Antecedentes: la presencia de acético en el Líquido de Diálisis (LD) expone al paciente a una concentración de acetato 30-40 veces superior a la normal. Dicha exposición aumenta en técnicas de Hemodiafiltración (HDF) online. El objetivo de dicho estudio fue evaluar los cambios clínico-analíticos al usar tres técnicas de Hemodiálisis (HD) diferentes. Métodos: se reclutaron 35 pacientes en HD estable. Se dializaron tres meses con HD convencional y luego fueron aleatorizados para pasar a una técnica de PHF on-line con concentrado convencional seis meses, y después pasaron a PHF on-line sin acetato otros seis meses. El otro grupo invertía estos dos períodos. Se obtuvieron análisis de sangre y datos clínicos de HD. Resultados: las medias de los acetatos posdiálisis fueron significativamente superiores durante los períodos de tratamiento con acético respecto al período sin acetato. El porcentaje de valores patológicos de acetato posdiálisis fue significativamente superior durante los períodos de tratamiento con acético (61 respecto al 30%). Las concentraciones de cloro pos-HD fueron superiores y las de bicarbonato pre y pos-HD fueron menores durante el período sin acético. El número de hipotensiones fue significativamente inferior en el período de PHF on-line con LD estándar respecto a los otros períodos. Conclusiones: la técnica de PHF on-line sin acetato disminuye la exposición a concentraciones elevadas de acetato y consigue que la mayoría de pacientes termine la HD con una acetatemia en el rango fisiológico. La PHF on-line es un tratamiento de HDF predilucional con mejor tolerancia que la HD estándar con bicarbonato.
Summary Background: the small quantity of acetate present in the dialysis fluid exposes patient’s blood to an acetate concentration 30-40 times the physiological levels. This amount is even greater in hemodiafiltration on-line. Our purpose was to evaluate the clinical-analytical effects using three different dialysis techniques in the same patient. Methods: 35 patients on hemodialysis were included. All patients were treated with conventional bicarbonate dialysate for 3 months, after randomization were switched to first be treated with PHF online with standard bicarbonate dialysate for 6 months and then switched to PHF on-line acetate-free dialysate for the other 6 months or to invert the two last periods. Blood samples were drawn monthly throughout the study and clinical data were obtained. Results: Posdialysis blood acetate levels were higher in patients treated with conventional bicarbonate dialysate with respect to the period of PHF with free-acetate dialysate. Moreover, the percentage of patients with posdialysis blood acetate levels in the pathologic range was higher in patients treated with conventional bicarbonate dialysate respect to PHF on-line acetate-free dialysate period (61% vs. 30%). Serum concentrations of chloride posdialysis were higher and serum concentrations of bicarbonate pre and poshemodialysis were lower in the PHF free-acetate period. The incidence of hypotensive episodes was significantly lower in the PHF on-line with conventional dialysate. Conclusions: PHF on-line with free-acetate dialysate allows that most of patients finished hemodialysis with blood acetate levels in the physiologic ranges. PHF on-line is a predilutional hemodiafiltration treatment with better tolerance than hemodialysis with standard bicarbonate dialysate.
INTRODUCTION
In recent years there have been significant changes within the field of HD, including new dialysis techniques, filters and dialysis solutions. In terms of the dialysis fluid (DF), tolerance of dialysis can be improved by reducing the quantity of acetate in the concentrate from 35-40 to 3-4mmol and use of a bicarbonate buffer.1,2 These small quantities of acetic acid present in the DF, which are required to maintain a pH between 7.1 and 7.4 and prevent salt precipitation, expose the patient to an acetate concentration 30-40 times higher than normal.3,4 Recently, an acetate-free dialysis concentrate has been produced in which hydrochloric acid (HC1) replaces acetic acid thus protecting patients from abnormal levels of acetate.4,5 Chronic hyperacetatemia, which is found in some HD patients, may be controlled using acetate-free dialysate.4
In terms of HD technique, convective therapies are associated with better tolerance and clearance of larger molecules as compared with conventional HD treatments.6 These techniques have shown good cardiovascular stability with the use of more biocompatible membranes and ultrapure endotoxin-free dialysate. Recently, a new pre-dilution convectional technique has been described on-line PHF, which uses a double chamber dialyser and allows reinfusion of large amount of substitution fluid than conventional post-dilution techniques.7,8 On-line PHF has proven to be a safe technique in both children and adults allowing greater β2-microglobulin clearance with good clinical tolerance.9,10
The purpose of this study was to evaluate and compare the changes in biochemical and clinical data during dialysis by subjecting the same patient to three different dialysis techniques: high-flow HD, on-line PHF with conventional dialysate and on-line PHF with acetate-free DF, using HCl.
