Karyomegalic interstitial nephritis (KIN) is an exceedingly rare disease characterized with enlarged tubular nucleus and presented with a slowly progressive renal failure, leading to end-stage renal disease (ESRD) usually before 50 years old.1 Zhou et al. identified recessive mutations of FAN1 gene as the cause of KIN.2 Approximately 70 patients with KIN have been reported worldwide till now, including nearly 20 families with an autosomal recessive inheritance proven to be associated with FAN1 pathogenic variant.2–5 There have been very few reports of renal transplantation and outcomes have generally been poor.5 In Chinese population, only two sporadic cases have been retrieved from the literature.6,7 Here we presented a novel compound heterozygote mutation in FAN1 gene in three Chinese familial cases of KIN with a long-term post-renal transplantation survival in one family member.
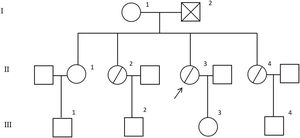
The parents of the proband (II-3) were nonconsanguineous and had four offsprings (II-1–II-4), three of which exhibited renal failure (shown in Fig. 1). We report the proband a 32-years old female was admitted to our nephrology department because of a two-year deranged renal function without hypertension or diabetes. During the past two years, she had a serum creatinine concentration fluctuated between 100 and 120μmol/L (normal range: 30–110μmol/L). On presentation, serum creatinine level was 121μmol/L, the estimated glomerular filtration rate (eGFR) was 42mL/min/1.73m2. The urinalysis was bland with absent proteinuria and hematuria, except for an obviously low urine specific gravity (SG) of 1.010. Her liver function was also deranged, with an alanine aminotransferase (ALT) of 62IU/L (normal range: 0–40IU/L), an aspartate aminotransaminase (AST) of 46IU/L (normal range: 0–40IU/L). Serology evaluation for hepatitis and human immunodeficiency virus was negative. Ultrasound showed bilateral atrophic kidneys with increased echogenicity. The left kidney measured 8.5cm in length and the right measured 9.2cm in length.
Patient II-2, born in 1963, received renal transplantation in 2014 because of renal failure. She had a history of exposure to decoration materials for a long time and a history of recurrent upper respiratory tract infections before renal transplantation. The renal function was relatively stable during the approximately 8-year follow-up period after transplantation. Recent serum creatinine level was 150μmol/L, with an eGFR of 33mL/min/1.73m2. Urinalysis showed a lower SG at 1.005, proteinuria, hematuria and glucouria was negative.
Patient II-4, born in 1971, a declined eGFR at 60mL/min/1.73m2 with serum creatinine level at 94μmol/L was detected in a physical examination in 2012, the urinalysis at that time was bland with absent proteinuria and hematuria, except for a relatively lower urine specific gravity of 1.015. During the approximately 10-year follow-up period, her serum creatinine concentration fluctuated between 90 and 130μmol/L with normal liver function. Recent ultrasound showed bilateral atrophic kidneys with increased echogenicity, both of the kidneys measured 8.4cm in length.
Since the kidneys were small to safely undergo biopsy, and there was a strong history of renal impairment in her family, whole exome sequencing (WES) was performed for proband II-3, which revealed a novel compound heterozygote mutation in the gene FAN1 NM_014967.4 (c.1943+1G>A(p.?)) and (ex.2-5del(p.?)) and confirmed by Sanger sequencing. A study of all family members using Sanger sequencing revealed that patient II-2 and II-4 carried the same compound heterozygote mutation. The unaffected sibling, their mother, and their children carried a single heterozygous allele. FAN1 NM_014967.4 (c.1943+1G>A(p.?)) mutation was found in their mother (shown in Fig. 2), FAN1 NM_014967.4 (ex.2-5del(p.?)) mutation was found in III-2 and III-3. Though karyomegaly of the renal epithelial cells could not be confirmed due to lack of a renal biopsy, given the presence of a compound heterozygote mutation, a family history of renal failure, a diagnosis of KIN was made.
FAN1 gene predominantly expressed in the kidney and is specifically engaged in the repair of a possible renal-specific DNA damage.2FAN1 mutations might render tubular cells more susceptible to environmental genotoxin-induced renal DNA damage, such as acute or chronic exposure to environmental toxins or radiations, and various exposure may explain a part of the CKD progression heterogeneity.8 Patient II-2 in our cases had a history of long-term exposure of heavy metal, and showed the most rapid renal progression, which supported the suggestion that environmental toxins interfered with KIN progression.
One patient of our cases received renal transplantation, and followed up for 8 years with relatively stable renal function. The long-term oncologic and infectious risk in patients with KIN who undergo renal transplantation was suggested to be correlated with immunosuppressive agents.9 Familial living donation in this context has to be evaluated carefully and by genetic testing, heterozygous carriers might be at increased risk of CKD and a donation in heterozygous carriers should be discouraged. Mutations in FAN1 gene should be suspected in individuals with interstitial nephropathy, especially with a family history of renal disease.
Statement of ethicsThis study protocol was reviewed and approved by the Ethics Committee of Shandong Provincial Hospital affiliated to Shandong First Medical University. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Author contributionsHuizi Zhu contributed to sample collection, analyzed clinical data, performed Sanger sequencing and segregation analysis, and drafted the paper; Yucai Liu and Xiumin Ding contributed to the collection of clinical data and drafted the paper; Xiang Liu, Liang Xu and Bing Zhao contributed to genetic counselling and sample collection; Xiaowei Yang and Rong Wang designed and initiated the study, monitored data collection and analysis for the study and revised the paper. All authors read and approved the final manuscript.
FundingThis work was supported by grants of Taishan Scholars Program of Shandong Province (No. ts201712090), Academic Promotion Program of Shandong First Medical University (No. 2019QL022), and China International Medical Foundation (No. Z-2017-24-2037).
Conflict of interestsNone.
We are grateful to the families who contributed to this study.