To the Editor,
Cinacalcet is an allosteric modulator that stimulates the calcium-sensing receptor on the surface of parathyroid cells when activated by the extracellular calcium ion and inhibits parathyroid hormone (PTH) release. At the same time it decreases levels of serum phosphorus and calcium.1 This calcimimetic agent has established itself as a mainstay in the treatment of secondary hyperparathyroidism, and is also useful in persistent hyperparathyroidism after renal transplantation, in primary hyperparathyroidism and hyperparathyroidism due to parathyroid carcinoma.1-3
We report our experience in treatment with cinacalcet in a case of hyperparathyroidism and hypercalcaemia due to an ectopic mediastinal parathyroid gland in a patient with chronic renal failure (CRF). We found no cases of hyperparathyroidism due to ectopic thyroid glands treated with cinacalcet in the current literature. However, there were two cases of haemodialysis patients successfully treated with this drug4,5 who were affected by parathyromatosis (hyperfunctioning parathyroid tissue
distributed throughout the neck, which is a rare cause of recurrent hyperparathyroidism after total or subtotal parathyroidectomy).
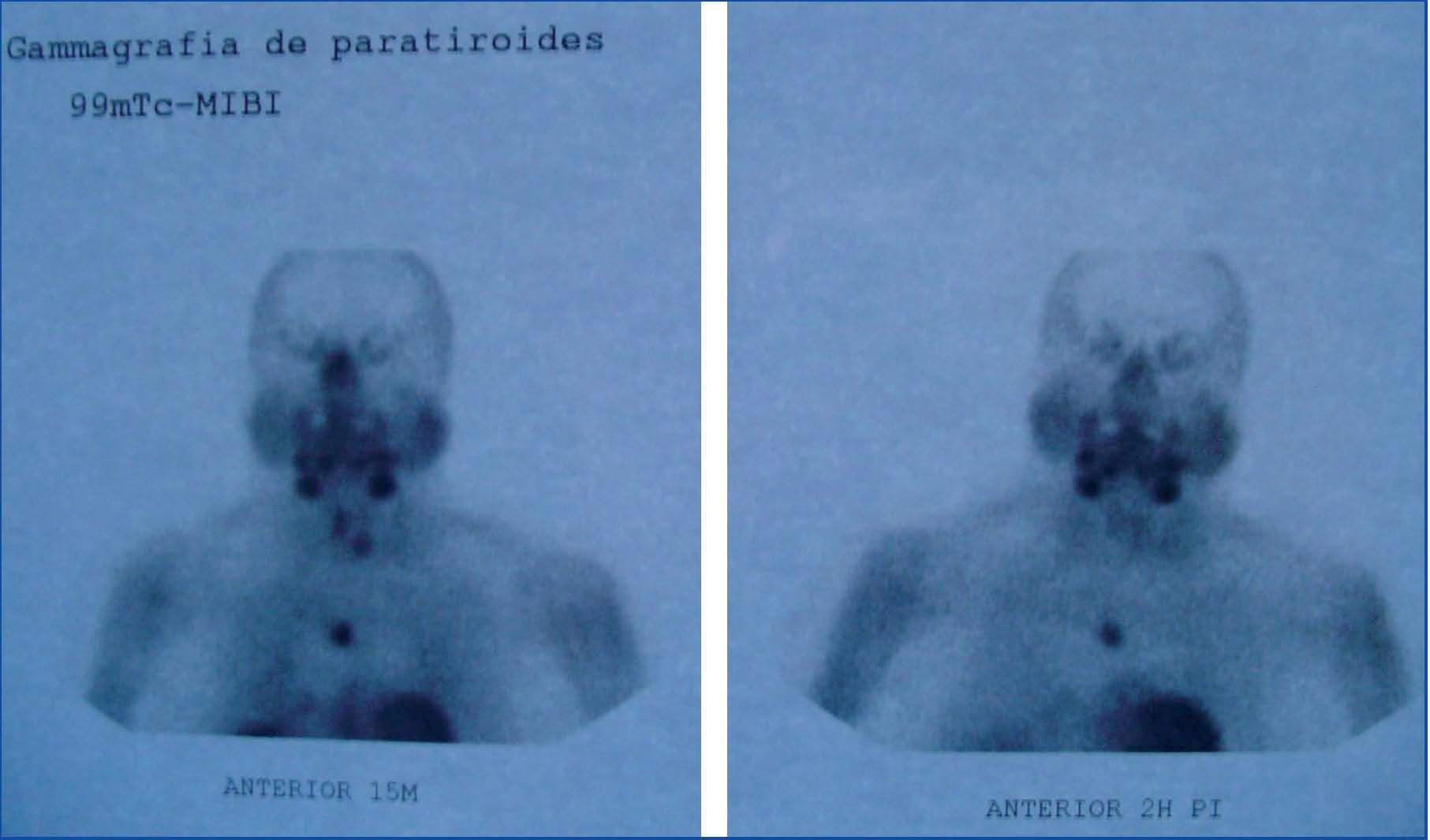
We describe the case of an 80-year-old woman referred to our department two years before due to stage 4 CRF of unknown origin. She had a history of obesity, poorly controlled hypertension (HT), gout, post-thyroidectomy hypothyroidism, generalised osteoarthritis and a gastric ulcer. The analytical tests revealed the following data: creatinine 3.8mg/dl, serum calcium 10.7mg/dl, phosphorus 4.5mg/dl and iPTH 725ng/ml. Tc-Sestamibi parathyroid scintigraphy showed ectopic hyperfunctioning parathyroid tissue in the mediastinum (Figure 1). Cinacalcet treatment was started (under a compassionate use programme) at a dose of 30µg every other day. The frequency of administration had to be increased and, subsequently, resolution of the hypercalcaemia was observed and the treatment was withdrawn due to gastrointestinal intolerance. However, hypercalcaemia of 11.2mg/dl returned and