The occurrence of pregnancy in women with Chronic Kidney Disease (CKD) is unusual and these women are prone to more complications, especially among those on dialysis. Nevertheless, the high rate of complications such as hypertension, polyhydramnios, pre-eclampsia, restricted intrauterine growth and preterm birth make this physiological state a challenge in women with advanced CKD.
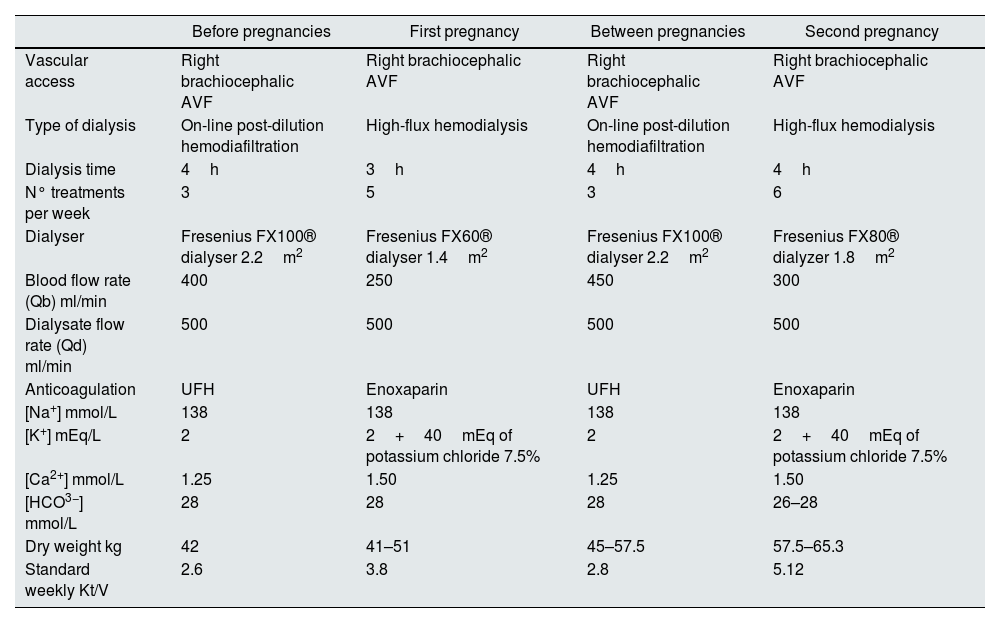
We report a case of a 29-year-old female patient with an obstetric history of a fetal loss at 31 weeks of gestation at the age of 18, in the sequence of an unsupervised pregnancy, diagnosed with gestational hypertension and severe pre-eclampsia at the time of delivery. At the age of 20, she presented with hypertension associated with thrombotic microangiopathy which required hemodialysis initiation. She was followed up as an outpatient in our hemodialysis department with dialysis prescription described in Table 1. Additional medical history of anemia and mineral bone disease associated with CKD controlled with darbopoetin, intravenous iron and vitamin D analogs.
Dialysis prescription.
| Before pregnancies | First pregnancy | Between pregnancies | Second pregnancy | |
|---|---|---|---|---|
| Vascular access | Right brachiocephalic AVF | Right brachiocephalic AVF | Right brachiocephalic AVF | Right brachiocephalic AVF |
| Type of dialysis | On-line post-dilution hemodiafiltration | High-flux hemodialysis | On-line post-dilution hemodiafiltration | High-flux hemodialysis |
| Dialysis time | 4h | 3h | 4h | 4h |
| N° treatments per week | 3 | 5 | 3 | 6 |
| Dialyser | Fresenius FX100® dialyser 2.2m2 | Fresenius FX60® dialyser 1.4m2 | Fresenius FX100® dialyser 2.2m2 | Fresenius FX80® dialyzer 1.8m2 |
| Blood flow rate (Qb) ml/min | 400 | 250 | 450 | 300 |
| Dialysate flow rate (Qd) ml/min | 500 | 500 | 500 | 500 |
| Anticoagulation | UFH | Enoxaparin | UFH | Enoxaparin |
| [Na+] mmol/L | 138 | 138 | 138 | 138 |
| [K+] mEq/L | 2 | 2+40mEq of potassium chloride 7.5% | 2 | 2+40mEq of potassium chloride 7.5% |
| [Ca2+] mmol/L | 1.25 | 1.50 | 1.25 | 1.50 |
| [HCO3−] mmol/L | 28 | 28 | 28 | 26–28 |
| Dry weight kg | 42 | 41–51 | 45–57.5 | 57.5–65.3 |
| Standard weekly Kt/V | 2.6 | 3.8 | 2.8 | 5.12 |
AVF: arteriovenous fistula; UFH: unfractionated heparin.
