Postdilution online haemodiafiltration (OL-HDF) with high convection volumes improves the survival of patients on haemodialysis1 and achieves greater elimination of medium-large molecules and protein-bound uraemic toxins.2,3 Just as Kt/V is used to standardise the dose of diffusion to the needs of the patient,4 we have used weight, body surface or body surface area or total body water to adjust the efficiency of convective transport in OL-HDF.5 In this study, we analyse the data in the article by Abad et al., “Protein-bound toxins: added value in their removal with high convective volumes” (Nefrologia 2016;36:637–42) to evaluate the effect of body composition on the efficacy of OL-HDF in the elimination of medium-large molecules and protein-bound toxins.
Demographic data, weight and height were collected from the 13 patients included in the study. In addition a body composition analysis was performed by bioimpedance spectroscopy (Body Composition Monitor®, FMC), predialysis, before a second weekly session during the last 3 months. Data from the 40 OL-HDF sessions were collected and the association between the percentages of reduction and the different body composition parameters was analysed. The convective volume was adjusted to these parameters to evaluate the relationship between the elimination of molecules and the standardised convection dose.
The age was 39.4±26 years, 87% men, weight 75.3±13.5kg, and 1.86±0.2m2 and 26.1±4.6kg/m2. The bioimpedance spectroscopy data were: overhydration 0.9±1L; Total body water (TBW) 42.3±9.8L; extracellular water (ECW) 18.7±3.4L; intracellular water (ICW) 23.5±6.8L; lean tissue 51.3±18.3kg (17.5±5.1kg/m2); fatty tissue 16.7±13.3kg (8.1±6.8kg/m2); adipose tissue 22.2±18.1kg; cell mass 30.3±12.7kg.
It was found a significant negative correlation between the reduction of medium-large molecules (beta-2 microglobulin, myoglobin and prolactin) and weight, BMI, surface area, TBW, ECW and ICW. The reduction of p-cresyl sulphate and indoxyl sulphate was negatively correlated with weight, surface, TBW, ECW, ICW, lean tissue and cell mass. The reduction of interleukin-6 and homocysteine was not related to any body composition parameter.
The convective volume (28.3±5.1L) was adjusted to the surface area (26.8±6.8L/1.73m2), weight (0.4±0.16L/kg), TBW (0.72±0.26L/L), ECW (1.59±0.51L/L) and ICW (1.34±0.55L/L), being the parameters associated with efficiency in the reduction of molecules. Table 1 shows the correlation between the convective volumes (adjusted and not adjusted to body composition) and the reduction percentages.
Correlations between standardised/non-standardised convective volume and percentage reduction of medium-large molecules and protein-bound toxins.
| Molecules (molecular weight) | Beta-2 microglobulin(11.8kDa) | Myoglobin(17kDa) | Prolactin(22kDa) | Interleukin-6(26kDa) | Homocysteine(135Da) | p-Cresyl sulphate(187Da) | Indoxyl sulphate(212Da) |
|---|---|---|---|---|---|---|---|
| Reduction percentages | 81.3±6.4 | 60±11.5 | 60.1±14.3 | 28±17.2 | 58.6±8.8 | 44.4±15.7 | 48.7±14.1 |
| Pearson | p (sig.) | Pearson | p (sig.) | Pearson | p (sig.) | Pearson | p (sig.) | Pearson | p (sig.) | Pearson | p (sig.) | Pearson | p (sig.) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Convective volume | 0.607 | <0.001 | 0.431 | 0.006 | 0.395 | 0.013 | 0.113 | 0.613 | 0.492 | 0.005 | 0.630 | 0.001 | 0.461 | 0.027 |
| Convective volume/1.73m2 | 0.747 | <0.001 | 0.522 | 0.001 | 0.509 | 0.001 | 0.860 | 0.780 | 0.433 | 0.009 | 0.653 | 0.001 | 0.510 | 0.013 |
| Convective volume/weight | 0.698 | <0.001 | 0.545 | <0.001 | 0.561 | <0.001 | 0.800 | 0.724 | 0.356 | 0.036 | 0.651 | <0.001 | 0.464 | 0.026 |
| Convective volume/TBW | 0.708 | <0.001 | 0.528 | 0.001 | 0.481 | 0.002 | 0.129 | 0.567 | 0.327 | 0.056 | 0.677 | <0.001 | 0.523 | 0.010 |
| Convective volume/ECW | 0.755 | <0.001 | 0.537 | 0.001 | 0.492 | 0.001 | 0.116 | 0.697 | 0.374 | 0.027 | 0.677 | <0.001 | 0.533 | 0.009 |
| Convective volume/ICW | 0.663 | <0.001 | 0.496 | <0.001 | 0.465 | 0.003 | 0.138 | 0.541 | 0.287 | 0.095 | 0.667 | 0.001 | 0.506 | 0.014 |
ECW: extracellular water; ICW: intracellular water; sig.: significance; TBW: total body water.
In bold: correlations that exceed that obtained with the unadjusted convective volume. In italics: insignificant correlations.
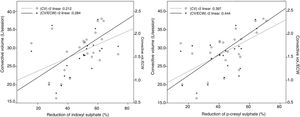
By adjusting the convection dose to body composition, we obtained a more accurate picture of the elimination of medium molecules and protein-bound toxins, such as p-cresyl sulphate and indoxyl sulphate. The strongest correlations between the reduction of beta-2 microglobulin, myoglobin and prolactin were with the convective volume adjusted for ECW, weight or body surface. The convective volume adjusted for ECW was the index with the highest correlation with indoxyl reduction and p-cresyl sulphate.
Other studies find ECW to be the best parameter to adjust the dose of convective transport in OL-HDF to predict the elimination of medium size molecules, while TBW or surface area can be helpful when bioimpedance spectroscopy is not available.6 In this new analysis, it is confirmed that the elimination of protein-bound molecules in OL-HDF, in addition to being conditioned by the amount of convective transport and the proportion of plasma protein binding, also depends on body composition. The influence of body composition and fluid distribution probably reflects the distribution volume of these molecules or their availability to be purified. In this regard, the ECW used to standardise convective transport is also the index that best predicts the elimination of protein-bound toxins such as indoxyl or p-cresyl sulphate (Fig. 1).
In conclusion, body composition influences the elimination of uraemic toxins of different sizes, in addition to protein-bound molecules. Convective volume adjusted to ECW or TBW is a useful marker to evaluate the efficacy of OL-HDF in the elimination of protein-bound molecules and toxins.
Please cite this article as: Macías N, Abad S, Aragoncillo I, Hernández A, Torres E, Santos A, et al. La composición corporal influye en la eliminación de toxinas urémicas unidas a proteínas en la hemodiafiltración online. Nefrologia. 2019;39:434–436.