Vitamin D deficiency and polypharmacy is a common problem over chronic kidney disease (CKD) population.
ObjectivesTo assess the clinical and analytical characteristics of CKD patients with 25-OH-D3 deficiency (<15 ng/mL), including the possible role of associated drugs.
MethodsA single center observational review of 137 incident patients referred to our outpatient clinic with different stages of CKD and 25-OH-D3<15ng/mL (male gender 53.3%, mean age 70.8 [±16.1] years, mean GFR (MDRD-4) 43.6 [±25.5] ml/min/1.73 m2). 25-OH-D3 levels were collected in spring. Clinical and biochemical data and associated medications were recorded.
ResultsMean 25-OH-D3 levels were 8.23 [±4.03] ng/ml. Eighty-eight patients (64.7%) had 3 or more concomitant drugs. Only 7 patients (5.1%) were not receiving any medication. Patients were divided in three groups according the therapies into none (n=26), RAS inhibitors or allopurinol (n=81), and RAS inhibitors plus allopurinol (n=30); with the aim to study the influence of statin therapy. Patients under renin angiotensin (RAS) inhibitors or Allopurinol treatment presented significantly higher 25-OH-D3 levels (p=0.001 and p=0.01 respectively), however patients with Statins treatment had lower 25-OH-D3 level (p=0.039). Personal history of diabetes, cardiovascular events or other therapies did not modify 25-OH-D3 levels, adjusted by age and eGFR.
ConclusionsCKD patients with vitamin D deficiency who received RAS inhibitors or Allopurinol treatment had higher 25-OH-D3 levels, however those with statins treatment had lower vitamin D levels. Randomized controlled trials are required to confirm these findings.
La deficiencia de vitamina D y la polifarmacia constituyen un problema común en la población con enfermedad renal crónica (ERC).
ObjetivosEvaluar las características clínicas y analíticas de los pacientes de ERC con deficiencia de 25-OH-D3 (<15 ng/mL), incluyendo la función posible de los fármacos asociados.
MétodosSe realizó una revisión observacional en un único centro, de 137 pacientes incidentes remitidos a nuestra clínica ambulatoria con diferentes estadios de ERC y 25-OH-D3<15 ng/mL (varones 53,3%, edad media 70,8 [±16,1] año, GFR medio (MDRD-4) 43,6 [±25,5] ml/min/1,73 m2). Los valores de 25-OH-D3 se recolectaron en primavera. Se registraron los datos bioquímicos y los fármacos asociados.
ResultadosLos niveles medios de 25-OH-D3 fueron de 8,23 [±4,03] ng/ml. Ochenta y ocho pacientes (64,7%) tomaban tres o más fármacos concomitantes. Únicamente siete pacientes (5,1%) no recibían medicación alguna. Los pacientes fueron divididos en tres grupos, conforme a las terapias: ninguna (n = 26), inhibidores RAS o Alopurinol (n = 81), e inhibidores RAS más alopurinol (n = 30), a fin de estudiar la influencia de la terapia de estatinas. Los pacientes sometidos a tratamiento de inhibidores de la renina-angiotensina (RAS) o Alopurinol presentaron unos niveles considerablemente superiores de 25-OH-D3 (p = 0,001 y p = 0,01 respectivamente), y sin embargo los pacientes con tratamiento de estatinas presentaron unos menores niveles de 25-OH-D3 (p = 0,039). La presencia de diabetes, episodios cardiovasculares u otras terapias no modificaron los niveles de 25-OH-D3, ajustados por edad y eGFR.
ConclusionesLos pacientes de ERC con deficiencia de vitamina D, sometidos a tratamiento de inhibidores RAS o Alopurinol reflejaron unos niveles superiores de 25-OH-D3, y sin embargo aquellos sometidos a tratamiento de estatinas reflejaron unos menores niveles de vitamina D. Se precisan ensayos aleatorizados controlados para confirmar estos hallazgos.
Over last decade, interest in vitamin D physiopathology has increased greatly due to the discovery of additional biological actions of vitamin D out off its traditional role in bone and mineral metabolism. These additional biological effects are: suppression of renin-angiotensin system1 (RAS), protection against cardiovascular event,2 decrease in inflammatory markers,3,4 reduction of megalin and cubilin shedding,5 improved systolic blood pressure in patients with type 2 diabetes,6 and increases nephrin expression in podocytes in experimental data.7
On the other hand, vitamin D deficiency is an emerging global health problem that is estimated to affect more than 1 billion people worldwide.8 It is very common in patients with chronic kidney disease (CKD), even at early stages,9 and the severity of deficiency increases with the progression of kidney disease.
