Cystinosis is a rare monogenic autosomal recessive disorder caused by pathogenic variants in the CTNS gene, encoding cystinosin. Loss-of-function of cystinosin leads to intralysosomal cystine accumulation, resulting in cellular dysfunction and multisystem involvement. In addition to symptomatic treatment, early initiation of cysteamine therapy and its strict adherence are essential to delay kidney failure and minimize extrarenal complications. We report the case of a 28-year-old woman diagnosed with infantile cystinosis at two years of age, treated with oral and topical cysteamine since then. Genetic testing identified two CTNS truncating variants associated with the infantile form: c.519_520del p.(Thr173*) and c.18_21del p.(Thr7Phefs*7). Despite a relatively late diagnosis and an unapproved dosing regimen, her leucocyte cystine levels have consistently remained below the upper limit, and both renal and extrarenal manifestations are well-controlled. This case highlights the phenotypic variability of cystinosis and underscores the importance of sustained cysteamine therapy in achieving favorable long-term outcomes, even when initiated later and maintained with an unconventional dosing regimen.
La cistinosis es una enfermedad autosómica recesiva monogénica poco frecuente, causada por variantes patogénicas en el gen CTNS, que codifica para la cistinosina. La falta de funcionalidad de la cistinosina conduce a la acumulación intralisosómica de cistina, lo que provoca disfunción celular y afectaciones multisistémicas. Además del tratamiento sintomático, el inicio precoz de la cisteamina y el mantenimiento estricto del tratamiento son esenciales para retrasar el deterioro de la función renal y minimizar las complicaciones extrarrenales.
Presentamos el caso de una mujer de 28 años diagnosticada de cistinosis infantil a los dos años de edad, tratada con cisteamina oral y topical desde entonces. El análisis genético identificó dos variantes patogénicas en el gen CTNS, asociadas con la forma infantil: c.519_520del p.(Thr173*) y c.18_21del p.(Thr7Phefs*7). A pesar de un diagnóstico relativamente tardío y de un esquema posológico no autorizado, sus concentraciones de cistina leucocitaria se han mantenido consistentemente por debajo del límite superior, y tanto las manifestaciones renales como extrarrenales están adecuadamente controladas.
Este caso describe la variabilidad fenotípica de la cistinosis y destaca la importancia del tratamiento prolongado con cisteamina para obtenér resultados favorables, incluso si se inicia más tarde o se sigue un esquema posológico poco convencional.
Cystinosis (OMIM #219800) is a rare, monogenic, metabolic, autosomal recessive disorder, with an incidence of 0.5–1 per 100,000 live births worldwide.1,2 Cystinosis is caused by homozygous or compound heterozygous pathogenic variants in the CTNS gene, which encodes cystinosin, a lysosomal cystine transporter protein. Loss-of-function in cystinosin leads to cystine accumulation in lysosomes, affecting intracellular inflammatory and fibrotic pathways.3 The progressive accumulation of cysteine disrupts cellular homeostasis, leading to oxidative stress, apoptosis, and ultimately tissue damage in multiple organs.2
Clinically, cystinosis is a multisystem disorder that can affect kidneys, cornea, thyroid, gastrointestinal tract, reproductive system, cardiovascular system, lungs, skin, musculoskeletal system, and peripheral nerves.1,4 The severity and age of onset of these manifestations depend on specific genotype–phenotype correlations, allowing the differentiation of cystinosis into infantile, juvenile, or ocular phenotypes.5 Renal involvement, characterized by Fanconi syndrome and progressive chronic kidney disease, is one of the hallmark of cystinosis; without treatment, kidney failure (KF) typically develops within the first decade of life in the infantile form.3
Although incurable, symptomatic treatment with oral and topical eye-drops of cysteamine – a specific cystine-targeted therapy – can minimize extrarenal complications and delay KF by 6–10 years.1,6 The efficacy of cysteamine mainly depends on early initiation and adherence to treatment, which is often challenging due to the drug's dosing regimen and side effects.1 Patients’ compliance can be monitored by measuring leucocyte cystine levels, using the upper limit of normal found in heterozygous carriers as a reference (<1nmol/½ cystine/mg protein).1
Here, we present the case of a 28-year-old woman with infantile cystinosis, treated with cysteamine since the age of 2, who has shown unexpectedly excellent outcomes despite the late treatment initiation and an unconventional dosing regimen.
