Duplex ultrasound (DUS) is increasingly used before vascular access (VA) surgery for haemodialysis. However, the cost-effectiveness of this approach is unknown. Our objective was to assess whether the introduction of a specialised consultation with DUS assessment modifies the cost and the time delay to achieve a first VA valid for haemodialysis.
Patients and methodsProspective cohort of patients undergoing a first VA (June 2014-July 2017) after a specialised consultation with DUS (ECO group). They were compared with a historical cohort (January 2012-May 2014) where VA was indicated exclusively by clinical evaluation (CLN group). We analysed the cost related to visits, DUS assessments, interventions, hospital admissions and graft materials to achieve a first VA valid for haemodialysis at least during 1 month.
Results86 patients in the CLN group were compared with 92 in the ECO group. Patients in the ECO group were younger (68.4 vs. 64.0 years; P=.038) but no other differences were seen among groups. The average cost to achieve a first AV valid for haemodialysis was significantly lower in the ECO group (2707 vs. 3347€; P=.024). There was a higher cost associated with DUS assessments in the ECO group yet the CLN group had a higher cost related to follow-up visits, successive surgical interventions, prosthetic material, days of hospital admission and catheters. The mean time needed to achieve a first AV valid for haemodialysis was also shorter in the ECO group (49.9 vs. 82.9 days, P=.002).
ConclusionThe introduction of a specialised vascular access consultation with DUS prior to VA surgery has reduced the cost necessary to achieve a first VA valid for haemodialysis. From the patient's point of view this has meant less interventions and hospital admissions and a shortening of the time delay.
La valoración mediante eco-doppler (ED) previa a la realización de un acceso vascular (AV) está cada vez más extendida, pero existen pocos estudios que aborden su coste/efectividad. Nuestro objetivo fue evaluar si la introducción de una consulta específica de AV con ED modifica el coste, los tiempos de demora, el número de re-intervenciones e ingresos para lograr un primer AV útil.
Pacientes y métodosCohorte prospectiva de pacientes sometidos a un primer AV (junio 2014-julio 2017), a quienes se practicó un ED preoperatorio (grupo ECO). Se compararon con una cohorte histórica (enero 2012-mayo 2014) de primeros AV indicados exclusivamente mediante valoración clínica (grupo CLN). Se calcularon los costes de realización y el seguimiento para lograr un AV útil para hemodiálisis durante como mínimo un mes sin complicaciones.
ResultadosSe compararon 86 pacientes del grupo CLN con 92 del ECO, siendo estos últimos más jóvenes (68,4 vs. 64,0 años; p = 0,038). El coste medio del grupo ECO fue significativamente inferior (ECO = 2.707 vs. CLN = 3.347 €; p = 0,024). El grupo ECO tuvo un coste mayor en ecografías preoperatorias y de seguimiento. El grupo CLN tuvo un coste superior respecto a consultas de seguimiento, intervenciones quirúrgicas sucesivas, material protésico, días de ingreso y catéteres. Se disminuyó el tiempo de demora para la realización del AV (CLN = 82,9 vs. ECO = 49,9 días; p = 0,002).
ConclusiónLa introducción de una consulta específica de AV para hemodiálisis con valoración ED, ha permitido disminuir el coste para lograr un primer AV útil, como consecuencia de una reducción en los tiempos de demora, visitas de control, re-intervenciones, días de ingreso e implantación de catéteres.
Key concepts
- •
Cohort study that compares the financial cost to achieve a functional vascular access (VA) for hemodialysis, in a group of patients assessed clinically (n = 86) and another group with ultrasound-doppler assessment (n = 92).
- •
The introduction of a specific consultation with echo-Doppler assessment reduced the cost of achieving a first useful VA by 21%.
- •
Delay periods, follow-up visits, reinterventions, days of admission and the need for catheter implantation were reduced.
At a technical level, there is controversy about the clinical usefulness of echo-doppler (ED) evaluation prior to performing a vascular access (VA) for hemodialysis (HD).1,2 However, the results of some meta-analyses3,4 have favored the preoperative use of this diagnostic method and the inclusion in the main clinical guidelines.5,6
The recommendation of the preoperative ED has conditioned changes in the clinical care of the patients and also the creation of a specific outpatient clinic for VA. These changes may be associated with an increase in cost. However, this increase in cost could be offset by direct clinical benefits, and improvement of certain organizational aspects, such as a decrease in waiting times or better long-term planning of VA.7
To date there are few studies that address the ratio cost/effectiveness resulting from the use echo-Doppler and the organizational changes to which it is often associated. We have described previously the clinical benefits of the introduction of preoperative DU in a prospective series of patients that needed a first VA for HD.8 The objective of this study was to assess whether the introduction of a specific VA consultation with ED modifies the financial cost, delay times and the number of re-interventions and admissions before achieving a first useful VA.