creatinine had increased to 4.13mg/dl with clinical deterioration (fatigue, walking difficulty, and headache) treatment was resumed at 30µg every 48 hours. With good tolerance and evident clinical improvement, normalisation of calcaemia was achieved after a month. The cinacalcet dose was progressively increased to optimise iPTH figures and an arteriovenous fistula was subsequently performed to prepare the patient for renal replacement therapy, being the estimated glomerular filtration rate 13ml/min. One year after starting the calcimimetic treatment at a dose of 90µg and 60µg on alternate days, hypocalcaemia of 7.8mg/dl was found, therefore, oral calcitriol was added to the therapy. Two years after diagnosis, the patient had a good quality of life with creatinine levels of 4.17mg/dl, serum calcium of 8.4mg/dl and iPTH of 404ng/ml. The cinacalcet dose was 90µg and 60µg on alternate days and calcitriol 0.25µg per day. Concomitantly, a proper control of blood pressure was reached.
When a patient with advanced CKF presents hypercalcaemia, in addition to secondary hyperparathyroidism, autonomous hyperparathyroidism should also be considered, for example, hyperparathyroidism caused by an ectopic parathyroid adenoma. Hence the usefulness of Tc-Sestamibi scintigraphy in differential diagnosis.6 Cinacalcet may be useful in the treatment of hypercalcaemia and control of hyperparathyroidism due to hyperfunctioning ectopic parathyroid gland, thereby avoiding surgery in elderly patients with high comorbidity. This medication is generally well tolerated, with nausea and vomiting as the most frequent side effects. Hypocalcaemia may also develop in approximately 5% of patients receiving cinacalcet. This is rarely symptomatic and may be treated by changing or adjusting the dose of phosphorus binders containing calcium or administering vitamin D derivatives.1
As we noted in our patient, administration of cinacalcet helped to stabilise the progression of CKF and improve blood pressure control, thereby being able to decrease the dose and number of antihypertensive drugs.
Figure 1. Tc-sestamibi parathyroid scintigraphy