Coronavirus disease 2019 (COVID-19) has been acknowledged pandemic by the World Health Organization. Critically ill cases of COVID-19 can develop severe complications (acute respiratory distress syndrome, multiple organ dysfunction, shock) or die.1 COVID-19 has high morbidity and mortality in patients with chronic kidney disease (CKD).2,3 Here we report a severe case presentation in which a COVID-19 patient with CKD stage 4 had satisfactory outcome through timely continuous venovenous hemodiafiltration (CVVHDF).
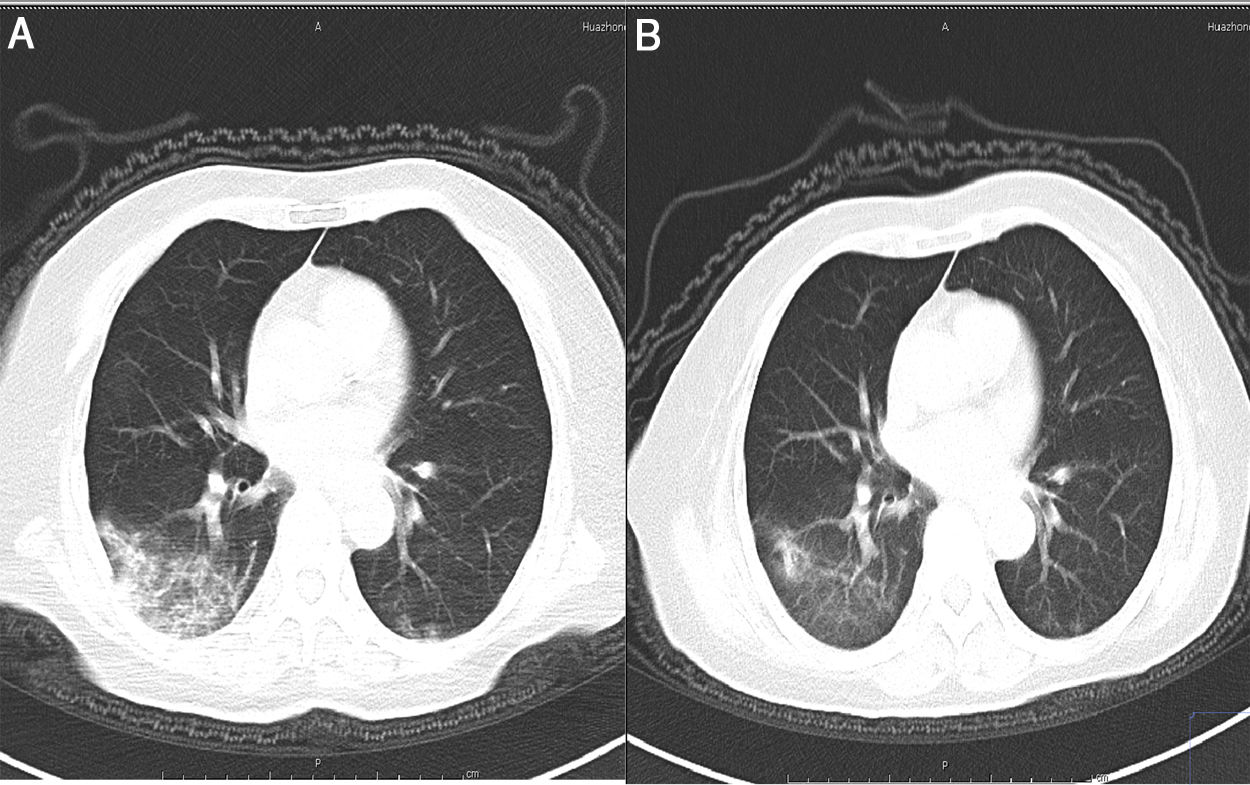
On February 11, 2020, a 74-year-old woman was referred to our hospital for “fever for 14 days and dyspnea for 4 days”. Nine days before her admission, diagnosis of this patient was confirmed by a positive SARS-CoV-2 reverse transcriptase-polymerase chain reaction testing (RT-PCR) test and chest CT in clinic and the antiviral drug arbidol was taken orally. On admission, her oxygen saturation was maintained 95% on the use of bi-level positive airways pressure (BiPAP). Blood sample tests revealed lymphopenia, increased neutrophil ratio and inflammatory cytokines, such as IL-2, IL-2 receptor (IL-2R), IL-6 and tumor necrosis factor-α (TNF-α) (Table 1). She had chronic kidney disease for 5 years and serum creatinine was generally maintained at 200μmol/L for 2 years. However, her serum creatinine was 657μmol/L on admission which revealed acute kidney injury (AKI). CT scan on the day of admission showed ground-glass opacity in both lungs. We showed the most severe lesion in Fig. 1A. On the second day of admission, vascular access was obtained via a flexible double-lumen catheter placed in the femoral vein. The patient underwent CVVHDF for 5 consecutive days and each lasted about 10h. Antivirus and antibiotics medications were also given. The patient released from the ventilator on the fifth day. Of note, plasma inflammatory cytokines concentrations and high-sensitivity C-reactive decreased after the CVVHDF (Table 1). Furthermore, serum creatinine decreased from 657umol/l to 302umol/l and remained stable within 7 days, and we removed the dialysis catheter. Chest CT showed remarkable absorption of lesions (Fig. 1B). From admission to discharge was totally 12 days.
