Acute kidney injury (AKI) is a common and significant complication in patients with liver failure (LF).1 AKI related to increased bilirubin levels has been well known since the beginning of the 20th century. This condition has received different names: cholestatic nephropathy, jaundice-related nephropathy, bile cast nephropathy and bile nephropathy.1–4
We present an unusual case of AKI due to severe hyperbilirubinaemia caused by anabolic steroids (AS) used for body-building. This is a 40-year-old man, with no previous medical history of interest, who came to the clinics for symptoms of jaundice, hypocholia, choluria, itching and asthenia. The patient presented with no substance abuse and reported that he had been taking Animal-Pak® and EA Havoc® vitamin supplements the previous month.
On physical examination, the only thing of note was a marked mucocutaneous jaundice. The tests on admission showed bilirubin: 30mg/dl, GPT: 226U/l, GOT: 89U/l and alkaline phosphatase and gamma-GT within normal range. He did not show coagulopathy and renal function was normal. Viral serologies, alpha-1-antitrypsin, ceruloplasmin, copper, antibodies, immunoglobulins and complement were normal, as was the abdominal ultrasound.
His clinical course showed a progressive increase in bilirubin to a peak of 39.9mg/dl. A liver biopsy was performed, showing areas of periportal hepatitis, canalicular and parenchymal cholestasis and perisinusoidal fibrosis; findings consistent with drug-induced hepatitis. Bilirubin levels gradually improved, reaching a bilirubin concentration of 30mg/dl at the time of discharge.
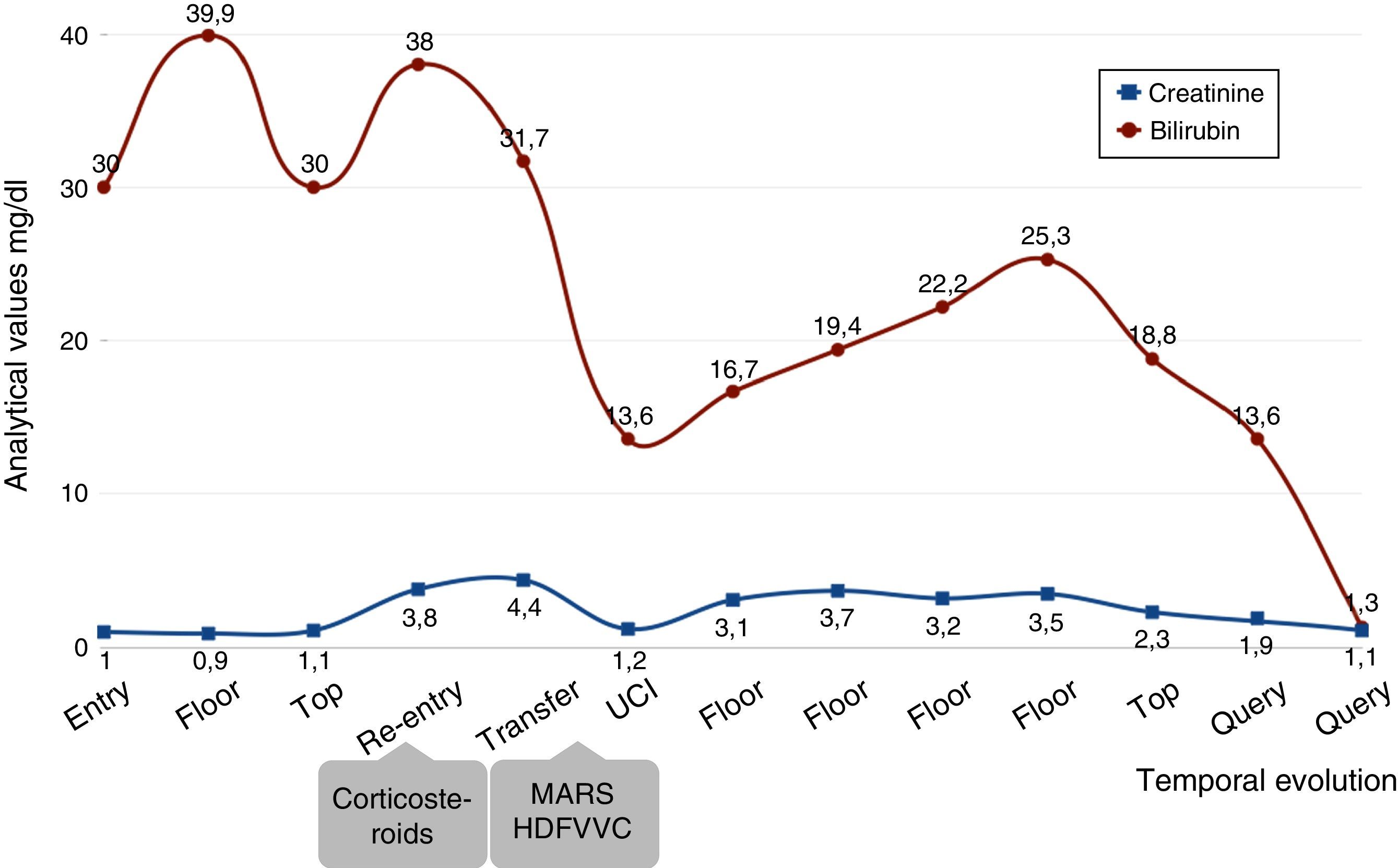
