Incidence of use for various renal replacement therapies is well known, but no data are available on the use of conservative treatment.
ObjectiveTo assess the proportion of patients with chronic kidney failure receiving conservative treatment.
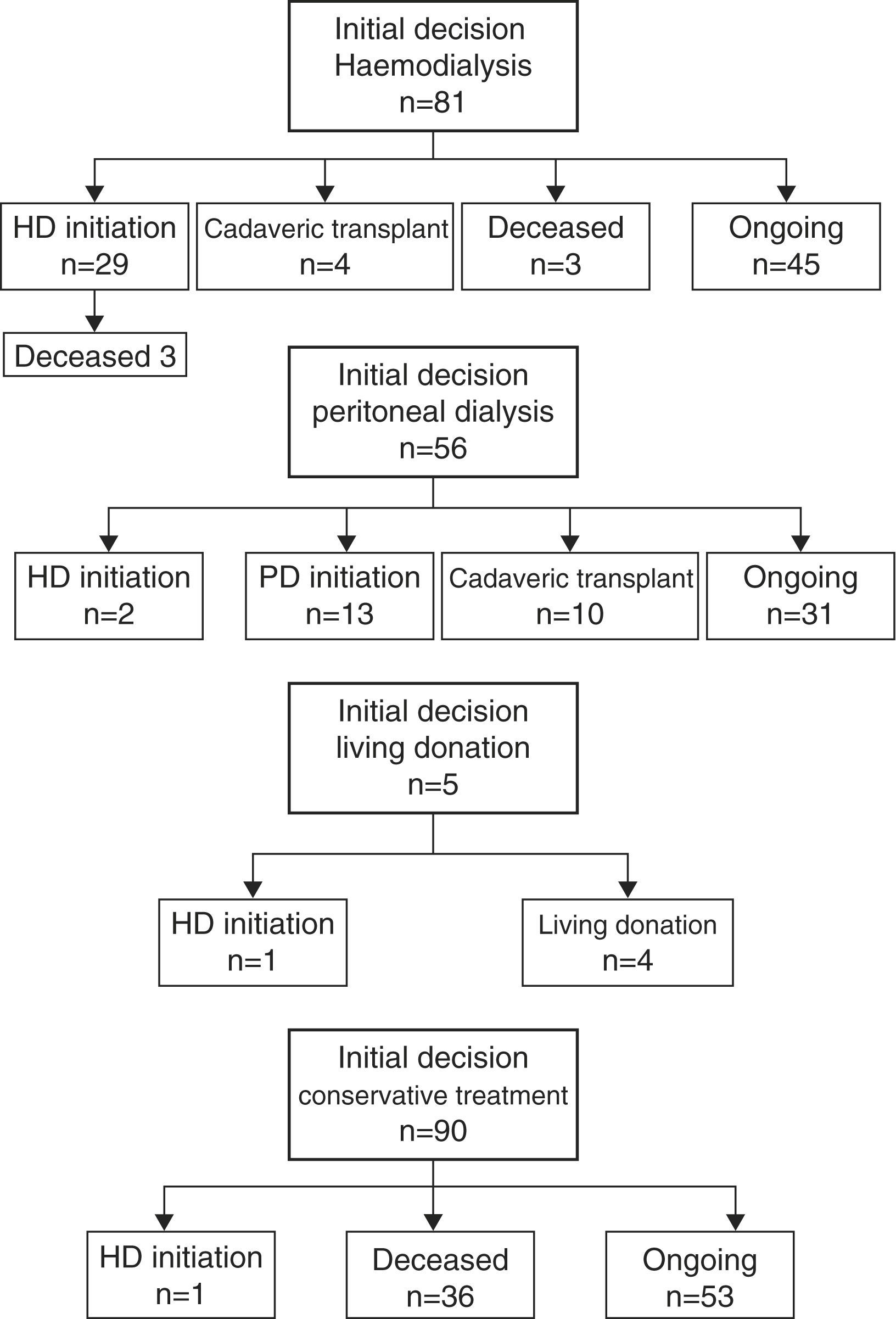
ResultsFrom July 1, 2013 to June 30, 2014, 232 patients with stage 5 CKD were seen in the Nephrology Department. After having received information on the existing therapeutic options and having known the opinion of their physicians, 81 patients (35%) selected haemodialysis, 56 (24%) preferred peritoneal dialysis, 5 (2%) selected a preemptive transplant from a living donor, and in 90 (39%) a conservative treatment option was selected. In a univariate analysis using logistic regression, variables associated to a preference for conservative treatment were age, Charlson index excluding age, walking difficulties, and the level of functional dependendce, with the first three factors achieving statistical significance in a multivariate analysis. Presence of a severe disease with a poor prognosis was the main reason for selecting a conservative treatment (49%), with the second one being symple, patients refusal to receive a renal replacement therapy (26%).