Vitamin D deficiency is partly caused by vitamin dysregulated D metabolism in kidney disease, because the final activation step of synthesis of Vitamin D, 1-hydroxylation, occurs primarily, but not exclusively, in the kidney.
CKD patients used to have a high comorbidity, so are treated with a huge amount of drugs.10,11 Therefore medication-related problems are very common in CKD patients. The possible collateral effect of these medications on vitamin D synthesis and metabolism had been previously described,12,13 but remains unclear.
We conducted an observational study to assess the characteristics of 25-OH-D3 deficient CKD patients, including the possible role of different associated therapies, as statins, renin angiotensin system (RAS) inhibitors or Allopurinol.
MethodsParticipantsA transversal single-center study was conducted including a sample of 137 incident patients referred to our CKD outpatient clinic. Patients undergoing renal replacement therapy, kidney transplant recipients, and with recent hospital admission in last 3 months or with acute diseases, were excluded. We also excluded patients supplemented with any kind of vitamin D or analog in the last 3 months. Medical records were consulted to obtain demographic, anthropometric data and previous cardiovascular events. Treatment was also recorded: kind and number of antihypertensive drugs, statin and allopurinol therapy. Analytical values were collected at the same time including creatinine, calcium, phosphate, parathormone (PTH), serum uric acid, ultrasensible C-reactive protein (CRP), proteinuria and urine albumin/creatinine ratio. To avoid seasonal changes, serum 25-OH-D3 levels were determined in all patients between February and May.
Patients were divided in three groups according RAS inhibitors or allopurinol concomitant therapies into none (n=26), RAS inhibitors or allopurinol (n=81), and RAS inhibitors plus allopurinol (n=30); with the aim to study the influence of statin therapy in these groups.
Laboratory measurements were made using standardized automated methods. Daily urinary albumin excretion was measured with an immunonephelometric method. Serum 25-OH-D3 levels and intact PTH were measured using standarized automated methods of chemiluminescence immunoassay (Liaison® and Immulite 2000®, respectively).
Estimated glomerular filtration rate (eGFR) was calculated using the MDRD-4 formula.14 Vitamin D deficiency was defined according with KDOQI 2008 guidelines as 25-OH-D3 levels less than 15 ng/mL.15
Statistical analysisNormally distributed values are expressed as mean ±SD (standard deviation); non-normally distributed values are expressed as median ±IQR (interquartile range). The differences in quantitative variables were examined using the chi-square test for categorical variables and t test for continuous variables. Analysis of variance was used to study the differences on 25-OH-D3 levels between the groups according concomitant therapies. A linear model was accomplished to identify the relationship between different variables. Multivariate analysis (linear multivariate regression) was performed to determine the independent risk factors for 25-OH-D3 deficiency including all the factors with p<0.1 in the univariate model and potential confounding factors (as concomitant therapies, age, gender, diabetes mellitus, eGFR, and prior history of congestive cardiac failure). All statistical analyses were conducted using SPSS for Windows, V 11 (SPSS®, Chicago, Illinois, USA). Statistical significance was set at P<0.05.
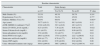
ResultsDemographic data, clinical and baseline biochemical characteristics are shown in Table 1. Mean serum 25-OH-D3 levels were 8.23±4.03 ng/ml. According with KDOQUI guidelines16 86 patients (62.7%) had CKD stage 3, 10.2% stages 1 and 2, and 27% presented eGFR<30ml/min/1.73 m2. Although male gender presented higher 25-OH-D3 levels (8.35 [±3.40] versus 7.52 [±3.06] ng/dl) these differences are not significant. Sixty-one patients (33.2%) had a previous cardiovascular event (CVE). The most frequent was myocardial infarction with 14.7%. Previous congestive cardiac failure (CCF) had been found in 18 patients (9.8%).