A week after being discharged the patient was admitted for AKI with serum creatinine (SCr) of 4.5mg/dl and bilirubin levels, which had increased, to 38mg/dl (Fig. 1). In light of these findings, treatment started with fluid replacement therapy, ursodeoxycholic acid, cholestyramine resin and corticosteroids (1mg/kg), the bilirubin levels decreased to 30mg/dl, but with AKI persisted, so haemodialysis was started followed by Molecular Adsorbents Recirculation System (MARS) therapy and continuous venovenous haemodiafiltration (CVVHD).
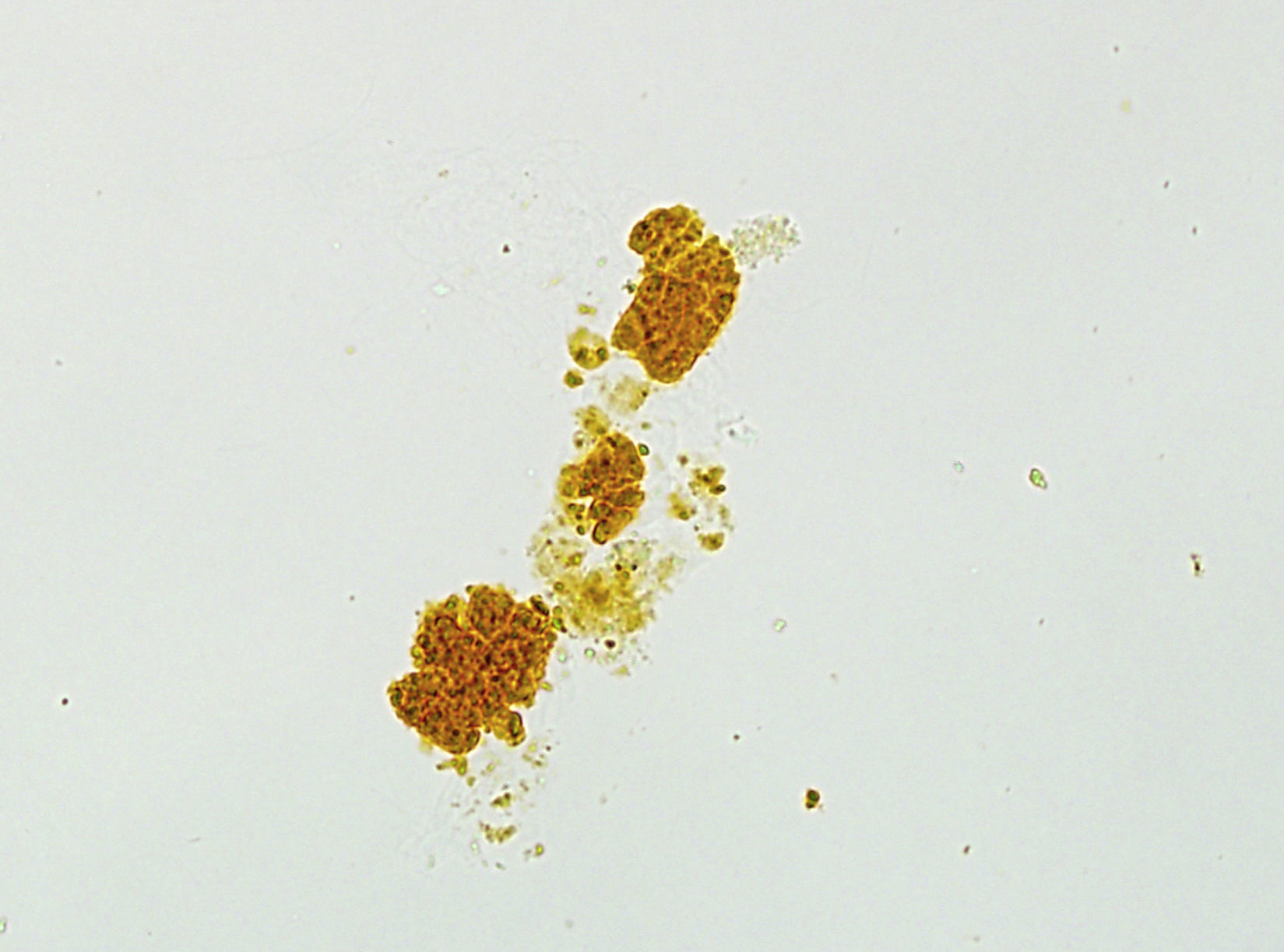
A complete renal evaluation was performed showing only the presence of abundant bilirubin casts in the sediment (Fig. 2). Subsequently, bilirubin levels gradually improved to 18.8mg/dl in parallel with the treatment, and corticosteroids were gradually decreased and MARS and CVVHD were withdrawn. Kidney function improved to a SCr of 2.4mg/dl at the time of discharge, so it was decided not to perform a renal biopsy. Four months after the onset of symptoms, the patient reached a SCr of 1.1mg/dl with a bilirubin level of 1.3mg/dl, with steroids being suspended two months after their introduction.
AS are synthetic derivatives of testosterone and can cause liver toxicity (cholestasis, nodular regenerative hyperplasia, neoplasms, etc.) as they alter the canalicular excretion of conjugated bilirubin and its sinusoidal uptake, causing it to accumulate.2,5 The patient had been taking Havoc®, which contains methylepitiostanol, a prohormone that is metabolised to produce the compound desoxymethyltestosterone. This compound can cause liver cholestasis, which is one of the reasons its sale has been banned.6
From a renal perspective, proteinuria associated with focal segmental glomerulosclerosis and AKI has been reported.2,5 Robles-Díaz et al. reported a series of 25 patients with hepatotoxicity due to AS, 31% of which developed AKI with full recovery of kidney function after the liver damage had been resolved without the need for renal biopsy.7