Mortality rate was 8.2/100 patient-months in conservative therapy group versus 0.6/100 patient-months in patients receiving renal replacement therapy (p<0.001). In patients receiving conservative therapy, baseline glomerular filtration rate at the time of study enrollment was the only variable showing a significant impact on survival.
ConclusionsAbout 39% of patients with stage 5 CKD seen over a 1-year period in the Nephrology Department received conservative therapy. Age, co-morbidity, and functional disability were the factors associated to selecting a conservative therapy option.
La incidencia de las diversas modalidades de tratamiento sustitutivo renal es conocida, pero no sucede así con la opción de tratamiento conservador.
ObjetivoConocer la proporción de pacientes con insuficiencia renal crónica sometidos a tratamiento conservador.
ResultadosEntre el 1 de julio de 2013 y el 30 de junio de 2014 fueron atendidos en el Servicio de Nefrología 232 casos con ERC en estadio 5. Tras recibir una información sobre las diversas alternativas terapéuticas y con la opinión del médico responsable, 81 enfermos (35%) optaron por el tratamiento con hemodiálisis, 56 (24%) mostraron preferencia por la diálisis peritoneal, 5 (2%) por el trasplante de vivo prediálisis, y en 90 enfermos (39%) se decidió realizar tratamiento conservador. En el análisis univariante de regresión logística las variables asociadas a la elección de tratamiento conservador fueron la edad, el índice de Charlson sin contar la edad, el grado de dificultad para la marcha y el grado de dependencia funcional, quedando los 3 primeros con significación significativa en el análisis multivariante. La existencia de una enfermedad grave con mal pronóstico a corto plazo fue la principal causa por la que se indicó el tratamiento conservador (49%), y la segunda fue la negativa del enfermo a recibir tratamiento sustitutivo renal (26%).
La tasa de mortalidad fue de 8,2/100 enfermos-mes en el grupo de tratamiento conservador y de 0,6/100 enfermos-mes en el grupo que decidió optar al tratamiento sustitutivo renal (p<0,001). En el grupo tratado de forma conservadora, el filtrado glomerular en el momento de inclusión en el estudio fue la única variable que influyó de forma estadísticamente significativa sobre la supervivencia.
ConclusionesEl 39% de los pacientes con ERC en estadio 5 atendidos durante un año en el Servicio de Nefrología fueron tratados de forma conservadora. Edad, comorbilidad y discapacidad funcional fueron las variables que se relacionaron con la elección de tratamiento conservador.
The distribution of patients into the different modalities of renal replacement therapy is known, however it is not clear the percent of patients that end up undergoing conservative treatment. The study “Epidemiology of Chronic Renal Disease in Spain” (Epidemiología de la Insuficiencia Renal Crónica en España, EPIRCE) showed that the prevalence of CKD-5 is in Spain is 0.03%, which is 300 patients per million inhabitants.1 According to the data from the Dialysis and Transplant Registry of the Spanish Society of Nephrology, 120 patients per million inhabitants started dialysis treatment or had an anticipated renal transplantation in the year 2012.2 Based on these data, it could be inferred that around 60% of the patients with CKD-5 do not receive renal replacement therapy due to one of the following reasons: they were poor candidates for such a therapy, they die for unknown reasons or it is also possible that they were not aware that the suffered from renal disease.
