y uno nefrectomía. Las tres restantes complicaciones se presentaron en una paciente hepatópata, una afectada de hemofilia y en la tercera se realizó nefrectomía que evidenció hemangiomas epitelioides múltiples. En el estudio prospectivo (enero de 2009-2010) se han realizado 70 biopsias, observándose complicaciones mayores en un 1,4% (un caso) y menores en un 2% (un caso), datos similares a los del estudio retrospectivo. No hubo diferencias en complicaciones mayores entre la aguja de 16 y la de 18 G. Conclusiones: Las complicaciones mayores fueron del 0,75-1,4% y se presentan, sobre todo, en pacientes sometidos a trasplante hepático. Con el empleo de la aguja de 16 G no se observaron más complicaciones mayores y sí una mayor rentabilidad diagnóstica.
Background: The renal biopsy is essential for the diagnostic of glomerular disease However, it is an aggressive procedure with risk of complications. Objectives: The aim of our study was to evaluate the complications directly related to percutaneous renal biopsy procedure in our centre. Methods: This retrospective study was performed using the data obtanined from all patients who underwent percutaneous renal biopsy of the native kidney from January 1992 to December 2008. A semiautomatic 18 G needle biopsy was used until 2004 and thereafter we used a 16 G needle. From January 2009 to January 2010 we prospectively analyzed changes induced by renal biopsy. We analysed age, sex, indication for biopsy, histopathological diagnosis, hypertension, serum creatinine, GFR-MDRD-4, proteinuria, hemoglobin pre and post biopsy. Minor complications were defined as a decrease in hemoglobin levels greater than 1 g/dL. Mayor complications were: need for blood transfusion, surgery, nephrectomy, angiography, embolization, or death. The renal biopsy was performed by the nephrologist with the help of ultrasound. Anticoagulant therapy was removed prior to the biopsy. Results: Total number of renal biopsies were 867. Seven hundred and ninety five renal biopsies were performed between 1992 and 2008. The prospective part of the study included 70 additional biopsies. Considering all patients, the mean age was 46.8±19 and 60.7% were male. There were only six major complications (0.75%). Three of these mayor complications occurred in liver transplanted patients and required vascular embolization or nephrectomy. The remaining 3 major complications were observed in: one patient with liver disease, another patient had trait of hemophilia and a third patient required nephrectomy which after examination demostrated epitheliod hemanangioma. During the prospective analysis the rate of major and minor complications did not change, 1.4 and 2.0 % respectively. Switching from 18 to 16 G biopsy needle did not result in an increase of major complications. Conclusions: Major complications derived from all renal biopsy during the last 18 years were observed in only 0.75-1.4 %. Major complications occurred mainly in liver transplant patients. The use of 16 G needle provided greater diagnostic yield than the 18 G and it did not cause an increase in complications.
INTRODUCTION
The percutaneous renal biopsy (RB) technique was introduced in the early 1950s and ever since has represented an indisputable study method of renal diseases, in particular the glomerular ones. Meanwhile, it is an invasive examination that should be individually indicated, depending on the clinical condition and the evaluation of the risks and benefits for each patient.1,2 Severe complications may arise such as macroscopic haematuria, perirenal haematoma, arteriovenous fistula, infection, damage to adjacent organs and even renal disease and death. European and American series publishing their experience report major complications at 1.2-6.6%.3-7 This data is vital to thoroughly inform the patient and obtain a signed informed consent.
An article has recently been published about the 50th anniversary of the first RBs performed in Spain.8 However, despite the extended time and experience with the RB technique, there are only two papers by nephrologists that analyse the complications associated with this technique.9,10
The objective of our study is to evaluate the major and minor complications of percutaneous RB and whether the use of needles of different calibres, 18 gauges (18 G) versus 16 G, implies greater diagnostic yield with the same associated risk.
MATERIAL AND METHOD
A retrospective study and a revision of the patient database and medical records to which native kidney percutaneous RB had been performed between January 1992 and January 2009 in our hospital. The study variables were the following: age, gender, clinical and histopathological diagnosis, presence or not of arterial hypertension (AHT), renal disease (MDRD4), proteinuria and (major and minor) complications associated with RB.