– Baseline characteristic of the patients.
| Baseline characteristic | ||||
|---|---|---|---|---|
| Characteristic | Total | Statin therapy | ||
| n=137 | Yes N=74 | No n=63 | P value | |
| Male Gender (%) | 53.3% | 49.3% | 50.7% | 0.24* |
| Hypertension (Yes) (%) | 91.9% | 54.4% | 45.6% | 0.77* |
| Diabetes Mellitus (Yes) (%) | 40.9% | 69.6% | 30.45 | 0.003* |
| Age (years) | 70.77 (±16.1) | 72.7 (±13.1) | 68.5 (±19.9) | 0.12 |
| eGFR (MDRD-4) (ml/min/1.73m2) | 43.62 (±26.22) | 39.5 (±18.9) | 48.5 (±32.3) | 0.53 |
| Serum 25-OH-D3 levels (ng/mL) | 8.23 (±4.03) | 7.38 (±2.9) | 8.66 (±3.6) | 0.022 |
| Serum Calcium levels (mg/dL) | 9.1 (±0.53) | 9.14 (±0.52) | 9.09 (±0.52) | 0.62 |
| Serum phosphate levels (mg/dL) | 3.54 (±0.68) | 3.6 (±0.71) | 3.5 (±0.65) | 0.64 |
| Serum PTH levels (ng/L) | 200.5 (±230.8) | 175.8 (±129.4) | 222.7 (±290.9) | 0.22 |
| Serum uric acid levels (mg/dL) | 6.84 (±1.77) | 6.76 (±1.77) | 6.92 (±1.76) | 0.59 |
| Serum CRP (mg/L) | 0.61 (±0.92) | 0.59 (±0.92) | 0.62 (±0.94) | 0.86 |
| Urine Albumin/Creatinine ratio (mg/g) | 564.0 (±994.6) | 586.7 (±898.2) | 542.0 (±1097.4) | 0.85 |
eGFR, estimated glomerular filtration rate; CRP, C-reactive protein, PTH, parathyroid hormone.
P-value obtained by T-student test, except * obtained by Mann-Whitney test.
Eighty-eight patients (64.7%) were receiving 3 or more concomitant drugs. Only 7 patients (5.1%) were not receiving any treatment. Bone and mineral metabolism parameters and eGFR of the patients according concomitant medications are shown in Table 2. Patients under RAS inhibitors and allopurinol treatment were associated with higher 25-OH-D3 levels. However, statin treatment, diabetes mellitus and history of CCF was associated with lower levels of 25-OH-D3 levels. Allopurinol-taking patients presented higher serum phosphate and PTH levels as well as and lower eGFR. Patients treated with insulin, erythropoiesis-stimulating agents (ESA) and with history of CVE presented lower eGFR. There are no differences between calcium levels according concomitant drugs. Multivariate analysis adjusted by age, gender, eGFR, serum calcium and PTH levels, personal history of diabetes, CVE or CCF showed that RAS inhibitors (beta 1.73, p=0.013), allopurinol treatment (beta 1.63, p= 0.011) and statins treatment (beta –1.35 and p=0.029) were independent predictors for lower serum 25-OH-D3 levels (Table 3).
– Analytical characteristic of the patients according with the therapies.
| n | 25-OH-D3 (ng/L) | p | Phosphate (ng/L) | p | Calcium (mg/dL) | p | PTH (mg/dL) | p | eGFR MDRD-4 (ml/ | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| min/1.73m2) | |||||||||||
| Therapy | |||||||||||
| RAS inhibitors | 113/ | 8.61 [3.95]/ | .001 | 3.57 [.71]/ | .33 | 9.14 [.54]/ | .32 | 147 [108-222]/ | .75* | 41.7 [24.1]/ | .138 |
| (yes/no) | 34 | 6.70 [2.50] | 3.44 [.59] | 9.04 [.48] | 213 [117-304] | 49.5 [31.5] | |||||
| Allopurinol | 38/ | 9.78 [4.67]/ | .01 | 3.74 [.73]/ | .03 | 9.20 [.47]/ | .22 | 189 [126-307]/ | .004* | 35.0 [11.1]/ | .001 |
| (yes/no) | 99 | 7.62 [3.19] | 3.46 [.65] | 9.09 [.55] | 147 [100-215] | 46.9 [29.4] | |||||