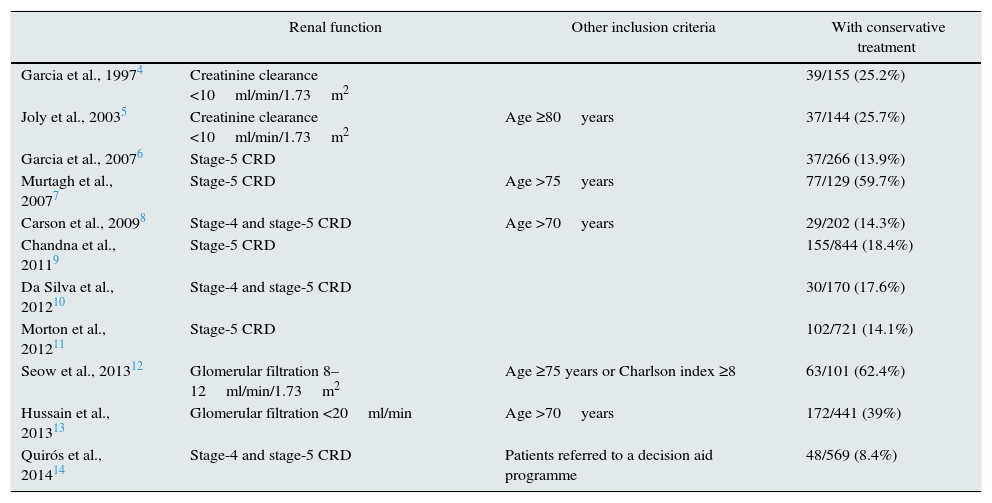
There is little information available on the percentage of patients with CKD on conservative therapy and the available data is very variable due to the great disparity of the population under analysis.3Table 1 shows a summary of the main studies that have been published. The numbers concerning Spain4,6,14 are very far from what we would have expected to obtain when the data from the EPIRCE study and the incidence of renal replacement therapy were compared. The data from hospitals in other countries also vary significantly according to the critera of selection.5,7–13
Percentage of patients undergoing conservative treatment for CRD in different published series.
| Renal function | Other inclusion criteria | With conservative treatment | |
|---|---|---|---|
| Garcia et al., 19974 | Creatinine clearance <10ml/min/1.73m2 | 39/155 (25.2%) | |
| Joly et al., 20035 | Creatinine clearance <10ml/min/1.73m2 | Age ≥80years | 37/144 (25.7%) |
| Garcia et al., 20076 | Stage-5 CRD | 37/266 (13.9%) | |
| Murtagh et al., 20077 | Stage-5 CRD | Age >75years | 77/129 (59.7%) |
| Carson et al., 20098 | Stage-4 and stage-5 CRD | Age >70years | 29/202 (14.3%) |
| Chandna et al., 20119 | Stage-5 CRD | 155/844 (18.4%) | |
| Da Silva et al., 201210 | Stage-4 and stage-5 CRD | 30/170 (17.6%) | |
| Morton et al., 201211 | Stage-5 CRD | 102/721 (14.1%) | |
| Seow et al., 201312 | Glomerular filtration 8–12ml/min/1.73m2 | Age ≥75 years or Charlson index ≥8 | 63/101 (62.4%) |
| Hussain et al., 201313 | Glomerular filtration <20ml/min | Age >70years | 172/441 (39%) |
| Quirós et al., 201414 | Stage-4 and stage-5 CRD | Patients referred to a decision aid programme | 48/569 (8.4%) |
The Ramon y Cajal hospital in Madrid provides healthcare assistance to a population of 550,000 inhabitants. Any patient who needs renal replacement therapy is attended in the Hospital Nephrology Service, and the incidence and prevalence of the various options of treatment are known. To determine the percentage of patients who are being treated conservatively, we have initiated a registry including all patients suffering from CKD-5 who were attended in the Nephrology Service. Below, we show our experience during the first 12 month period of our registry.
Materials and methodSince 1/7/2013, all the patients with stage-5 CRD who were attended in the different areas of the Nephrology Service of the Ramon y Cajal hospital (inpatient consultation, outpatient consultation, hospitalisation and interconsultations from other services) were incorporated into a registry in which basic clinical and analytical data were gathered. Patients who had renal transplants were excluded. The glomerular filtration rate was estimated by the MDRD4-IDMS formula.
An essential section of the registry refers to the therapeutic option chosen after the patient and his/her family had received detailed information regarding all the existing methods (haemodialysis, peritoneal dialysis, renal transplant and conservative treatment). The indication for conservative treatment was always agreed upon with the patient and his/her family, and this decision was registered in his/her medical record and in the issued clinical report. In these cases, the main reason for which a patient was not considered to be a candidate for renal replacement therapy was also requested, with one of the following five possibilities to be chosen: acute disease not curable by dialysis or renal transplant influencing short-term survival, functional deterioration, gait difficulties, cognitive deficit-significant psychiatric disorder, or the patient's decision.