Patients and methodsThe intervention group was a prospective cohort of consecutive patients with stage 5 chronic kidney disease who underwent a first VA for HD between June 2014 and July 2017 in a single center (ECO group). The control group (CLN group) was the cohort of consecutive patients who underwent a first VA for HD between January 2012 and May 2014 in the same center was retrospectively analyzed.
The preoperative evaluation in the ECO group was performed in a specific VA clinic by single vascular surgeon (E.M.) that assessed the patient clinically and with the use of DU. The ultrasound was performed using a 7-11 MHz linear transducer and Logiq S7 Expert equipment (General Electric Healthcare, USA). In the CLN group, the preoperative evaluation was carried out exclusively clinically in a non-VA specific vascular surgery outpatient clinic. In both groups, the decision on the type of VA to be performed was made by vascular surgeons, in the CLN group only based on the clinical assessment and in the ECO group with additional information from the DU. All patients signed the informed consent for the interventions performed.
Surgical interventions and the first postoperative visit at 2 weeks were performed by vascular surgeons in both groups. Thereafter, patients were followed by the nephrology service every 3-4 months if patients were CKD stage 4 (GFR between 30-15) or every 1-2 months if patients were on stage 5 (GFR < 15. A HD nurse assessed the of development of the VA and possibilities of puncture. When lack of maturation or functional problems were detected, they were assessed again by the vascular surgery service. During follow-up, the data recorded was : a) functionality for HD, defined by successful puncture providing correct blood flows to the dalyzer (Qb > 300 ml/min in the first punctures); b) the number of clinical and ultrasound assessments required due to VA dysfunction; c) the number of re-interventions to maintain patency and usefulness of VA; d) the need for new VAs; and e) the mature VA through which HD was initiated.
The first useful VA was considered the one that allowed HD sessions without complications for a period of at least one month. In patients in whom the VA was not used, the death or change of RRT method (transplant or peritoneal dialysis) was considered the end of follow-up. The finance department of our center was asked to report the billing rates for the different healthcare acts involved in performing and monitoring the VA: a) the clinical and ultrasound assessment visits prior to the intervention; b) Actual surgery for creation of VA(including, if required, admission costs or prosthetic material); c) visits for clinical or ultrasound evaluation by vascular surgery during follow-up; d) additional surgical or endovascular interventions to maintain assisted patency and utility of the VA; e) surgical interventions for new VAs (including, if required, admission costs or prosthetic material); and e) the use of central venous catheters (CVC).
Statistical analysisQualitative variables were described as frequency and percentages, and quantitative variables by mean and standard deviation. The comparison of clinical characteristics and finantial cost between the two groups of patient was performed using the Chi-square test for qualitative variables and Student's t-test and Mann-Whitney U for quantitative variables. Statistical analysis was performed using the SPSS ® version 25 program. A p value of less than 0.05 was considered statistically significant.
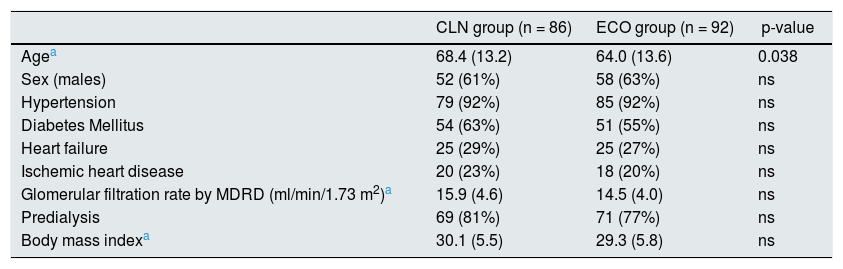
ResultsThe ECO group include 92 patients, while the CLN group had 86 patients. As shown in Table 1 at baseline there were no significant differences in the characteristics of both groups, except for age, which was lower in the ECO group. The mean follow-up was 1755.41 days in the CLN group (minimum 31/maximum 3007) and 1163.85 days in the ECO group (minimum 16/maximum 2106). The immediate and follow-up clinical results have been previously published.8
Baseline characteristics of patients undergoing a first surgical vascular access for hemodialysis, indicated after preoperative CLN or ECO.
