Pregnancy in haemodialysis patients continues to be rare due to various factors that decrease fertility. Conception rates varying from 0.3 to 2.2%.1,2 Maternal-foetal complications are greater in haemodialysis patients than in the general population, although the latest published series provide figures of successful pregnancies close to 70%, which is a result of improvement in dialysis techniques and maternal-foetal care.3
Maternal complications are: spontaneous abortion, abruptio placentae, anaemia, infection, premature rupture of membranes, polyhydramnios, preterm delivery, arterial hypertension, pre-eclampsia, eclampsia, haemorrhage, caesarean section and maternal death. Complications of the newborn (NB) are: intrauterine growth restriction, prematurity, acute and chronic foetal distress, respiratory distress and intrauterine or neonatal death.
Some published results recommend that patients be dialysed for as long as possible, preferably more than 24 h a week and, and at the time of delivery, try to dialyse on the same day.4
We present the case of a pregnant woman on haemodialysis with an insufficient last session prior to delivery and a live NB with analytical parameters similar to those of the mother, with preserved diuresis without clinical or haemodynamic repercussions and without the need for treatment.
She was a 26-year-old woman with a history of dyslipidaemia and chronic kidney disease secondary to class IV lupus nephropathy on standard haemodialysis of three sessions per week of four hours each during two years, through arteriovenous fistula, residual diuresis of 500 ml, and medical treatment was 40 mg of atorvastatin and 200 mg of hydroxychloroquine daily.
In the presence of amenorrhoea, pregnancy was confirmed, so the dialysis time was intensified to six weekly sessions of four hours duration and the concentration of calcium and bicarbonate in the dialysis bath was decreased to avoid water electrolyte imbalances. Enoxaparin was used as an anticoagulant and ultrafiltration was limited to 2 l per session to avoid problems of uteroplacental perfusion. Treatment with folic acid and oral iodine was started. A non-restrictive diet was prescribed, except for salt and water. Weekly pre- and post-dialysis analytical laboratory tests and gynaecological check-ups were performed.
At week 18, arterial hypertension was detected and treatment was started with methyldopa 250 mg every 8 h, with good control of blood pressure throughout the pregnancy until the end of the pregnancy. Haemoglobin remained around 11 g/dl, with intravenous iron requirements of 100 mg per week and increased darbepoetin to 60 g weekly.
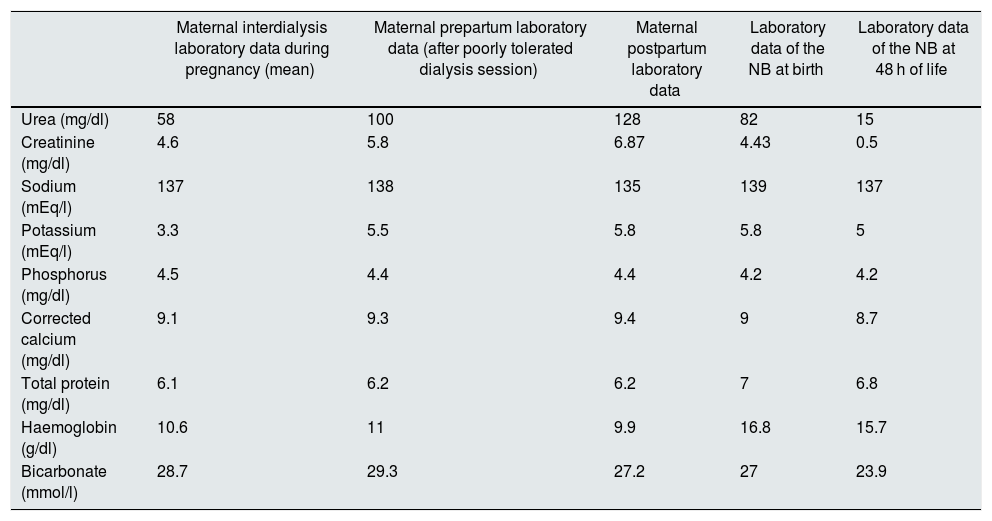
At week 36 + 2, the patient was referred to the reference hospital for prodromal labour. A prepartum haemodialysis session was administered, with poor haemodynamic tolerance requiring the discontinuation of the dialysis session ; then the induction of vaginal delivery with prostaglandins and oxytocin was started, but, in the absence of progression, an urgent caesarean section was performed, resulting in a live newborn of 2970 g, without pathological signs on examination and diuresis preserved at all times. Given the mother’s situation, on haemodialysis and with uncontrolled uraemia, laboratory tests were performed on the NB and it was found that creatinine was elevated (4.43 mg/dl), urea was 82 mg/dl, sodium was 139 mEq/l, potassium 5.8 mEq/l, phosphorus 4.2 mg/dl and bicarbonate 27 mmol/l. Two days after birth, without the need for treatment, these values were normalised in the NB (Table 1), and remained in nrmal range in subsequent follow-ups.