The date of inclusion in the registry is the date of the first visit the patient made to the Nephrology Service in the period of time under analysis, and the clinical and analytical data correspond to that moment. The follow-up period for each patient begins on the date of inclusion and ends on the date the patient passed away or on the day the study finalised (30/6/2014). Patients who started renal replacement therapy were not ruled out at the beginning of it.
To ensure that the population sample was complete, we asked the Biochemistry Department for a correspondence of all the analysis requests submitted by the Nephrology Service between 1/7/2013 and 30/6/2014, in which the glomerular filtration rate was under 15ml/min/1.73m2. After ruling out transplant patients and cases of acute renal failure or of reversible deterioration in renal function in patients with CRD, all stage-5 CRD cases were identified and this population was compared to the one from the existing registry. Cases not included previously were incorporated into the registry, taking into account the date of inclusion of the first blood test with glomerular filtration rate<15ml/min/1.73m2, and clinical data were recovered retrospectively.
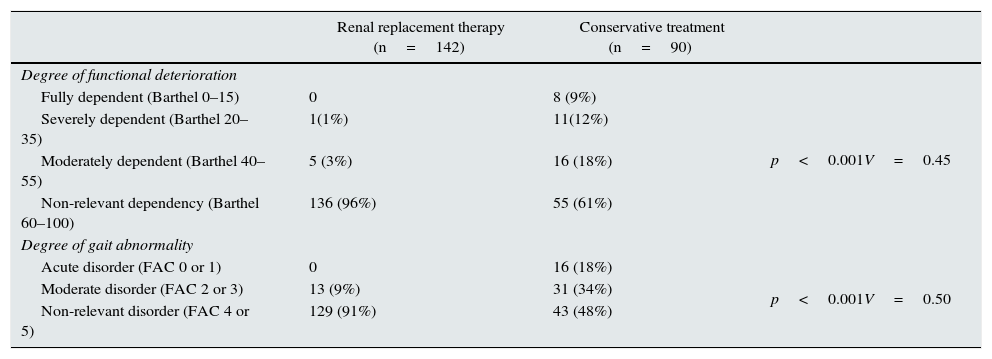
As a comorbidity index we used the Charlson index without taking into account the age component. Functional deterioration was assessed using the Barthel index15 and gait abnormalities using the FAC scale.16 If the score in the Barthel index is below 60, the patient is considered to be dependent in order to carry out basic daily life activities (from 40 to 55, the dependency degree is considered moderate, from 20 to 35 the dependency is severe and below 20, the patient is considered fully dependent). The gait FAC scale has six categories (0: patient cannot walk; 1: patient walks with difficulty held by another person; 2: patient needs support from another person to walk; 3: patient can walk only under supervision; 4: patient can walk independently on level ground, but requires help on stairs; 5: patient can walk independently anywhere). If the score on the FAC scale is between 0 and 1, it is considered that the patient has acute gait abnormalities, if the score is between 2 and 3, the disorder is considered moderate, and if the score is between 4 and 5, it is considered that there are no gait abnormalities or that they are mild.
The patients who were assigned conservative treatment were given the option to continue the follow-up at the chronic renal disease division of the Nephrology Service or at the Palliative Care Unit. All the patients who were given care in the chronic renal disease division followed the same care protocol that was applied to the patients who chose the renal replacement therapy alternative. The patients who were attended at the Palliative Care Unit followed the specific protocol that was previously described for these cases.17
Statistical analysisThe glomerular filtration rate, the Charlson index and the follow-up time have normal distributions (Kolmogorov–Smirnov test), and the results are expressed as mean±SD. Age does not follow a normal distribution and is expressed as median and interquartile range. The comparison of the numeric variables with normal distribution was performed using the analysis of variance (ANOVA) or the Student's t-test, and for age we used the Mann–Whitney test. The qualitative variables are expressed as percentages of the population under study and they were compared using Fisher's tests and the Chi-square test; to evaluate the degree of association between qualitative variables we used the Cramer's V coefficient that ranges between 0 (no association) and 1 (perfect association). To evaluate the dependence between the option for conservative treatment and certain variables, we carried out a logistic regression analysis, submitting the adjusted odds ratio (OR) and the confidence interval (CI) of 95%. To analyse the predictor variables for mortality within the group treated conservatively, we used the Cox proportional hazards model. A p<0.05 was considered statistically significant.