| CLN group (n = 86) | ECO group (n = 92) | p-value | |
|---|---|---|---|
| Agea | 68.4 (13.2) | 64.0 (13.6) | 0.038 |
| Sex (males) | 52 (61%) | 58 (63%) | ns |
| Hypertension | 79 (92%) | 85 (92%) | ns |
| Diabetes Mellitus | 54 (63%) | 51 (55%) | ns |
| Heart failure | 25 (29%) | 25 (27%) | ns |
| Ischemic heart disease | 20 (23%) | 18 (20%) | ns |
| Glomerular filtration rate by MDRD (ml/min/1.73 m2)a | 15.9 (4.6) | 14.5 (4.0) | ns |
| Predialysis | 69 (81%) | 71 (77%) | ns |
| Body mass indexa | 30.1 (5.5) | 29.3 (5.8) | ns |
CLN: standard clinical assessment; ECHO: Doppler echo; MDRD: Modification of Diet in Renal Disease; ns: not significant.
The time elapsed between the request of VA by the nephrologist and the creation of the VA was 82.9 days (SD = 81.4) in the CLN group and 49.9 days (SD = 44.9 ) in the ECO group, this difference is statistically significant (p = 0.002).
A 70.9% of the patients in the CLN group and 80.4% of the patients in the ECO group were treated with HD. The cases that did not reach HD in the CLN and ECO group were due to death (17.4 and 10.9%, respectively), change of type of RRT (7.0 and 2.2%) or staying in pre-dialysis up to the end of follow-up (4.7/6.5%).
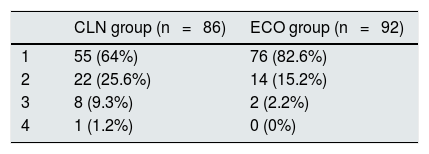
A new additional VA was required in cases due to thrombosis or because it could not be punctured, in 36% of the patients in the CLN group and 17.4% in the ECO group (p = 0.023); the number of interventions performed is shown in Table 2. The mean number of interventions to achieve a useful VA for HD for at least one month without complications was 1.47 in the CLN group and 1.19 in the ECO group (p < 0.001).
Number of interventions performed to achieve a VA useful for HD during at least one month without complications, indicated after CLN or after preoperative ECO.
| CLN group (n = 86) | ECO group (n = 92) | |
|---|---|---|
| 1 | 55 (64%) | 76 (82.6%) |
| 2 | 22 (25.6%) | 14 (15.2%) |
| 3 | 8 (9.3%) | 2 (2.2%) |
| 4 | 1 (1.2%) | 0 (0%) |
VA: vascular access; CLN: standard clinical evaluation; ECHO: Doppler echo; HD: hemodialysis.
The number of additional interventions performed to maintain the function of the initial or the successive VA before starting their HD puncture, were 14 in the CLN group (6 superficializations, 3 complete ligations, 2 ligation of collaterals, one pseudoaneurysm correction, one thrombectomy and one angioplasty) and 11 in the ECO group (5 angioplasties, 3 collateral ligations, one thrombectomy, one superficialization and one complete ligation).
Due to VA failure or lack of maturation, 7 patients (11.5%) in the CLN group and 2 (2.7%) in the ECO group required the placement of CVC implantation (p = 0.04). This is without taking into consideration those cases that had already started HD through a CVC prior to performing the VA.
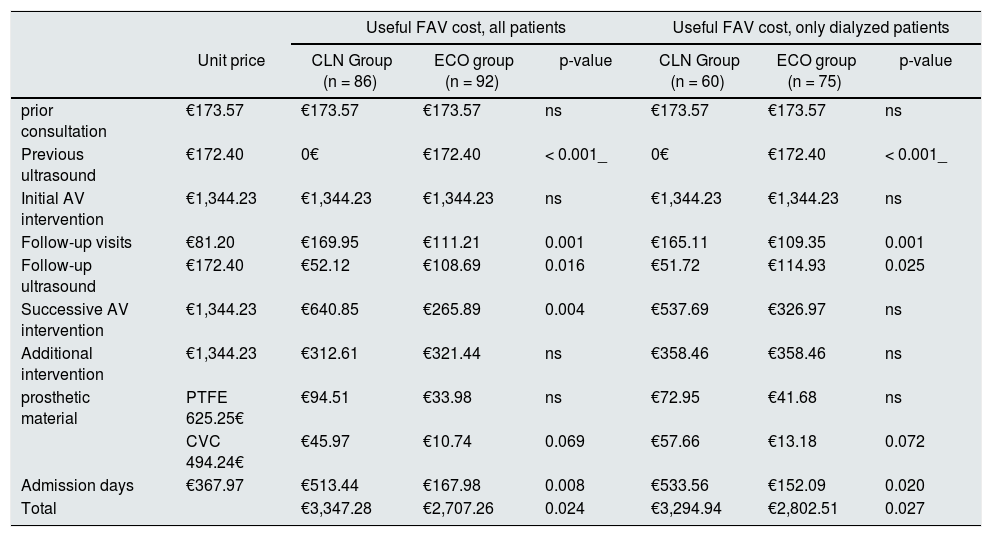
Based on the billing rates of the different types of care performed, a cost calculation was made until a useful VA was achieved able to be punctured for HD for at least one month without complications, or until the end of follow-up in those who did not receive dialysis. The mean costs of each act of care for each of the groups are shown in Table 3. The mean total cost in patients from the ECO group was significantly lower than in the CLN group (€2707 vs. €3347 ; p = 0.024). Although patients in the ECO group had a higher cost in preoperative or follow-up ultrasounds, the CLN group had a higher cost in terms of clinical visits, consultations, successive surgeries, prosthetic material, and days staying in the hospital. These differences were maintained even if only patients who started HD were analyzed.
