Tacrolimus is the cornerstone of immunosuppressive therapy in kidney transplantation, but its pharmacokinetic variability and narrow therapeutic window present challenges for optimal dosing and long-term graft survival.1 Extended-release formulations, such as LCPT (Envarsus®) and ER-Tac (Advagraf®), have been developed to improve adherence and bioavailability.2,3 However, direct comparative studies using paired kidneys from the same donor are scarce. Here, we present a prospective, paired, open-label study comparing the efficacy and safety of LCPT and ER-Tac in de novo kidney transplant recipients.
MethodsWe included 108 adult recipients of deceased donor kidney transplantation (DDKT) at a single center (Málaga, Spain). Each donor provided kidneys to two recipients, one assigned to LCPT and the other to ER-Tac, minimizing donor-related confounding. All patients received standard triple immunosuppression (tacrolimus, mycophenolic acid, steroids). Clinical and laboratory data were collected at baseline and regular intervals up to 48 weeks. Renal function, acute rejection (clinical and subclinical), pharmacokinetics, and safety (including infection and post-transplant diabetes) were assessed. Protocol biopsies were performed at three months in a subset of patients.
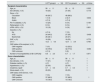
ResultsBaseline characteristicsBoth groups were well matched for recipient and donor demographics (Table 1).
Basal donors and recipients’ characteristics.
| LCPT group(n=54) | ER-Tac group(n=54) | p-Value | |
|---|---|---|---|
| Recipient characteristics | |||
| Age, ys. | 58±11 | 55±12 | 0.325 |
| Sex (female), n (%) | 18 (33) | 27 (50) | 0.118 |
| Race, n (%) | |||
| Caucasian | 49 (90.7) | 48 (88.9) | 0.842 |
| Black | 1 (1.9) | 2 (3.7) | |
| Arabic | 4 (7.4) | 4 (7.4) | |
| Pre-Tx diabetes, n (%) | 13 (24) | 8 (14) | 0.184 |
| Retransplant, n (%) | 8 (14) | 8 (14) | 1 |
| cPRA >50%, n (%) | 10 (18) | 9 (16) | 0.801 |
| Induction, n (%) | |||
| No | 4 (7.4) | 7 (13) | 0.409 |
| ATG | 24 (44.5) | 27 (50) | |
| Basiliximab | 26 (48.1) | 20 (37) | |
| DGF, n (%) | 16 (29) | 18 (33) | 0.775 |
| CIT, h | 13.2±4.0 | 12.9±3.9 | 0.760 |
| CMV status of the recipient, n (%) | |||
| CMV-negative | 7 (13) | 12 (22.2) | 0.062 |
| CMV-positive | 43 (79.6) | 42 (77.8) | |
| CMV-unknown | 4 (7.4) | 0 (0) | |
| Number of incompatibilities (A-B-C-DR-DQ) | 6.8±2.0 | 6.7±1.7 | 0.971 |
| Donor characteristics | |||
| Age, ys. | 58±11 | 58±11 | 1 |
| Sex (female), n (%) | 17 (31) | 17 (31) | 1 |
| Diabetes mellitus, n (%) | 4 (7) | 4 (7) | 1 |
| Hypertension, n (%) | 22 (40) | 22 (40) | 1 |
| Creatinine, mg/dl | 0.7±0.3 | 0.7±0.3 | 1 |
| Stroke death, n (%) | 29 (53) | 29 (53) | 1 |
| CMV status of the donors, n (%) | |||
| CMV-negative | 7 (13) | 7 (13) | 1 |
| CMV-positive | 37 (68.5) | 37 (68.5) | |
| CMV-unknown | 10 (18.5) | 10 (18.5) | |
Data are shown as mean and standard deviation or median and interquartile range.
Abbreviations: cPRA: calculated panel reactive antibody; ATG: anti-thymocyte globulin; DGF: delayed graft function; CIT: cold ischemia time; Tx: transplant; CMV: cytomegalovirus.