| Statins | 74/ | 7.55 [3.31]/ | .039 | 3.57 [.07]/ | .64 | 9.14 [.52]/ | .62 | 166 [121-253]/ | .12* | 39.5 [18.9]/ | .056 |
| (yes/no) | 63 | 8.83 [4.08] | 3.51 [.65] | 9.10[.54] | 144 [98,219] | 48.5 [32.3] | |||||
| Omega-3 | 5/ | 6.2 [5,11.5]/ | .97* | 3.41 [2.51-4.05]/ | .58* | 9.2 [8.75-9.6]/ | .65* | 135 [77-189]/ | .43* | 43.1 [35.8-86]/ | .19* |
| (yes/no) | 131 | 7.6 [4.9, 10.4] | 3.46 [3.03-4.02] | 9.2 [8.8-9.4] | 150 [109-241] | 36.8 [35.7-48] | |||||
| OAD | 24/ | 6.5 [4,11.1]/ | .108 | 3.62 [.68]/ | .46 | 9.15 [.53]/ | .75 | 156 [98-245]/ | .85* | 43.5 [24.5]/ | .98 |
| (yes/no) | 113 | 7.55 [4.9, 10.4] | 3.54 [.68] | 9.11 [.53] | 150 [110-239] | 43.7 [26.7] | |||||
| Insulin | 23/ | 7.21 [3.04]/ | .18 | 3.57 [.70]/ | 0.82 | 9.17 [.43]/ | .61 | 183 [113-242]/ | .47* | 36.2 [10.1]/ | .009 |
| (yes/no) | 114 | 8.44 [4.18] | 3.50 [.68] | 9.11 [.55] | 150 [107-238] | 45.2 [28.2] | |||||
| OAD + Insulin | 7/ | 6.5 [4,11.1]/ | .58* | 3.52 [3-4.2]/ | .89* | 9.3 [9-9.6]/ | .34* | 126 [121-150]/ | .52* | 37.1 [29.3-48.2]/ | .66* |
| (yes/no) | 130 | 7.55 [4.9, 10.4] | 3.43 [3-4] | 9.2 [8.8-9.4] | 153 [107-242] | 38.5 [25.7-39.4] | |||||
| Aspirin | 29/ | 8.51 [3.53]/ | .49 | 3.42 [.72]/ | .28 | 9.14 [.43]/ | .76 | 189 [135-260]/ | .72* | 37.9 [11.1]/ | .038 |
| (yes/no) | 103 | 7.98 [3.74] | 3.57 [.67] | 9.11 [.55] | 146 [101-221] | 45.2 [28.8] | |||||
| ESA | 11/ | 6.42 [2.67]/ | .17* | 3.91 [3.24-4.41]/ | .09* | 9.12 [8.71-9.53]/ | .55* | 150 [105-336]/ | .28* | 25.1 [21.6-33.6]/ | .001* |
| (yes/no) | 125 | 8.28 [3.74] | 3.42 [3.0-4.0] | 9.22 [8.86-9.43] | 229 [111-225] | 38.6 [30.1-49.1] | |||||
| Past medical history | |||||||||||
| Gender | 73/ | 8.35 [3.40]/ | .13 | 3.44 [0.69]/ | .03 | 9.0 [0.52]/ | .14 | 146 [96-226]/ | .10* | 47.0 [29.2]/ | .11 |
| (male/female) | 64 | 7.52 [3.06] | 3.71 [0.65] | 9.2 [052] | 165 [119-260] | 39.8 [21.8] | |||||
| Diabetes | 81/ | 7.14 [2.95]/ | .005 | 3.52 [0.68]/ | .68 | 9.1 [0.56]/ | .24 | 154 [121-220]/ | .69 | 39.5 [18.3]/ | .09 |
| (yes/no) | 56 | 8.88 [4.06] | 3.65 [0.69] | 9.2 [0.47] | 148 [101-244] | 46.5 [30.3] | |||||
| History of CCF | 19/ | 6 [4.5-8.25]/ | .004* | 3.54 [0.65]/ | .96* | 9.13 [0.53]/ | .87* | 221 [128-277]/ | .09* | 39.4 [28.8-45.7]/ | .92* |
| (yes/no) | 129 | 7.7 [4.98-10.5] | 3.53 [0.69] | 9.11 [0.53] | 148 [104-222] | 36.7 [28.7-48.8] | |||||
| History of CVE | 60/ | 7.45 [4.93-9.93]/ | .5* | 3.47 [0.66]/ | .34 | 9.08 [0.50]/ | .47 | 187 [134-279]/ | .001* | 36.6 [11.3]/ | .002 |
| (yes/no) | 77 | 7.7 [4.8-10.55] | 3.59 [0.7] | 9.16 [0.56] | 132 [91-213] | 49.1 [32.6] | |||||
| Proteinuria | 34/ | 7.16 [3.24]/ | 0.075 | 3.60 [0.75]/ | .49 | 8.97 [0.54]/ | .52 | 146 [101-189]/ | .38* | 41.0 [21.4]/ | .38 |
| (yes/no) | 100 | 8.3 [3.28] | 3.51 [0.67] | 9.18 [0.52] | 154 [114-253] | 445 [127.8] |
n, number of patients; eGFR, estimated glomerular filtration rate; RAS inhibitors, inhibitors of renin-angiotensin-aldosterone system; CCF, congestive cardiac failure; OAD, oral antidiabetic drugs; ESA, erythropoiesis-stimulating agents. Proteinuria yes if Urine Albumin Creatinine ratio >300 mg/g.