Mean financial cost of the different care acts to achieve a useful VA for at least one month: a) in all patients, and b) only in patients who have used VA to perform hemodialysis.
| Useful FAV cost, all patients | Useful FAV cost, only dialyzed patients | ||||||
|---|---|---|---|---|---|---|---|
| Unit price | CLN Group (n = 86) | ECO group (n = 92) | p-value | CLN Group (n = 60) | ECO group (n = 75) | p-value | |
| prior consultation | €173.57 | €173.57 | €173.57 | ns | €173.57 | €173.57 | ns |
| Previous ultrasound | €172.40 | 0€ | €172.40 | < 0.001_ | 0€ | €172.40 | < 0.001_ |
| Initial AV intervention | €1,344.23 | €1,344.23 | €1,344.23 | ns | €1,344.23 | €1,344.23 | ns |
| Follow-up visits | €81.20 | €169.95 | €111.21 | 0.001 | €165.11 | €109.35 | 0.001 |
| Follow-up ultrasound | €172.40 | €52.12 | €108.69 | 0.016 | €51.72 | €114.93 | 0.025 |
| Successive AV intervention | €1,344.23 | €640.85 | €265.89 | 0.004 | €537.69 | €326.97 | ns |
| Additional intervention | €1,344.23 | €312.61 | €321.44 | ns | €358.46 | €358.46 | ns |
| prosthetic material | PTFE 625.25€ | €94.51 | €33.98 | ns | €72.95 | €41.68 | ns |
| CVC 494.24€ | €45.97 | €10.74 | 0.069 | €57.66 | €13.18 | 0.072 | |
| Admission days | €367.97 | €513.44 | €167.98 | 0.008 | €533.56 | €152.09 | 0.020 |
| Total | €3,347.28 | €2,707.26 | 0.024 | €3,294.94 | €2,802.51 | 0.027 | |
Indicated after CLN or after preoperative ECO in euros.
VA: vascular access; CLN: Standard clinical assessment; CVC: central venous catheter; ECO: Echo Doppler; AVF: arteriovenous fistula; ns: not significant; PTFE: vascular prosthesis: polytetrafluoroethylene tube.
As far as other factors associated with high cost. Obesity (BMI > 30) implied a higher cost in the overall patient population (p = 0.037) and in the CLN group (p = 0.042), but not within of the ECO group (p = 0.342). The rest of the factors did not show statistical significance.
DiscussionThe most notable result of the study is that the cost to achieve a useful VA was 21% lower in the ECO group compared to the CLN group. The fundamental aspects that influenced this decrease in cost were a lower number of follow-up visits and, above all, a less need to perform new successive VAs due to failure of the initial one. Consequently there were savings in hospital admission days and in the material required for arteriovenous prosthesis or tunneled CVC. This cost reduction has been greater than the extra cost of ultrasound assessments, both preoperatively and during follow-up.
To control the possible biases that could be caused by the intention-to-treat analysis of the total number of patients, with differences in the use of VA and in the period of follow-up, we performed a second analysis selecting those patients in whom VA had been used to initiate treatment with HD. The results obtained are very similar to those of the overall number of patients and would confirm a difference in costs regardless of the ultimate use of VA. It should be noted that the cost to achieve a useful VA in the CLN group was slightly lower in the subgroup of patients who underwent dialysis compared to those who did not, this is the inverse to the observed in the ECO group. A higher percentage of prosthetic VA that were never used would explain the extra cost in non-dialyzed patients in the CLN group.