Mean serum creatinine and estimated glomerular filtration rate (eGFR) were similar between groups throughout follow-up. At week 4, eGFR was 45mL/min/1.73m2 (LCPT) vs. 41mL/min/1.73m2 (ER-Tac; p=0.256); at week 48, 49 vs. 51mL/min/1.73m2 (p=0.638).
Acute rejectionClinical acute rejection occurred in 23.4% (LCPT) vs. 28.3% (ER-Tac; p=0.817). Subclinical rejection on protocol biopsy was observed in 61% (LCPT) vs. 80% (ER-Tac; p=0.405).
PharmacokineticsLCPT required significantly lower total daily doses (TDD) than ER-Tac at all time points (week 48: 0.05 vs. 0.08mg/kg; p=0.006). LCPT achieved higher trough concentrations early post-transplant (days 2 and 7; p=0.007 and p=0.04, respectively), with higher bioavailability (Fig. 1).
(A) Tacrolimus TDD. Symbols indicating statistically significant differences between groups: *: p=<0.001; **: p<0.001; ***: p<0.001; †: p<0.001; ††: p<0.001; ‡: p<0.001; ‡‡: p=0.01; #: p=0.006. (B) Trough concentration of tacrolimus. Symbols indicating statistically significant differences between groups: *: p=0.007; ‡: p=0.04. (C) Bioavailability of tacrolimus. Symbols indicating statistically significant differences between groups: *: p=0.006; **: p=0.005; ***: p=0.001; †: p=0.001; ‡: p=0.001; #: p=0.001. The data are showed as mean±standard deviation. Abbreviations: TCT: trough concentration of tacrolimus; TDD: total daily dose.
Incidence of post-transplant diabetes was 27.8% (LCPT) vs. 35.2% (ER-Tac; p=0.407). Rates of CMV and BK virus infection were numerically lower in the LCPT group. Patient and graft survival were comparable.
DiscussionOur paired-kidney analysis demonstrates that LCPT offers significant pharmacokinetic advantages over ER-Tac, with lower required doses and higher early bioavailability, while maintaining similar efficacy and safety. These findings are consistent with previous studies showing improved bioavailability and reduced dose requirements with LCPT.4–7 The observed trend toward reduced subclinical rejection and improved early renal function with LCPT may be clinically relevant, given the association of early subclinical inflammation with long-term graft loss.8,9
Both formulations were well tolerated, with similar rates of adverse events. The lower infection rates and numerically reduced post-transplant diabetes in the LCPT group align with the hypothesis that improved pharmacokinetics may translate into fewer complications.10
Limitations include the single-center design and limited sample size for protocol biopsies. Nonetheless, the paired-kidney methodology strengthens the comparative analysis by minimizing donor variability.
ConclusionLCPT provides superior pharmacokinetic properties with a lower daily dose and higher early bioavailability compared to ER-Tac, without compromising efficacy or safety. Larger, multicenter studies are warranted to confirm these findings and evaluate long-term outcomes.
CRediT authorship contribution statementV.L. and D.H. participated in designing, data analysis, writing original draft preparation and funding acquisition. J.P.G., M.L., J.A.T., C.G., C.P., T.V. and P.R.E. participated in data collection and in writing review of the manuscript. All authors agreed with the final document.
Institutional review board statementThe study was conducted according to the guidelines of the Declaration of Helsinki, and approved by de Provincial Ethics and Clinical Research Committee of Malaga (Cei Provincial de Malaga) (protocol code: 11/2017/PI13 and date of approval: 28 November 2017).
Informed consent statementInformed consent was obtained from all subjects involved in the study.
FundingThis study was partly funded by grants from the Instituto de Salud Carlos III, Madrid, Spain (PI17/02043, ICI21/00042, and RICORS NetworkRD21/0005/0012), FONDOS FEDER and FIISC (PFIISC23/12).
Conflicts of interestThe authors declare no conflicts of interest.
We are grateful to the kidney transplant team at our center for their participation in the study, and to Maria Romero (Trialance, S.C.C.L.) for providing medical writing support.