Henoch–Schönlein purpura (HSP) is a generalized vasculitis, which could cause a large variety of symptoms in different organs. Acute pancreatitis is an inflammatory disorder and may be life-threatening if it is severe. HSP could cause the acute pancreatitis rarely. It tends to develop in the first week of the illness after characteristic purpura, or develop later.1 Exceptionally, acute pancreatitis developed during the course of HSPN as an initial presenting feature before the typical rash. Here we report an adult patient with HSPN presenting after the acute pancreatitis.
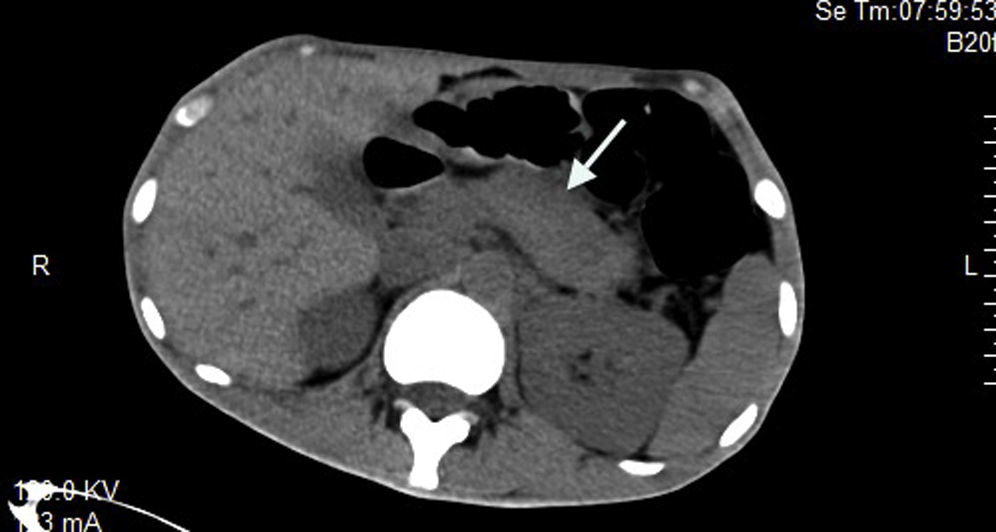
A 19-year-old man was admitted to our hospital with the chief complaint of “abdominal pain and abnormal urine test for 1 month, erythematosus purpura over legs for 5 days”. He received the treatment for pancreatitis in the local hospital. However, the pancreatitis did not get remission. On admission of our hospital, the patient had a normal blood pressure and respiratory rate. There was a diffuse purpuric rash located over the legs. Abdominal examination showed tenderness in all quadrants with rebound tenderness. There was no hepatosplenomegaly, and bowel sounds were normal. Blood testing showed hemoglobin (101g/l), white cell count (19.6×109g/l), neutrophil (9.7×109g/l). Erythrocyte sedimentation rate and C-reactive protein were significantly high at 29mm/h and 100.3mg/l, respectively. Serum testing showed glucose (3.3mmol/l), urea (6.31mmol/l), creatinine (52umol/l), albumin (28.5g/l), total cholesterol (4.1mmol/l), and triglyceride (1.6mmol/l). Serum amylase (332U/l) and lipase (85.2U/l) were increased. Urinary sediment examination showed microscopic hematuria. The proteinuria of 24h is 2.48g/2L. Rheumatoid factor and complements (C3, C4) were within the normal range, and antinuclear antibodies, anti-DNA, antiphospholipids, antineutrophil cytoplasmic antibodies, and hepatitis viral markers were negative. Abdominal ultrasound showed a peritoneal effusion. Abdominal computed tomography (CT) scan noted an edematous pancreas (Fig. 1).
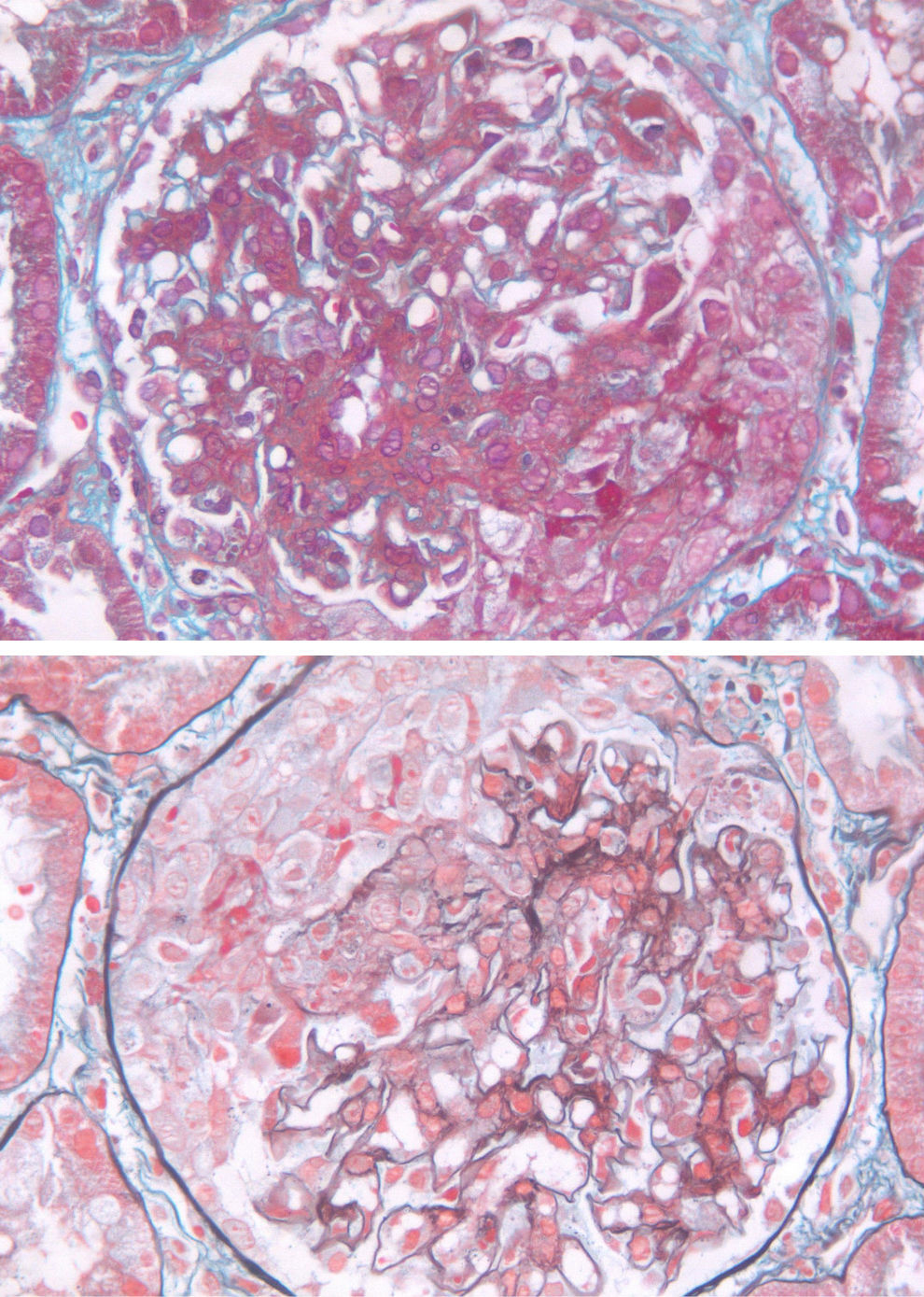
The result of renal biopsy was focal proliferative necrotizing purpura nephritis. Focal granular staining for IgA and C3 in the mesangium was shown using immunofluorescence staining. By light microscopy, glomeruli showed a mild hypercellularity in mesangial cells and matrix, focal endocapillary hypercellularity, eight crescents of 10 glomerulis, 1 necrosis of capillary loop. There is interstitial edema and inflammation composed mainly of mononuclear leukocytes and tubular epithelial injury (Fig. 2). The result of the light microscopy was confirmed by the electron microscopy.