Complications associated with percutaneous RB are classified as major when there is need of blood transfusion and/or surgery, nephrectomy, arteriography, embolisation or death and a minor complication is defined as a decrease in haemoglobin > 1g/l without the need for blood transfusion or any other technique. To analyse minor complications, we began a prospective study from January 2009 to 31 December 2009 gathering several parameters, among those the haemoglobin levels prior to and after the RB.
The indication was always individualised, from the evaluation of benefit-risk ratio and with the following requirements: normal or controlled coagulation at the moment of the biopsy and removal of all platelet and/or non-steroidal antiinflammatory drugs (NSAID) a week before.
The reasons for the RB was recorded in the data sheet, such as: 1) nephrotic syndrome; 2) chronic nephritic syndrome; 3) persistent urinary alterations; 4) HTN; 5) acute renal failure; 6) chronic renal failure (CRF); 7) isolated macroscopic haematuria and 8) recurrent haematuria.
Samples were taken through ultrasounds and in real time by the nephrology team without the participation of the radiodiagnosis team. We used a semiautomatic instrument (Bard® MaxCore®) with an 18 G needle prior to 2004 and a 16 G needle thereafter, with a minimum of one and maximum of four attempts. The patient stayed 24 hours in the unit, monitoring his clinical situation after the RB and control haematocrit measurements were performed. No routine control kidney ultrasound was performed except in situations such a decrease in haemoglobin over 1g, intense pain and/or haematuria. We studied the RB indication, the number of glomeruli obtained for the optical microscopy (OM) study and the proportion for the electron microscopy studies. We evaluated the complications found in these two periods and related them to the diagnostic yield.
RESULTS
Eight hundred and sixty seven renal biopsies were performed in 18 years and we observed:
Major complications (17-year retrospective study)
A total of 797 percutaneous RBs were performed on 765 patients in 17 years. The causes that motivated the RB were: nephrotic syndrome in 186 cases (23.4%), chronic nephritic syndrome in 6 cases (0.8%), persistent urinary alterations in 114 cases (14.3%), AHT in 14 cases (1.8%), ARF in 245 cases (30.8%), CRF in 127 cases (16.0%), isolated macroscopic haematuria in 17 cases (2.1%) and recurrent haematuria in 32 cases (4%). Considering all the patients, the mean age was 46.8±19, 60.7% were male and 64% were hypertensive. The mean creatinine level was 2.84 ± 2.55mg/dl and the mean number of glomeruli 9.94 ± 0.036. As in other series, more than half the biopsies were performed (54.2%) for ARF or for nephrotic syndrome.
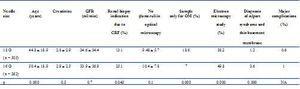
There were major complications in 0.75% of the cases, which correspond with a total of 6 patients. As observed in Table 1, three of these had undergone liver transplantation, presented perirenal haematoma and required blood transfusions; two of them were treated by embolisation and one with nephrectomy. There were other three major complications. One was a patient with liver disease who presented perirenal haematoma and required more than two units of red blood cell concentrate. Another patient, with haemophilia, required embolisation. And a final complication treated with nephrectomy; multiple epithelioid haemangiomas were observed in the pathological specimen (Table 1).
Minor complications (prospective study)
With the aim of analysing the minor complications associated with the RB in our nephrology department, we decided to add a prospective study of the biopsies performed from January 2009 to January 2010. A minor complication was understood as those that involve a decrease in haemoglobin over 1g/l, but without need for transfusion. As a result, the haemoglobin prior to and after the biopsy were measured as a primordial variable, with a haemoglobin mean of 12.8 ± 2.2 and 12.5 ± 2.39 before and after the biopsy, respectively (P = 0.1).
In this period, we observed that of the total number of biopsies performed (n = 70), the mean age of the patients was 46.4 ± 15.3 years, 69.2% were male, the mean creatinine level was 2.86 ±2.34mg/dl and 13.2% (7 cases) presented minor complications. None required blood transfusion and only one case presented severe arterial hypotension.
Diagnostic yield
In the 17 years of retrospective study, two periods of time can be differentiated: before 2004, period in which an 18 G needle was used and after 2004, when a 16 G needle was used. One of the objectives of our study was to determine if the change in needle size involved and increase in diagnostic yield. Furthermore, we studied whether there was a relationship between the needle thickness and the number of major complications associated (Table 2).