Bilirubin increases in the sinusoid in LF which can cause direct tubular damage, and therefore AKI. It is known that the risk of tubular injury increases when the bilirubin levels are higher than 20mg/dl.1,2,5,8,9 Bilirubin is transported in the proximal tubule; when it is saturated it leads to the formation of casts which cause tubular damage, either from the direct toxicity of the bilirubin or from the intratubular obstruction of the casts.1,8 The mechanisms responsible for the tubular damage are the uncoupling of the mitochondrial phosphorylation, thereby decreasing ATPase activity, oxidative damage of the tubular cell membrane, and the inhibition of Na+−H+, Na+−Cl− and Na+−K+2,10 pumps.
Diagnosis requires clinical suspicion and a urinary sediment test needs to be carried out, which typically shows bilirubin casts and epithelial cells containing bilirubin.9 Tubules full of degenerated epithelial cells and bile pigment casts together with dilation of the lumen and cytoplasmic vacuolisation with glomerular integrity are usually found in the kidney biopsy.3,4 In the electron microscope study it is typical to find dilated mitochondrial cristae and an accumulation of bile acids within the lysosomes.8
Treatment is not specific and is fundamentally supportive. Renal replacement therapy has no specific role except for the treatment of AKI, while plasmapheresis may have a use in reducing pro-inflammatory substances.9 Other options aimed at reducing inflammatory cytokines and bilirubin are MARS, Coupled Plasma Filtration Adsorption (CPFA) and plasma filtration adsorption dialysis. Steroids, cholestyramine, ursodeoxycholic acid and lactulose have demonstrated minimal benefit.8 AS can cause these symptoms, so amateur athletes should be informed about their side-effects.
Please cite this article as: Milla Castellanos M, Gutiérrez Martínez E, Sevillano Prieto A, Rodríguez Ramos P, Praga Terente M. Nefropatía por cilindros biliares asociada a disfunción hepática severa causada por esteroides anabolizantes. Nefrologia. 2018;38:221–223.