PATIENTS AND METHODS
Patients
Thirty-five clinically stable HD patients (20 men and 15 women) from six level-3 hospitals in Spain (Madrid, Córdoba, Santander and Barcelona) were selected for the study. All patients gave informed consent to participate in the study and the study was approved by the six hospitals’ ethics committees.
The inclusion criteria were as follows: aged over 18; undergoing HD for more than three months who were stable on three weekly sessions of 3 to 5 hours a stable regimen of anticoagulation and erythropoietin; haematocrit higher than 28% and vascular access allowing flows greater than 250ml/min.
Patients with known coagulation problems were excluded from the study as were those with a survival rate lower than 18 months or with significant residual renal function (diuresis greater than 400ml/day or creatinine clearance > 2ml/min).
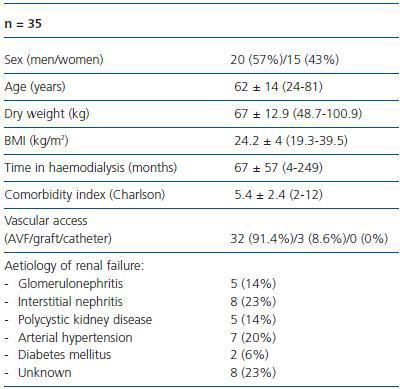
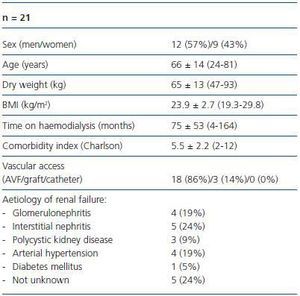
The patients had a mean age of 62 ± 14 years (range 24-81) and the mean duration of HD treatment was 67 ± 57 months (range 4-249) (table 1a).
The aetiology of renal failure was glomerulonephritis (n = 5); interstitial nephritis (n = 8); polycystic kidney disease (n = 5); arterial hypertension (n = 7); diabetes mellitus (n = 2); and unknown (n = 8).
The Charlson comorbidity index was 5.2 ± 2.4 (range 2-12), (table 1a).
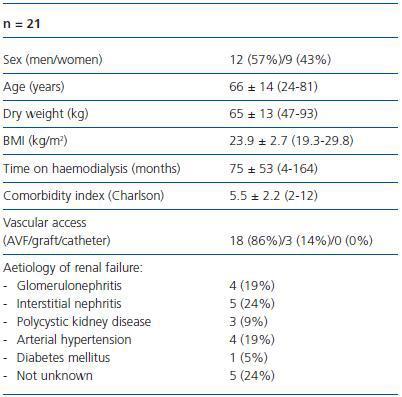
Table 1b shows the characteristics of the 21 patients who completed the study. There were no significant differences between the 35 patients selected and the 21 who completed the study.
Dialysis technique and study design
All patients underwent dialysis for 3-4 hours thrice weekly using conventional bicarbonate concentrate with acetate (BHD3 A4, Fresenius Medical Care, Bad Homburg, Germany or Dialisan-Bicart Ca 30, Hospal, Lyon, France). All HD machines were equipped with endotoxin filters (Bellco, Mirandola, Italy). Daily diuresis was less than han 150ml/24 hours and mean dry weight was 65.2 ± 13kg (47-100). The mean Kt/V (Daugirdas 93) was 1.26 ± 0.24, the mean Qb was 345 ± 40ml/min, the Qd was fixed for all at 500ml/min. Interdialytic weight gain was 1.8 ± 0.75kg.