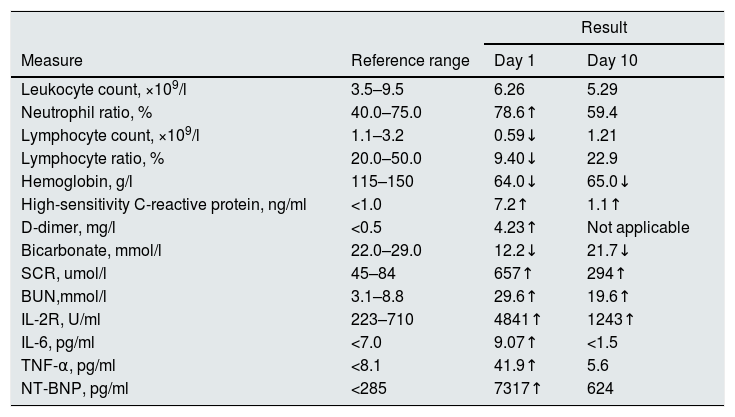
Clinical laboratory results.
| Result | |||
|---|---|---|---|
| Measure | Reference range | Day 1 | Day 10 |
| Leukocyte count, ×109/l | 3.5–9.5 | 6.26 | 5.29 |
| Neutrophil ratio, % | 40.0–75.0 | 78.6↑ | 59.4 |
| Lymphocyte count, ×109/l | 1.1–3.2 | 0.59↓ | 1.21 |
| Lymphocyte ratio, % | 20.0–50.0 | 9.40↓ | 22.9 |
| Hemoglobin, g/l | 115–150 | 64.0↓ | 65.0↓ |
| High-sensitivity C-reactive protein, ng/ml | <1.0 | 7.2↑ | 1.1↑ |
| D-dimer, mg/l | <0.5 | 4.23↑ | Not applicable |
| Bicarbonate, mmol/l | 22.0–29.0 | 12.2↓ | 21.7↓ |
| SCR, umol/l | 45–84 | 657↑ | 294↑ |
| BUN,mmol/l | 3.1–8.8 | 29.6↑ | 19.6↑ |
| IL-2R, U/ml | 223–710 | 4841↑ | 1243↑ |
| IL-6, pg/ml | <7.0 | 9.07↑ | <1.5 |
| TNF-α, pg/ml | <8.1 | 41.9↑ | 5.6 |
| NT-BNP, pg/ml | <285 | 7317↑ | 624 |
Scr, serum creatinine; IL-2, interleukin-2; IL-2R, IL-2 receptor; TNF-α, tumor necrosis factor-α; BUN, blood urea nitrogen; NT-BNP, N-terminal brain natriuretic peptide.
The successful treatment of this patient arouses our thinking. Is there a positive effect of continuous venovenous hemodiafiltration? According to the literature, the positive role of continuous renal replacement therapy (CRRT) is still no consistent conclusion in critically ill patients.4 CRRT has been applied to critically ill patients, including patients with SARS-CoV, MERS-CoV and other viral infectious diseases such as Ebola virus disease due to its accurate volume control, steady acid–base and electrolyte correction, and achievement of hemodynamic stability.5,6 A meta-analysis revealed that the use of continuous venovenous hemofiltration (CVVH) in critically ill patients with sepsis or acute respiratory distress syndrome (ARDS) was associated with a significant reduction in mortality at the longest follow-up available when compared to patients randomized to conventional therapy.7 A single-center randomized trial of 231 critically ill patients with AKI showed an absolute reduction in 90-day mortality on the use of CVVHDF.8 However, CRRT was associated with increased mortality in patients with MERS-CoV.5 In a prospective, randomized control study, survival at 28 days and recovery of renal function in critically ill patients with oliguric acute renal injury were not improved using CVVH.9 Studies on CRRT for COVID-19 patients are scarce, so whether CRRT has a positive effect on COVID-19 is uncertain.
Pneumonia caused by coronavirus infection, including SARS-CoV, Middle East respiratory syndrome coronavirus (MERS-CoV) and SARS-CoV-2 can cause a series of immune responses of T and B cells, and many cytokines and chemokines also participate in the inflammatory factor storm after coronavirus infection. The continuous existence of proinflammatory cytokines in circulation, leading to uncontrolled inflammatory response.10 CVVHDF is effective means clearing inflammatory cytokines, which can also promote homeostasis, improve hemodynamics and reduce systemic inflammatory response.4
The presented case report shows an elderly woman with history of CKD stage 4. On admission, the patient had hypoxemia and used BiPAP unit on admission. Her blood sample tests showed AKI, low bicarbonate, increased inflammatory cytokines. Both CT and clinical features demonstrated a severe case and indicated a high tendency being critically ill. Through timely CVVHDF and other supportive therapy, the patient achieved pneumonia cure and AKI recovery.
In conclusion, we have reported one such patient, and suggest there is a positive effect of continuous venovenous hemodiafiltration on the treatment of severe COVID-19 patients. Certainly, further high-quality randomized controlled trials, adequately powered for mortality, are needed to clarify the impact of CVVHDF.
Statement of ethicsInformed consent has been obtained from the patient for publication of the letter to editor and accompanying images. The study was approved by the medical Ethics Committee of Tongji Hospital Affiliated to Medical College, Huazhong University of Science and Technology (TJ-IRB20200422).
Funding sourcesThis work was supported by National Natural Science Foundation of China (NSFC 81974089, 81470934) and Science Foundation of Hubei Province (2018CFB554, 2019CFB675).
Conflict of interestNone.
The authors greatly appreciate all the Tongji hospital staff for their efforts in recruiting and treating patients and express gratitude to the patient.