P-value obtained by T-student test, except * obtained by Mann-Whitney test.
– Linear Multivariate Regression (adjusted by age, eGFR and prior history of Congestive cardiac failure).
| P value | Beta | |
|---|---|---|
| Allopurinol treatment | p=0.011 | 1.63 |
| RAS inhibitors | p=0.013 | 1.73 |
| Statin Treatment | p=0.029 | –1.35 |
| Diabetes Mellitus | p=0.06 | –1.18 |
RAS inhibitors, inhibitors of renin-angiotensin-aldosterone system.
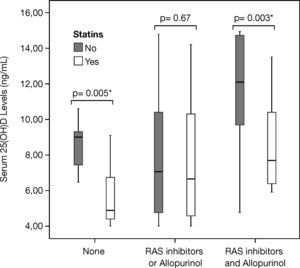
Patients who were not receiving RAS inhibitors or allopurinol presented lower 25-OH-D3 levels than those receiving RAS inhibitors or allopurinol, and RAS inhibitors plus allopurinol (p<0.001) (Fig. 1). Highest 25-OH-D3 levels (11.7±3.11 ng/mL) of our cohort were found in patients receiving RAS inhibitors plus allopurinol without statins. Lowest 25-OH-D3 levels of our cohort (5.7±1.82 ng/mL) were found in patients who receiving statins alone. In the group without RAS inhibitors or Allopurinol patients under statins therapy presented lower serum vitamin D levels (5.7±1.82 ng/mL vs. 7.8±3.4 ng/mL, p=0.05) compared with patient under RAS inhibitors or Allopurinol alone. Similarly, in the group with RAS inhibitors plus Allopurinol patients under statins therapy presented lower serum vitamin D levels (11.7±3.5 ng/mL vs. 8.5±2.5 ng/mL, p=0.003) than those with RAS inhibitors plus Allopurinol alone. There were also statistical differences when we compared patients under statin treatment with and without RAS or allopurinol therapy (5.7±1.82 ng/mL vs. 7.5±3.2 ng/mL, respectively p=0.015) and comparing patients under statin treatment with RAS or allopurinol therapy with patients under RAS plus allopurinol therapy (5.7±1.82 ng/mL vs. 8.5±2.3 ng/mL, p=0.02 respectively). Similarly, there were statistical differences comparing patients without statin treatment with RAS inhibitors or Allopurinol treatment vs. RAS inhibitors plus Allopurinol (7.8±3.4 ng/mL vs. 11.7±3.5 ng/mL, p=0.002).
– Relationship between therapies and baseline serum 25-OH-D3 levels. Patients were divided in three groups according with the concomitant therapies, and there were significant statistical differences between groups (p<0.001). Patients who were not receiving renin angiotensin system (RAS) inhibitors or allopurinol (n=26) presented lower 25-OH-D3 D levels than those receiving RAS inhibitors or allopurinol (n=81), and RAS inhibitors plus allopurinol (n=30) (p<0.001). Highest 25-OH-D3 levels (11.7±3.11, p=0.003) were found in patients receiving RAS inhibitors plus allopurinol without statins. Lowest 25-OH-D3 levels (5.7±1.82, p=0.005) were found in patients who only receiving statins.
Additionally, we collected 25-OH-D3 levels in 23 CKD patients before (17.8 [11.9-26.45]) and 3 months after (22.0 [13.65-27.45]) RAS inhibitors introduction (p<0.001), and in 15 patients before (43.3 [14.0-76.8]) and 3 months after (25.7 [23.2-43.3]) Allopurinol introduction (p=0.66).
DiscussionOur data suggest that concomitant treatment with allopurinol and RAS inhibitors is associated with high levels of 25-OH-D3 in CKD vitamin D deficient population. On the other hand, treatment with statins is associated with lower levels.