Laboratory test results and their progression.
| Maternal interdialysis laboratory data during pregnancy (mean) | Maternal prepartum laboratory data (after poorly tolerated dialysis session) | Maternal postpartum laboratory data | Laboratory data of the NB at birth | Laboratory data of the NB at 48 h of life | |
|---|---|---|---|---|---|
| Urea (mg/dl) | 58 | 100 | 128 | 82 | 15 |
| Creatinine (mg/dl) | 4.6 | 5.8 | 6.87 | 4.43 | 0.5 |
| Sodium (mEq/l) | 137 | 138 | 135 | 139 | 137 |
| Potassium (mEq/l) | 3.3 | 5.5 | 5.8 | 5.8 | 5 |
| Phosphorus (mg/dl) | 4.5 | 4.4 | 4.4 | 4.2 | 4.2 |
| Corrected calcium (mg/dl) | 9.1 | 9.3 | 9.4 | 9 | 8.7 |
| Total protein (mg/dl) | 6.1 | 6.2 | 6.2 | 7 | 6.8 |
| Haemoglobin (g/dl) | 10.6 | 11 | 9.9 | 16.8 | 15.7 |
| Bicarbonate (mmol/l) | 28.7 | 29.3 | 27.2 | 27 | 23.9 |
Uraemic toxins in women on haemodialysis can trigger systemic foetal poisoning, with underdevelopment of organs and tissues, delayed cell proliferation, intrauterine growth reduction, polyhydramnios and immature lung which is manifested by respiratory failure at the time of delivery. Therefore, a “normal” environment for the foetus, free of accumulated toxins, is essential. To maintain the predialysis urea nitrogen level below 50 mg/100 ml,5,6 it is recommended that patients should be dialysed for as long as possible, preferably more than 24 h per week. It seems that six weekly sessions lasting four hours are more beneficial than longer sessions with less weekly frequency and, at the time of delivery, try to dialyse the patient on the same day od delivery.4
What was interesting in our case was the new born’s analytical presentation that reflected the maternal one that did not complete the haemodialysis session prior to delivery, without complications of the new born secondary to uraemia and with spontaneous normalisation of biochemical parameters.
We therefore conclude by pointing out the importance of maintaining adequate dialysis during pregnancy and of carrying out a last session as close to delivery as possible to avoid analytical alterations in the new born, as well as possible complications of poor maternal blood clearance, which in our case did not require any type of measure for the new born. We also emphasise the importance of recording these experiences in order to achieve a higher rate of success and maternal-foetal survival, since information on the management of these patients and their newborns is still scarce.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Borrego García E, Díaz Gómez L, Navas-Parejo Casado A, Prados Garrido MD. Parámetros bioquímicos de un recién nacido de madre en hemodiálisis tras sesión inadecuada. Descripción de un caso. Nefrologia. 2021;41:480–482.