Total mean conductivity was 13.9 ± 0.1ms/cm and mean bicarbonate conductivity was 3.1 ± 0.1ms/cm and both remained constant for all patients during the study. The temperature of the DF was fixed at 36º C for all patients in all the centres during the study. All patients used high permeable synthetic membranes during the first three months of the study. When the technique was changed to on-line PHF, the membranes were substituted by double chamber polyethersulfone dialysers. The mean volume of liquid infused during pre-dilution was 10L/hour.
All the patients underwent conventional HD for three months and one group was then randomised to on-line PHF technique using a conventional concentrate with bicarbonate for six months and then changed to on-line PHF with acetate-free concentrate (611 free-acetate, Bellco, Mirandola, Italy). The other group reversed these two periods. The patients were randomised by centre and allocation order. Blood tests were performed monthly throughout the study. Clinical data was collected during 13 consecutive sessions at baseline and at 3, 6, 9, 12 and 15 months.
The three techniques used during the study were performed using the Formula dialysis machine (Bellco, Mirandola, Italy).
HD tolerance was evaluated as in terms of number of hypotensive episodes, headaches, pruritus, vomiting or cramps per month.
Episodes of hypotension were defined as a fall in systolic blood pressure, below 95mmHg associated with symptoms requiring the intervention of healthcare professionals.
Monthly blood tests performed pre and post-HD included urea, creatinine, sodium, potassium, chloride, bicarbonate, acetate, calcium, phosphate, glucose, albumin, β2-microglobulin and C-reactive protein (CRP). The latter was analysed using nephelometry (ultrasensitive CRP, Behring Diagnostics, GMBH, Rarburg, Germany) with a detection limit of 0.1mg/ml and a reference range between 0.1 and 0.4mg/L. The coefficient of variation was lower than 4%.
The following were measured pre-dialysis: uric acid, total cholesterol, HDL cholesterol, triglyceride, total proteins, prealbumin, ferritin, transferrin saturation index, serum iron, parathyroid hormone, haematocrit, haemoglobin, fibrinogen and homocysteine.
Serum acetate was determined by the ultraviolet radiation method. The enzymatic reaction in acetate synthesis results in the formation of NADH+ measured as an increase in absorbency. Normal values in the healthy population were lower than 0.1mmol/L with a detection limit of 0.01mmol/L.
Preparing the acetate-free DF
All the electrolytes, except from bicarbonate, were present on the concentrate.The acetic acid was substituted by HCl (Bellco-Soludia, Fourquevaux, France). The pH of the concentrate was then less than 1.
Statistical analysis
The data are expressed as mean ± standard deviation. The Kolmogorov-Smirnov test was used to evaluate the normal distribution of the variables. All the variables had normal distribution with the exception of CRP which had an exponential curve and required logarithm transformation. For parametric variables, the paired t-test was used for two measurements and the ANOVA test for more than two.
For non-parametric variables, the Wilcoxon test was used for two measurements and the Dunett’s test for more than two. The Friedman test was used to evaluate the effect of the different treatments on HD tolerance.
The X2 test was used for categorical variables. All the data were analysed using the SPSS version 12. Statistical significance was defined as p < 0.05.
RESULTS
The study lasted 15 months.
Of the 35 patients 30 were randomised. Of these four died, five received a kidney transplant and 21 completed the study.
During the first six months, 12 patients were randomised to on-line PHF with conventional DF and 18 patients were randomised to on-line PHF with acetate-free DF. The groups then switched to the alternative treatment for a further 6 months.
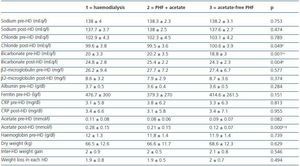
No significant differences were found in the biochemical parameters, except for post-dialysis chloride level and pre and post-dialysis bicarbonate. Dry weight and interdialytic weight gain remained stable during the entire study (table 2).
The pre-dialysis plasma acetate levels during the conventional HD treatment period and the acetate-free on line PHF ± standard deviation of the concentrate did not differ statistically from the group treated with on-line PHF with HCl concentrate (0.10 ± 0.09 vs. 0.09 ± 0.07mmol/L, p = ns), while the post-dialysis acetate levels were significantly higher during the treatment period with acetic acid concentrate in comparison to the treatment with HC1 concentrate (0.24 ± 0.16 vs. 0.15 ± 0.13, p = 0,000) (table 2).