The introduction of the DU probably made a difference not only in the evaluation prior to the placement of VA performance, but also during its follow-up, since the nephrologist uses the DU to assess lack of maturation of the AV and helps to detect lesions earlier when they are able to be corrected. Thus, endovascular interventions through angioplasty has increased, which in the CLN period was anecdotal; a greater VA survival was achieved at the expense of increasing costs in additional interventions. Despite this, this concept of cost has been very similar in both groups, as the need for other VA maintenance surgical procedures has been reduced.
In our study, in order to better adjust the real value, we decided to include the hospital bills of all care processes related to the creation and monitoring of the VA. In addition, we decided to value the expenses until reaching an objective: the usefulness of the VA to perform HD for a month without complications or until the end of follow-up in those who that were not punctured. We consider that performing the calculation throughout the entire follow-up could produce bias, since the 2 series evaluated were not coincident in time and therefore the period of the CLN group was higher. In addition, the complications presented by a VA that is being punctured regularly are not comparable to those that are not, so we decided to limit the evaluation to the beginning of its use to perform HD.
There is increasing evidence in favor of the use the DU as useful tool in the evaluation of the patient prior to placement a VA for HD,3,4 however the studies in the literature on the cost/effectiveness of this exploration are very scarce. The Austrian group of Györi et al.9 published a study in 2019 in which, in addition to an analysis of patency and complications of their series, they provided an analysis of costs, although including only the surgical interventions performed throughout the entire follow-up period. Like in our study, it is concluded that, given the greater number of reinterventions in the clinical evaluation group, the VA performed after ultrasound evaluation had a significantly lower cost (4074 vs. 6078 €; p < 0.001). The economic figures of this study are not comparable with the one carried out in our center, since the bill for surgical activity in both health systems is very different.
Another advantage besides the reduction in cost was the reduction in waiting periods by 40%, as a result of the modification of the referral protocols, as well as the improvement in the registration of patients who were awaiting intervention.. In the GEMAV5 clinical guide, delay periods of 3 months for normal priority referrals and 6 weeks for preferential referrals are indicators of quality of care. In our study, the average delay in the ECO group was 49 days, so it would be within the quality standards stablished, although we did not discriminate between VA of preferential priority and those that did not.
The patients included in our study were similar in number and characteristics in both groups, except for a higher mean age in the CLN group. Among the recognized risk factors 10,11, advanced age is one of those that may imply a worse prognosis of VA,12 so the difference found (68.4 vs. 64 years) could have some influence when it comes to to explain a worse result of the CLN group. But in the analysis of risk factors, age did not influence the cost, so we consider that this difference has not been of great relevance in the economic aspect.
Apart from the ultrasound assessment, obesity was a risk factor for a higher economic cost in the overall number of patients. But analyzing both groups separately, it was observed that the influence is diluted in the ECO group. The negative influence of obesity on the clinical results of VA for HD is widely recognized, as well as the usefulness of DU to assess the venous heritage in this subgroup of patients,13 thus avoiding unnecessary additional interventions.
There were no differences between both groups in the percentage of patients not previously controlled by nephrology and who had started HD urgently through CVC (19 vs. 22%) before being evaluated for VA assessment and performance. However, it was significant that the need to implant a CVC due to delayed maturation of an AVF was reduced in the ECO group as compared with the CLN group (11.5 vs. 2.7%). The decrease in surgical delay and the increase in the usefulness of AVFs have undoubtedly contributed to the improvement of this parameter. In Catalonia, the percentage of incident patients who started HD through a catheter during 2018 was 59.4%,14 which is much greater than the values observed in our series.
This study is not without the limitations that we want to highlight. First, the retrospective nature of the control series, which limits the validity of the information recorded. Second, the billing model of our center, in which there is a single cost per surgical act regardless of its complexity, therefore it does not allow discriminating the different value of the techniques. Thirdly, despite the assessments being made by a single explorer, ultrasound has a subjective component inherent to the technique itself, although this fact is shared by other studies with similar characteristics. Finally, the data collection belongs to a single hospital center with a limited number of patients and the results obtained may not be extrapolated to other populations, so they should be interpreted with caution.
In conclusion, the introduction of a specific VA clinic for HD patients, with evaluation by ED, has made it possible to reduce the cost of achieving a first useful VA, by reducing delay times, control visits, the number of re-interventions, days of admission and catheter implantation.
FinancingThis research has not received specific aid from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Mateos Torres E, Collado Nieto S, Arenas Jimenez MD, Lacambra Peñart M, Marcos Garcia L, Clará Velasco A. Impacto de la introducción de una consulta específica con valoración eco-doppler en el costo asociado a la obtención de un primer acceso vascular para hemodiálisis. Nefrologia. 2022;42:22–27.
This article has been performed within the framework of doctoral studies at the Autonomous University of Barcelona (UAB).