Case reportThe patient is a 28-year-old female diagnosed with cystinosis at 2 years of age following the detection of Fanconi syndrome and corneal cystine crystals. Since diagnosis, she has been treated with oral and topical eye-drops of cysteamine. Notably, her maternal aunt also had cystinosis, with severe disease progression and the onset of KF at six years of age (genetic data unavailable). Patient's genetic testing by using a next-generation sequencing panel7 identified two truncating variants in the CTNS gene (reference: NM_004937.3), classified as pathogenic according to ACMG criteria8: c.519_520del p.(Thr173*) inherited maternally, and c.18_21del p.(Thr7Phefs*7) of unknown origin due to unavailability of paternal testing. Although both variants are associated with infantile cystinosis,1,5 the phenotype related to the first variant is poorly described in the literature, while the latter is associated with significant phenotypic variability.9
Over the years, the patient has exhibited several disease manifestations, including osteopenia managed with active vitamin D supplements, hypokalemia treated with potassium supplements, mild corneal cystine deposits, primary hypothyroidism well-controlled with hormone therapy, delayed puberty and oligomenorrhea treated with estroprogestins, mild dysphagia, and mild myopathy of the feet and hands managed with carnitine supplements. She has a BMI of 18.4 with a height of 163cm and weight of 49kg, and the characteristic cystinosis phenotype including blond hair, pale skin, and blue eyes.1
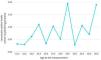
Despite her multisystem involvement, the genotype related to the infantile form, and the relatively late diagnosis, the 28-year-old woman has exhibited excellent clinical outcomes. Furthermore, although treated with oral cysteamine every 8h in order to assess compliance, her leucocyte cystine levels are frequently below the upper limit, with a median of 0.66 [IQR 0.34;1.07]nmol/½ cystine/mg protein (Fig. 1). She also maintains a well-preserved kidney function, with a serum creatinine of 74μmol/L (estimated glomerular filtration rate of 95mL/min/1.73m2) and a renal ultrasound revealing normal-sized kidneys with bilateral microlithiasis. Her urinary analysis is consistent with mild tubulopathy, characterized by tubular proteinuria with an urine protein–creatinine ratio of 653mg/g creatinine, hypercalciuria, hyperuricosuria, hypocitraturia, urine pH of 6.5–7.0, hyposthenuria with urinary density of 1004–1010, and polyuria (6L/day).
DiscussionAs a rare autosomal recessive disorder, cystinosis typically occurs in individuals without a positive family history of the disease. However, in this case, the patient's maternal aunt was also affected despite no known consanguinity. Due to the lack of genetic testing of the patient's maternal grandparents and aunt, further clarification of this unusual familial occurrence is not possible.
Cystinosis can be diagnosed using three methods1: corneal cystine crystals detection, leucocyte cystine measurement, and genetic testing. The patient's diagnosis was suspected firstly at 2 years of age due to Fanconi syndrome, and was subsequently confirmed by corneal cystine crystals detection, elevated leucocyte cystine levels, and genetic testing. Although paternal DNA was unavailable, the clinical and biochemical characteristics strongly suggest a trans configuration of the two truncating CTNS variants.
Currently, cysteamine remains the only disease-specific therapy for cystinosis, improving prognosis by delaying KF and mitigating extrarenal complications.1,6 Early treatment initiation and patient adherence to the strict dosing regimen are crucial to cysteamine's efficacy. Although the patient began treatment at 2 years of age – considered late for cystinosis6 – after more than 25 years, she developed only mild extrarenal manifestations, maintained well-preserved kidney function, and a mild tubulopathy managed with indomethacin and supplements. The explanation of this excellent outcome can rely on several factors, including the phenotypic variability of c.18_21del variant, the potential influence of genetic and epigenetic modifiers, and the patient's exceptional adherence, as confirmed by low leucocyte cystine levels despite an unapproved dosing regimen.
In conclusion, this case highlights the phenotypic variability of cystinosis, even in patients with truncating variants typically associated with the infantile form. It underscores the importance of early and sustained treatment in achieving favorable outcomes and suggest that factors beyond genotype, including epigenetic modifiers and treatment adherence, may play a significant role in disease progression and prognosis.
CRediT authorship contribution statementAll the authors provided care for the patient and contributed to writing the paper.
Patient consentThe patient gave informed consent to publish this case.
Conflict of interestThe authors declare that they have no conflict of interest.
The authors thank the patient whose medical history is described here. This study has been funded by the Instituto de Salud Carlos III (ISCIII)/FEDER funds (PI23/00426), and RICORS program to RICORS2040 (RD21/0005/0001) funded by European Union-Next GenerationEU.