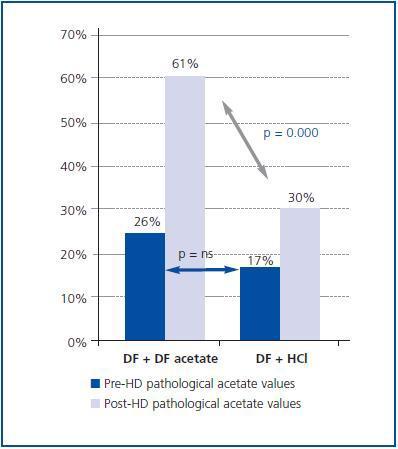
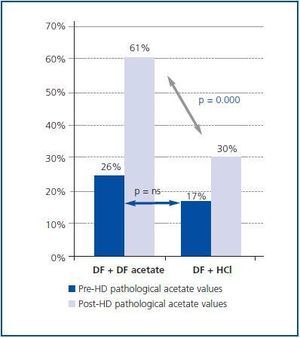
There were no significant differences in the nonphysiological values of acetate in pre-dialysis (26% of patients using DF with acetate, 17% of patients using DF with HC1, p = ns). There were however significant differences between the two treatment periods (with or without acetate) regarding the presence of pathological values of acetate in post-dialysis (61% of patients using DF with acetate vs 30% of patients using DF with HC1, p = 0.000) (figure 1).
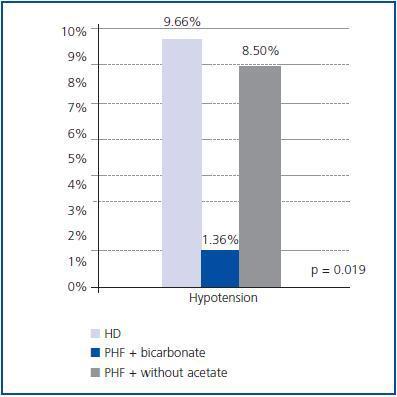
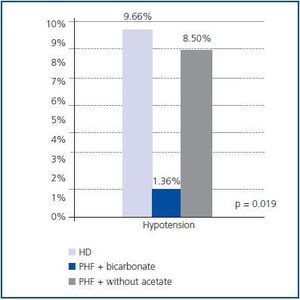
On-line HDF with conventional DF was associated with fewer hypotensive episodes than treatment with conventional HD or on-line PHF without acetate (p = 0.019), (figure 2). There was no difference in the remaining parameters for dialysis tolerance between the groups but the symptoms were very low throughout the study.
No significant differences were found in the β2-microglobulin reduction rate between conventional HD and convective techniques (table 2).
DISCUSSION
With the widespread use of dialysis in patients with multiple co-morbidities (diabetics, advanced age, cardiovascular complications) there is a need for more efficient (better clearance of larger uraemic toxins) and well tolerated (more biocompatible) dialysis techniques.
In recent years, pre and post-dilution convective techniques and acetate-free techniques such as acetate-free biofiltration (AFB) led to an improvement in haemodynamic tolerance, correction of the acid-base balance, clearance of larger molecules and greater biocompatibility (ultrapure water) in comparison with conventional HD.6,11 The present study did not find greater clearance of β2-microglobulin with convective treatment in comparison with conventional HD, however this may be explained by insufficient volumes of pre-dilution reinfusate.
When the study was performed, the Formula machine did not allow infusion flows greater than 160ml/min for on-line HDF. This meant that the volume infused was limited to between 28.8 and 38.4L. The comparable volume, in terms of the clearance of medium molecules such as ‚β2-microglobulin, is 20L in post-dilution HDF, which would be approximately 60L in pre-dilution HDF.12
As expected, the acetate-free on-line PHF allows the majority of patients to complete treatment with post-HD acetatemia within the physiological range in comparison with the other two techniques which use conventional concentrate with 4mmol/L of acetate. These results are in agreement with other studies, whether using conventional HD and DF with or without acetate or pre-dilution HDF using DF with or without acetate.4,5,13
Recently, Pizzarelli et al.5 reported that the gain in acetate is particularly high in convective treatments and that the plasma levels of acetate return to baseline levels two hours after completing the treatment. In our study, we found no differences in the pre-dialysis values using the concentrate with or without acetate supporting the finding of temporary hyperacetatemia.