ResultsBetween 1/7/2013 and 30/6/2014, 232 patients with stage-5 CRD were attended at the Nephrology Service. These patients were not given dialysis nor were they transplanted. 206 patients were prospectively included in the CRD registry; the other 26 were retrospectively incorporated after being identified in the patients’ correspondence provided by the Biochemistry Service. There are 141 males (61%) and 91 females (39%), their age ranging between 15 and 93 (median age is 75, interquartile range 66, 82). The aetiologies of renal disease were: vascular nephropathy (25%), diabetic nephropathy (24%), glomerulonephritis (12%), interstitial nephritis (8%), polycystic kidney disease (6%), other nephropathies (11%) and unknown origin (14%). Glomerular filtration rate at the moment of incorporation in the registry was 11.5±2.8ml/min/1.73m2 (range 3.2–14.9ml/min/1.73m2).
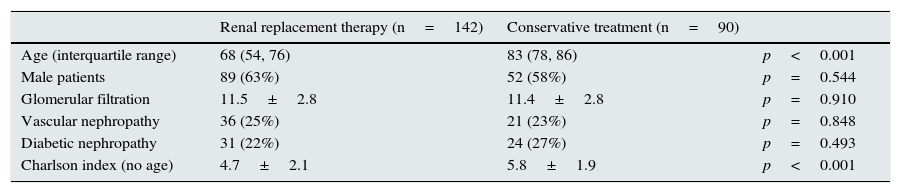
After receiving information regarding the different therapeutic alternatives and with the advice of the physician in charge, 81 patients (35%) opted for haemodialysis treatment, 56 (24%) preferred peritoneal dialysis, 5 (2%) preferred predialysis living donor renal transplantation, and 90 patients (39%) decided to undergo conservative treatment. Table 2 shows the most relevant clinical data at the moment of inclusion in treatment according to the chosen therapeutic option.
Clinical and analytical data according to the therapeutic option chosen.
| Renal replacement therapy (n=142) | Conservative treatment (n=90) | ||
|---|---|---|---|
| Age (interquartile range) | 68 (54, 76) | 83 (78, 86) | p<0.001 |
| Male patients | 89 (63%) | 52 (58%) | p=0.544 |
| Glomerular filtration | 11.5±2.8 | 11.4±2.8 | p=0.910 |
| Vascular nephropathy | 36 (25%) | 21 (23%) | p=0.848 |
| Diabetic nephropathy | 31 (22%) | 24 (27%) | p=0.493 |
| Charlson index (no age) | 4.7±2.1 | 5.8±1.9 | p<0.001 |
The 142 patients who opted for renal replacement therapy were younger (median age was 68, interquartile range 54, 76) (p<0.001), and their Charlson index was lower (4.7±2.1) (p<0.001) than the 90 patients from the conservative treatment group. The degree of functional deterioration and gait abnormalities were very selective variables between both groups of patients (Table 3). The level of association between these variables and the decision to undergo conservative treatment was slightly higher for the degree of gait abnormality (V=0.50) than for the degree of dependence (V=0.45). Functional deterioration and gait abnormalities are closely related variables (p<0.001, Cramer's V coefficient=0.60).
Degree of functional deterioration (Barthel index) and of gait abnormalities (FAC scale) according to the therapeutic option chosen.