The number of glomeruli in the study through OM did not vary significantly; however, complications were not greater while the diagnostic yield improved, increasing the number of samples for the study with electron microscope (38.2% with a 18 G needle and 49.8% with a 16 G needle; P < 0.005) and increasing the diagnosis of diseases such as thin basement membrane or Alport syndrome (P <0.000).
DISCUSSION
It is indisputable that the percutaneous RB is a crucial therapeutic tool in the study of renal diseases and it is also our duty to improve this technique and evaluate our situation in relation to the possible associated complications. For this reason, the moment of performing the procedure, the indispensable experience of the surgeon and the possible complications are matters that need to be reviewed in the present. Furthermore, we have intention of drafting our own informed consent, which includes our experience over the last decade. We can now affirm that percutaneous RB is a low risk procedure, most of the complications are minor, with no clinical repercussions, although this procedure should be performed in a disciplined manner, avoiding risk factors and monitoring the appearance of possible complications.
In our hospital’s nephrology unit, the reference for a population of 798,822, we performed a total of 797 percutaneous renal biopsies on 765 patients over the last 17 years (January 1992 to January 2009), meaning 46.8 renal biopsies/year.
Our premise has been to avoid the risk factors for complications associated with this technique. According to Mackinnon et al.7, the risk of minor complications of percutaneous RB is less if anti-platelet treatment is withdrawn, which is not the case for major complications. All of our patients were withdrawn from anti-platelet treatment a week before the RB, which could have helped in lowering the complication rate. An ultrasound control is generally performed after the RB when the patient presents a decrease in haemoglobin, pain, haematuria and/or haemodynamic instability, although not systematically. The risk of RB has been studied in other papers, for example in liver transplantation candidates with associated renal disease.7 We have observed in our study that three of the six major complications occurred in patients who underwent liver transplantation. Indeed, in some centres, percutaneous RB is contraindicated in patients with double pathology: liver and kidney disorders, despite apparently normal coagulation levels. In these cases transvascular RB is indicated.11-14 We have only recently started to perform this procedure, so our clinical experience is limited.
In this study the complications of RB in two time periods, before and after 2004, have been quantified. Before 2004, an 18 G needle was used, while a 16 G needle was used afterwards; there was no increase in the number of major complications although there was a better diagnostic yield. This has been observed in the decrease in diagnoses such as unexplained CRF and with the increase in samples for electron microscopy with diagnosis of pathologies that require this technique, such as Alport syndrome and thin basement membrane. Proposing a change in the percutaneous RB needle would be related with decreasing the number of complications but, as observed, these have been limited and since there is greater yield with a 16 G needle, we will continue performing biopsies with it. A similar experience with a 14 G needle supports our experience.10
There is only one series carried out in Spain in 1999 with a complication rate higher than 1.7%10 versus the 0.75-1.4% in our hospital. Major complications in Europe and the United States range between 1.2 and 6.4%.3-7 Regarding minor complications, they are estimated at 6.6-19.7%5,6 and 11.3% in our analysis. The number of major complications obtained in our study is low, even lower than those described elsewhere, which could be explained, among other aspects, because the technique is performed by nephrologists with a broad experience and with real time ultrasound control. Furthermore, we follow a strict patient selection protocol for RB, evaluating the risks-benefits and contraindicating its use in those treated with anti-platelet and anti-inflammatory drugs or any medication that could potentially affect the coagulation periods. The complications registered were presented in high risk patients, mainly patients subjected to transplantation or some degree of liver dysfunction.
Lastly, although in a low percentage, the presence of major complications compels us to perform a strict selection of the patients that will undergo percutaneous RB, especially in patients with liver diseases, in order to achieve diagnostic yield, help to establish the prognosis and contribute to modify the treatment with no risks to the patient.
To summarise, the rate of major complication associated with percutaneous RB in our centre was 0.75-1.4%, and the minor ones was 13.2%. The change of needle from 18 G to 16 G did not add morbidity but did increase the diagnostic yield. This is the information the patient should receive before signing the informed consent for a percutaneous renal biopsy according to our experience, as described in this revision.
Table 1. Characteristics of the patients with major complications
Table 2. Diagnostic yield