In this study, there was a reduction in the levels of bicarbonate, pre and post-dialysis, in patients using the acetate-free concentrate. Once in the body, the acetate converts to bicarbonate. Thus, in a patient with bicarbonate levels of 20mmol/L in the plasma pre-dialysis, who undergoes HD with a conventional DF, containing 4mmol/L of acetic acid, in the final positive balance of buffer, approximately 25% corresponds to acetic acid and its metabolisation. With the new acetate-free DF, this component does not exist and therefore to achieve a similar balance the concentration of bicarbonate in the DF needs to be increased, raising its partial conductivity. We suggest that this needs to be increased by 0.2mS/cm, as proposed by Pizzarelli et al. in their study.14
It is known that the acetate induces hypotension by causing vasodilatation and myocardial depression. When we changed from a conventional HD to the convective technique using a standard concentrate, the number of hypotensive episodes was reduced. However it was surprising that when we used acetate-free on-line PHF technique the number of hypotensive episodes increased again (as in the conventional HD treatment period). One possible explanation for this phenomenon may be that the lower supply of bicarbonate in the acetate-free dialysate group was not compensated for by increasing the bicarbonate conductivity in the machine and, therefore, the tendency towards acidosis resulted in poorer tolerance in the convective technique. In addition to this, the concentration of sodium in the DF has a direct and significant influence on tolerance of dialysis. The ratio between sodium concentration and final conductivity decreases due to the increased concentration of chloride in this new DF. Chloride has a high ionic strenght which significantly contributes to conductivity, with higher strenght than that of acetic acid. Since the machine adjusts dilution based on final conductivity, the increased chloride is compensated with greater dilution of the other elements, with greater proportional influence on sodium. To maintain sodium concentration in acetate-free DF we have to increase the total final conductivity by 0.2mS/cm. It is important to remember that if these adjustments are not made, the patient dialysing with the new acetate-free DF will be more acidotic and the dialysate will have less sodium.
Among the multiple factors influencing anaemia in renal failure, is the existence of molecules that accumulate during uraemia which inhibit erythropoiesis.15 By clearing particles of greater molecular weight, convective techniques allow better control of anaemia and a reduced dose of erythropoietin.16 In addition it is known that acetate is a promoter of inflammation and this in turn reduces the response to erythropoietin. We did not find any changes in haemoglobin levels or erythropoietin requirements after changing from conventional HD to the convective technique with or without acetate.
It has been suggested that the repeated increase in acetatemia during the dialysis sessions is part of the chronic inflammation presented by patients with renal failure in HD. The exposure to small amounts of acetate during conventional HD is able to induce the production of cytokines by activated polymorphonuclear leukocytes, demonstrated by increased TNF synthesis, serum levels of IL-1‚ and nitric oxide synthetase activity.17-19 The inflammatory parameters evaluated during the study, such as CRP, ferritin and/or albumin, were not modified following the change in technique and/or dialysate. The duration of the study and the small sample size (21/30 patients selected completed the study) may have been insufficient to detect significant changes in these parameters.
It is also to be noted that the sample of patients who participated in this study is not representative of the global HD population since, by including patients with good vascular access allowing high blood flows, a population with low prevalence of diabetes mellitus was selected and catheters for vascular access were excluded.
CONCLUSIONS
The on-line PHF technique using an acetate-free concentrate prevents exposure to high concentrations of acetate with the patient achieving the end of the HD session levels of acetatemia within the physiological range. On-line PHF is a pre-dilution PHF treatment with greater tolerance than conventional HD using bicarbonate, that requires high volumes of replacement liquid to achieve effective clearance of molecules with greater molecular weight such as β2-microglobulin. Improvement in tolerance of dialysis may be achieved by the addition of acetate-free DF, but this should be accompanied by increased bicarbonate conductivity (+0.2mS/cm) and total conductivity (+0.2mS/cm) in the HD machine.
Acknowledgement
To Sorin Group.
Table 1a. Characteristics of the patients selected for the study
Table 1b. Characteristics of the patients who completed the study
Table 2. Monitoring of different biochemical parameters pre and post-dialysis
Figure 1.
Figure 2.