CKD patients used to have a high comorbidity and therefore are treated with a huge amount of drugs. The possible collateral effect of these medications on vitamin D synthesis and metabolism had been previously described in some reports, but remains unclear.
Although the interaction between Vitamin D and RAS is well known there are not previous reports about the effect of RAS inhibition on vitamin D levels. Vitamin D is a down regulator of the RAS by supressing renin expression,1,17 and its deficiency can activate the local RAS in the kidney.18 The renoprotective and antiatherogenic efficacy of the combination therapies of RAS inhibitors and vitamin D analogue has been reported in animal models.19-21 To provide biological plausibility to our finding, we have 2 different arguments. Firstly, RAS inhibitors by decreasing glomerular proteinuria, decrease the competition between proteins and vitamin D for receptor-binding site to be reabsorbed by megalin-cubilin complex in the proximal tubule.22 That means that RAS inhibitors increase the free receptor-binding sites for vitamin D reabsorption. And secondly, RAS inhibitors have a potent antiinflammatory effect23,24 and the inflammatory status has been associated in many studies with vitamin D levels.3-5
Patients treated with Allopurinol had higher 25-OH-D3 levels. We did not find any association with serum uric acid levels. Takahashi et al. described a lower serum 1-25 (OH) D3 levels in gout patients compared with control subjects, and a significant increase in serum 1-25 (OH) D3 after 1 year of administration of uric acid lowering agent. In animal models had been found that uric acid and xanthine suppresses 1alpha-hydroxylase activity and synthesis of 1-25 (OH) D3 and also suppresses its clearance rate.25 Moreover in the Vanholder et al. small cohort of CKD patients had been reported an increase in 1-25 (OH) D3 after allopurinol treatment,26 which they mainly attributed to a decrease in clearance rate of 1-25 (OH) D3. On the other hand, the anti-inflammatory power of Allopurinol was found also in moderate CKD.27 In our opinion, the increase in 25-OH-D3 on allopurinol treated patients observed is due to decrease in anti-inflammatory markers and suppression on 25-OH-D3 clearance rate.
Vitamin D is mainly produced by the endogenous pathway. Seven-dehydrocholesterol is converted to vitamin D3 in the skin in response to ultraviolet B light exposure.28 Statins reduce both cholesterol and 7-DHC production, and would be expected to reduce both cholesterol and vitamin D production. Furthermore, 25-OH-D3 before to be hydroxilated in the kidney, need to be reabsorbed in the proximal tubules by megalin/cubilin/amnioless complex. Megalin belongs to LDL receptor family.29 This complex must be prenylated to be active. Statins, by inhibiting HMG-CoA reductase, reduce the amount of mevalonate, a key intermediate in these preynilation. Deficiency or dysfunction of the megalin– cubilin complex decreases vitamin D concentrations.30 However the effect of statins in vitamin D metabolism is unclear and some studies suggested that statins may increase10 or not affect30 vitamin D levels, maybe depending on their anti-inflammatory power.
We did not find any association between some of the traditional risk factors for 25-OH-D3 deficiency, as age, female gender, diabetes mellitus5 or proteinuria.4 Possibly because we selected a very specific cohort, CKD patients with severe deficiency of 25-OH-D3, what means a proteinuric elderly male dominant cohort (564.0 [±994.6] mg/g, 70.77 [±16.1] years and 53.3 respectively) with 40.4% of diabetics.
Although we found an increase in 25-OH-D3 levels after 3 months of SRAA therapy in a small subanalysis group (n=23) reassuring our previous findings, we understand that the small sample size just allow us to highlight the possible association.
There are several limitations to our study. Firstly, the small number of patients. Secondly, 25-OH-D3 levels could be undervalued because we only made a single determination in spring (February and May). Thirdly, we did not consider for how long the patients have been with the recorded therapy, the reason, the dose or the achievement of the therapeutic gold. Finally this is just a transversal study, therefore we only can point the associations that we found, but not the causality.
In conclusion, 25-OH-D3 deficiency and polypharmacy are a common problem over CKD patients. Patients under RAS inhibitors or Allopurinol treatment had higher 25(OH) D levels, however patients with statins treatment had lower vitamin D level. Finally, randomized controlled trials are required to confirm these findings.
Financial supportNone.
Conflict of interestsThe authors declare that they have no conflict of interests.