| Renal replacement therapy (n=142) | Conservative treatment (n=90) | ||
|---|---|---|---|
| Degree of functional deterioration | |||
| Fully dependent (Barthel 0–15) | 0 | 8 (9%) | p<0.001V=0.45 |
| Severely dependent (Barthel 20–35) | 1(1%) | 11(12%) | |
| Moderately dependent (Barthel 40–55) | 5 (3%) | 16 (18%) | |
| Non-relevant dependency (Barthel 60–100) | 136 (96%) | 55 (61%) | |
| Degree of gait abnormality | |||
| Acute disorder (FAC 0 or 1) | 0 | 16 (18%) | p<0.001V=0.50 |
| Moderate disorder (FAC 2 or 3) | 13 (9%) | 31 (34%) | |
| Non-relevant disorder (FAC 4 or 5) | 129 (91%) | 43 (48%) | |
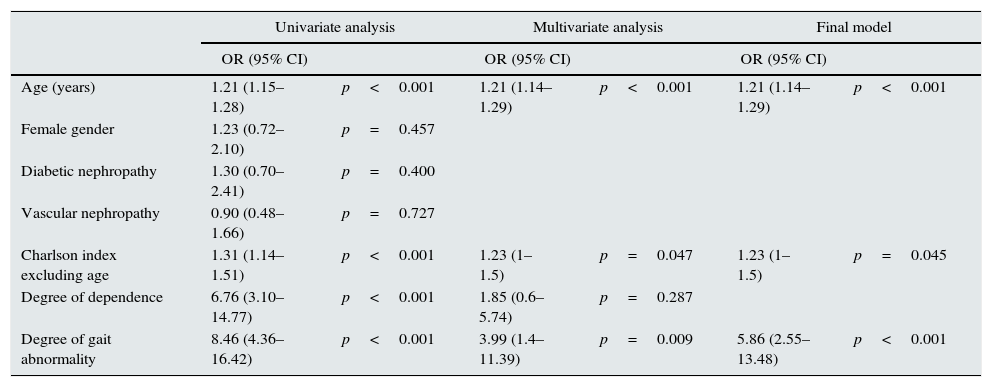
In the univariate analysis of the logistic regression (in which we used as dichotomous dependent variable the decision to undergo conservative treatment or renal replacement therapy), age, the Charlson index, degree of dependence and degree of gait abnormalities were associated with the choice of conservative treatment. In the multivariate analysis, age, degree of gait abnormalities and the Charlson index reached statistical significance (the latter being on the edge of statistical significance) (Table 4).
Variables associated with the decision to undergo conservative treatment.
| Univariate analysis | Multivariate analysis | Final model | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||
| Age (years) | 1.21 (1.15–1.28) | p<0.001 | 1.21 (1.14–1.29) | p<0.001 | 1.21 (1.14–1.29) | p<0.001 |
| Female gender | 1.23 (0.72–2.10) | p=0.457 | ||||
| Diabetic nephropathy | 1.30 (0.70–2.41) | p=0.400 | ||||
| Vascular nephropathy | 0.90 (0.48–1.66) | p=0.727 | ||||
| Charlson index excluding age | 1.31 (1.14–1.51) | p<0.001 | 1.23 (1–1.5) | p=0.047 | 1.23 (1–1.5) | p=0.045 |
| Degree of dependence | 6.76 (3.10–14.77) | p<0.001 | 1.85 (0.6–5.74) | p=0.287 | ||
| Degree of gait abnormality | 8.46 (4.36–16.42) | p<0.001 | 3.99 (1.4–11.39) | p=0.009 | 5.86 (2.55–13.48) | p<0.001 |
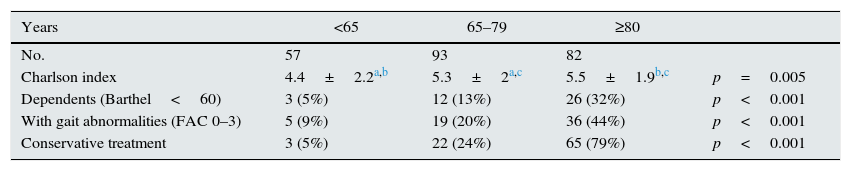
Table 5 shows the value of the Charlson index and the percentages of dependent patients, patients with gait abnormalities, and patients with conservative treatment by age group. The Charlson index shows a lower value, with statistical significance, in the age group of patients below the age of 65, compared to the other two groups. There is no statistically significant difference between the two groups above that age.
Charlson index (no age) and percentages of patients with dependence, gait abnormalities and election of conservative treatment, according to age group.
The main reason for which a patient was not considered as a candidate for renal replacement therapy, of which there were 44 patients (49%), was due to the existence of an acute concomitant disease, which was not expected to improve with dialysis or transplantation and which influenced short-term prognosis, 13 cases (14%) were due to the degree of functional dependence and gait abnormalities, and 10 patients (11%) due to dementia or acute psychiatric disorder. The other 23 patients (26%) turned down the option to undergo renal replacement therapy even though there was no absolute contraindication against it. Compared to the 67 patients who had contraindications for dialysis, the 23 patients voluntarily included in the conservative therapy were older (median age was 86 vs 82, p=0.010) and had a lower Charlson index (4.1±1.2 vs 6.4±1.7, p<0.001). The patients’ decision to undergo conservative treatment increased with age: 1 patient out of the 13 conservatively treated was below the age of 75 (8%), six patients out of 39 between the age of 75–84 (15%) and 16 patients out of 38 were 85 or older (42%) (p=0.007).