The patient was diagnosed as purpura nephritis complicated by acute pancreatitis. He was started on therapy with methylprednisolone 40mg/d intravenously for 5 days before the renal biopsy result. Afterwards, 0.5g bolus of methylprednisolone was given intravenously for 3 days and after that prednisone orally (30mg/day) and MMF orally (1.5mg/day). Abdominal pain disappeared at the third day of the treatment and the pancreas was normal after two weeks’ treatment. After 1-year follow-up, the patient recovered well with prednisone (10mg/day) and MMF (0.25mg/d), and renal function was normal, proteinuria was less than 150mg/day, and abdominal CT scan was normal.
The association between pancretitis and Henoch–Schönlein Purpura Nephritis is rare. In our case, purpura nephritis complicated by acute pancreatitis was showed in this 19-year-old man. HSP is a rare cause of acute pancreatitis that can occur before or after the characteristic rash. In our case, the symptoms occurred before the rash. The pancreatitis tends to develop on the first day of the illness but may develop as late as day 75.2 Acute pancreatitis is presumed to be caused by vasculitic involvement of the pancreas.
The clinical feature of HSP nephritis is quite variable. The pathology of this patient showed a mild hypercellularity in mesangial cells and matrix, focal endocapillary hypercellularity, eight crescents of ten glomerulis, 1 necrosis of capillary loop. In the literature, only two cases got renal biopsy of purpura nephritis with pancretitis. One case showed moderate-to-severe increase of mesangial matrix with crescent formation3 and one case showed endocapillary proliferative glomerulonephritis.2 There is no special feature in the pathology of those patients.
Steroids have been used to treat HSP patients with pancretitis.4–7 For most HSP related pancretitis without nephritis, parenteral nutrition and Nasogastric suction was used to treat the pancretitis,8,9 and the outcome of pancretitis improved. In our case, the patient's pancretitis did not improve with the supportive treatment; however, the symptoms of pancretitis disappeared with the steroids usage. In the literature, two patients were diagnosed as HSP related pancretitis with nephritis. In the study by Frirui et al., kidney biopsy showed endocapillary proliferative glomerulonephritis and the patient was given 1g bolus methylprednisolone intravenously for 3 days and after that prednisone orally (60mg/day).2 And in the study by Nie et al., as HSP nephritis (severe) was confirmed, intravenous methylprednisolone (500mg/d) was given to the patient for 3 days followed by oral dehydrocortisone of 30mg/d.3 The two patients got complete remission in pancreas and kidney.
HSP is a rare and benign cause of acute pancreatitis. This complication could occur before the characteristic rash and shown as an initial manifestation of HSPN. Steroids could improve the outcome of the HSPN patients with pancreatitis.