Five months after starting hemodialysis, she was found to be pregnant on a routine abdominal ultrasound, with an estimated gestational age of 12 weeks. At the time, she was passing 1000mL of urine a day and had a dry-weight of 42kg. Immediately, dialysis prescription was changed to a 20hours a week, as shown in Table 1. Pre-dialysis urea values were kept under 60mg/dL, potassium levels between 4.2 and 5.3mg/dL, blood pressure maintained under 140/90mmHg and dry weight was gradually incremented. An increment of dialysis time was proposed to the patient, but she promptly refused. Prenatal care and follow-up were carried out at the Obstetric Unit, with frequent ultrasound checks excluded fetal malformations. At 36 weeks of gestation she was submitted to a programmed cesarean section for pelvic presentation with active contractility. The newborn had a birthweight of 2375g an Apgar score of 9 at 0′ and 10 at 5′ and normal neonatal development.
After delivery patient returned to similar dialysis prescription (Table 1). Also, she always refused a kidney transplant and there was suspicion of poor therapeutic adherence. Nine years later, she presented with amenorrhea for three consecutive months, and pregnancy was confirmed after the detection of beta-subunit of human chorionic gonadotropin (11568mUI/mL). Fetal ultrasound showed an embryo with an estimated gestational age of 4/5 weeks. At the time, she was passing 500mL of urine a day and had a dry weight of 57.5kg. This time, the total weekly dialysis time was increased to 24h per week (Table 1). Pre-dialysis urea values were kept under 30mg/dL. Blood pressure was difficult to control and varied between 130–180/60–100mmHg. She was held on close obstetric monitoring, and at 25 weeks and 5 days of pregnancy she was referred to the Obstetrics Emergency Service due to decreased fetal movements and, after the diagnosis of fetal growth restriction, she was hospitalized for fetal pulmonary maturation and fetal surveillance. At 26 weeks and 4 days of pregnancy, an emergent cesarean section was performed due to a suspicion of placental abruption. With a birthweight of 660g, and an Apgar score of 6 at 0′ and 7 at 5′ and 8 at 10′, the newborn required prolonged hospitalization in the neonatal intensive care unit, which was uneventful and showed good neonatal development.
During both pregnancies, erythropoiesis-stimulating agents and intravenous iron dosing was increased. The patient's hemoglobin was maintained at 10–12g/dl with the use of darbepoetin alpha once a week and IV iron sucrose dosage enough to maintain transferrin saturation of 30% or greater per unit protocol. Anti-hypertensive therapy was also changed in both cases with immediate suspension of angiotensin-converting enzyme-inhibitor and furosemide and the introduction of alpha-methyldopa (while maintaining carvedilol and long-acting nifedipine). The patient also received multivitamin, calcium carbonate, and folic acid throughout the pregnancies. Programmed adjustment of the dry weight was made by revising the estimated dry weight weekly to an expected weight gain during pregnancy progression, and she was allowed unlimited protein intake. Metabolic alkalosis was also prevented by closely following acid-base status and adjusting dialysate bicarbonate concentration accordingly.
The two main determinants of hemodialysis schedule are dialysis frequency and dialysis duration that significantly correlated with prematurity and delivery of a small for gestational age baby.1 The increase in dialysis time ensures a less uremic environment for the fetus, allows the mother a more liberal diet and fluid intake. It also helps to control hypertension and reduce the amplitude of blood volume and electrolyte shifts.2–6 Although no randomized prospective trials of pregnant women on dialysis exist, retrospective data suggest maintaining pre-dialysis BUN values at ≤50mg/dl is an appropriate goal.2,3,5,6
Careful attention needs to be paid to dialysis strategy, anemia control, fluid balance, control of hypertension, nutrition, and close monitoring of fetal well-being and maternal morbidities. Approaching pregnancy in a CKD patient in hemodialysis requires careful multidisciplinary management among nephrologists, obstetricians, nutritionists, nurses and dialysis staff.
Authors’ contributionsJoão Carvão, Pedro Vieira and Luís Resende provided medical care of the patient. João Carvão wrote the manuscript. Luís Resende and Pedro Vieira reviewed the literature. All authors edited the manuscript. João Carvão is the article guarantor
Statement of ethicsInformed consent was obtained for this report.
Funding sourcesNo subsidies or grants contributed to this work.
Conflicts of interestThe authors have no conflicts of interest to declare.