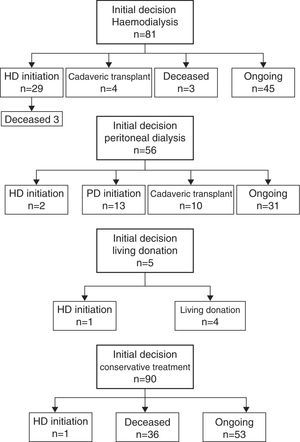
Fig. 1 shows the evolution of the patients according to the therapeutic option chosen at the beginning. During the 12 months of the study, 64 patients started renal replacement therapy: 33 (52%) were treated with haemodialysis, 13 (20%) with peritoneal dialysis, and 18 (28%) received anticipated renal transplants (four from living donors and 14 from cadaver grafts). The glomerular filtration at the start of renal replacement therapy was the following: haemodialysis 5.5±2.6ml/min/1.73m2; peritoneal dialysis 8.4±3.5ml/min/1.73m2 and anticipated renal transplant 8.4±2.8ml/min/1.73m2 (p=0.003 between haemodialysis and peritoneal dialysis, p<0.001 between haemodialysis and anticipated renal transplant).
40% of the patients assigned to the conservative treatment group (36 cases) and 4% of the patients who had chosen renal replacement therapy (six cases, all from the subgroup that had chosen treatment with haemodialysis; three passed away before initiating said treatment) passed away. Due to the higher mortality rate, the follow-up period was shorter for the conservative treatment group (4.9±3.2 vs 7.2±3.7 months (p<0.001)). The mortality rate was 8.2/100 patients-month in the conservative treatment group and 0.6/100 patients-month in the group that opted for renal replacement therapy (p<0.001).
In the group of patients treated conservatively, we analysed the influence of the different variables related to mortality using the Cox proportional hazards model. Evaluated individually, age, gender and primary renal disease variables were not associated with mortality, but the Charlson index was, regardless of age (regression coefficient: 0.185, p=0.029), the glomerular filtration at the moment of inclusion in the study (regression coefficient: −0.238, p<0.001), the assignation to conservative treatment due to medical contraindication and not voluntarily (regression coefficient: 0.309, p=0.041), the degree of dependence (regression coefficient: 0.391, p=0.006), and the degree of gait abnormality (regression coefficient: 0.567, p=0.010). When we built a Cox model with these five variables, only the glomerular filtration continued influencing mortality with statistical significance and of protective type (regression coefficient: −0.256; OR: 0.77, CI: 0.67–0.88, p<0.001).
Out of the 90 patients assigned to conservative treatment, 41 (46%) were voluntarily given care in the Palliative Care Unit (six were transferred to a half-stay hospice and 35 were treated within the Home Care Program).
By 30/6/2014, 129 patients with stage-5 CRD were receiving care at the Nephrology Service. These patients were not given dialysis nor were they transplanted. Out of those patients, 76 (59%) chose to receive renal replacement therapy (45 chose haemodialysis and 31 peritoneal dialysis) and 53 (41%) remained with the conservative treatment option.
DiscussionDuring the 12 months of the study, 64 patients from the control population of the Ramon y Cajal Hospital began renal replacement therapy for the first time. The annual incidence of new patients (116.4patients/million inhabitants) is similar to that of the national registry and slightly higher than that of the autonomous registry of Madrid (104.6patients/million inhabitants in 2012).18
If the data from the EPIRCE study are comparable to our region, for the population given care at the Ramon y Cajal Hospital, there must be around 165 patients with stage-5 CRD. If we assume that this population remains stable over time due to the natural flow of incoming and outgoing patients, according to our incidence of patients who begin renal replacement therapy, we must consider that about 101 patients (61% of the patients with stage-5 CRD) do not come to undergo dialysis or renal transplants due to various reasons (decision to undergo conservative treatment, death, hidden disease). The rate of conservative treatment in patients with stage-5 CRD monitored at the Nephrology Service is 39% if we calculate it from a total of 232 patients given care at the Nephrology Service during one year, and 41% in 129 patients monitored the day the study was finalised. To these percentages we should add 1% corresponding to the three patients who chose renal replacement therapy and died before starting treatment, but we are still far from the theoretical percentage comprising 61% of patients with stage-5 CRD who ultimately would not receive renal replacement therapy.
By 30/6/2014, the Nephrology Service was monitoring 129 patients with stage-5 CRD. To achieve the number in accordance with the EPIRCE study (165 cases), we lack 36 more patients. It is possible that their renal disease was not yet diagnosed or that they were being assisted at other services or healthcare institutions. It is possible that the majority of these last cases were not referred to the Nephrology Service because their doctors did not consider them to be candidates for renal replacement therapy, and if they had been taken into account they would have increased the rate of patients treated conservatively and we would have come closer to the theoretical number.
In our series, as well as in the rest of the series published,4,9,10,13,19 and as expected, patients treated conservatively are characterised as being elderly patients with comorbility as compared to the patients who chose the various options for renal replacement therapy. Functional capacity, as measured by degree of dependence and gait abnormalities, has been a clearly differentiating factor between both groups of patients. It is possible that in the decision to indicate renal replacement therapy, the impact on functional capacity will be more important than age and comorbility.10 Functional deterioration was the main cause to not include patients for dialysis in the Garcia et al. series of 1997.4 However, in our series, when asked what was the main reason for choosing conservative treatment, the most common cause was the existence of an acute disease influencing short-term survival (49% of the total of the cases). Functional deficiency was only claimed as the main reason in 14% of the cases, which indicates that the prognosis of the clinical condition had more influence than the functional impact.
The patient's refusal to undergo dialysis treatment is especially relevant, and in 26% of our cases it was the reason for including them in the conservative treatment group. In the series of the Gregorio Marañón Hospital from Madrid, the patient's decision was the reason for exclusion from dialysis treatment in 14.6% of the patients given care within the home care program.19 In the first study conducted at the Nephrology Service at the Parc Taulí Healthcare Corporation in Sabadell, the patient's decision was the reason for conservative treatment in 25.6% of the cases, the same percentage as ours.4 In the following review, this percentage increased to 35.1% and was the first reason to not assign patients to dialysis treatment.6 In our series, the patients who refused dialysis treatment had a lower comorbility rate than the rest of the patients in conservative treatment, data that are in line with the absence of medical contraindications to undergo dialysis treatment in these patients. Old age was the main variable associated with this decision.
As a consequence of population ageing, the incidence and predominance of elderly patients who reach stage-5 CRD increase exponentially. There are publications that show positive results regarding dialysis treatment in the elderly.20,21 As an isolated variable, age should not be a factor in determining indication for renal replacement therapy, and this choice was taken into account for all patients in our series, regardless of age. Nevertheless, it is clear that age is associated with the election of conservative treatment.19 In our series, this association was considered of statistical significance both in the univariate and multivariate logistic regression analysis. In the analysis by age groups, the percentage of patients with conservative treatment clearly increases with age, just as the degree of dependence and the degree of gait abnormalities increase. This increase cannot be attributed to a higher comorbility (the Charlson index stabilised in patients age 65 and older), but to a progression in the functional disability rate that comes with age, and to the patient's decision, which was the main cause for not assigning patients to dialysis treatment in the oldest age group.
During the 12 months under study, 64 patients started renal replacement therapy (33 with haemodialysis, 13 with peritoneal dialysis, and 18 with anticipated renal transplant). Except for the anticipated renal transplant, there were few changes between the therapies chosen at the beginning and at the end (two patients who had chosen peritoneal dialysis, one patient who had a renal transplant from a living donor and one patient undergoing conservative treatment began renal replacement therapy with haemodialysis at the end).
The mortality rate was greatly higher in the group of patients assigned to conservative treatment: the mortality rate, expressed in 100 patients-month, was almost 14 times higher than that of patients who opted for renal replacement therapy. We must take into consideration that all the patients with stage-5 CRD who were assisted at the Nephrology Service were included in the study, and many of them were at an advanced stage of the disease. In fact, 46% of the patients assigned to conservative treatment were transferred to the Palliative Care Unit; most of them were receiving Home Care.17
It is clear that our data correspond to the patients attended at the Nephrology Service and do not include the cases monitored at other services or healthcare institutions nor do they include the population with hidden disease in this situation. However, they provide information on the percentage of patients undergoing conservative treatment. These data must be taken into account and compared to the experience at other centres in order to gain precise knowledge of the magnitude of this problem.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Teruel JL, Burguera Vion V, Gomis Couto A, Rivera Gorrín M, Fernández-Lucas M, Rodríguez Mendiola N, et al. Elección de tratamiento conservador en la enfermedad renal crónica. Nefrologia. 2015;35:273–279.