In-patient hypertension is a common problem seen in the hospital setting. Current evidence-based guidelines define and address management of hypertension in ambulatory care and hypertensive emergencies in the hospital setting. However, they lack guidance for the management of acute asymptomatic/non-emergent hypertension in the hospitalised patient. The risk-benefit of treating inpatient asymptomatic hypertension is largely unknown. In this narrative review, we discuss current evidence-based perspectives to address this clinical entity.
La hipertensión de los pacientes ingresados es un problema frecuente en el ámbito hospitalario. Las directrices actuales basadas en la evidencia definen y abordan la gestión de la hipertensión en la atención ambulatoria y las urgencias hipertensivas en el ámbito hospitalario. Sin embargo, no hay orientaciones sobre la gestión de la hipertensión aguda asintomática/no urgente en el paciente hospitalizado. Se desconoce en gran medida la relación riesgo-beneficio del tratamiento de la hipertensión asintomática en los pacientes hospitalizados. En esta revisión narrativa analizamos las perspectivas actuales basadas en la evidencia para abordar esta entidad clínica.
Hypertension in hospitalized patients is a frequent problem. The prevalence of in-patient hypertension ranges from 50.5% to 70.2% with hypertension defined as ≥140/90mm Hg or mean 24-h BP>125/80mm Hg.1 The age adjusted prevalence of hypertension as a secondary diagnosis in hospitalised patients aged 35 years or older is estimated to be around 35% in men and 32% in women.2
The treatment decisions for hypertension management in the hospital are usually based on extrapolation of evidence-based guidelines intended for ambulatory patients. This approach may be unsuitable, as measurement of hypertension in the hospital setting does not follow many methodological requirements to ensure accurate measurement of blood pressure (BP) (for example, having the patient seated with back supported and feet on the floor, ensuring quiet surroundings, etc.). The circumstantial causes leading to elevated BP in the hospital such as anxiety, pain, anger and stress are often overlooked.
A unique phenotype of in-hospital hypertension called ‘green suit hypertension’ has been described in preoperative patients with high BP attributed to withholding anti-hypertensive drugs and anxiety of seeing their surgeons who typically wear green scrubs.3 There is no strong evidence that treatment based on the current guidelines for ambulatory hypertension improves outcomes in hospitalized patients. Nevertheless, for all practical purposes, hypertension management in-hospital remains dependent on current guidelines meant to guide out-patient care decisions.4 In this review, we discuss literature on the topic and propose an algorithmic approach to manage this scenario based on current evidence-based perspectives. Hypertension in pregnancy is excluded from the scope of this review.
Types of in-patient hypertensionThe spectrum of inpatient hypertension ranges from asymptomatic BP elevations with unknown clinical significance to severe elevated BP with evident hypertension mediated organ damage (HMOD) or potential life-threatening consequences.
Acute severe hypertension defined as systolic blood pressure (SBP)>180mm Hg is seen in 14% of admitted patients.5 Acute severe hypertension is classified into 2 types.
(a) Hypertensive urgency: An elevated BP of SBP>180mmHg and/or DBP>110–120mm Hg without HMOD.6 (b) Hypertensive emergency: An elevated BP of SBP>180mm Hg and/or DBP>110–120mm Hg with acute HMOD to heart, brain and microvasculature.6 Prompt identification and clinical differentiation of hypertensive crises is important for triage to intensive care and ascertaining need for oral or intravenous therapy.
The diagnosis of hypertension is often made in the in-patient setting. This could be long standing untreated hypertension or a transient acute elevation of BP. Systemic complications related to hypertension such as stroke, heart failure and renal dysfunction are usually the result of chronic uncontrolled hypertension rather than a single episode of acute elevation of BP. The significance and consequences of acute asymptomatic elevated hospital are unknown and there is no standard approach to treatment. The goal of managing elevated BP in this scenario should be to prevent possibility of HMOD and avoid unnecessary cancellation of scheduled procedures.3
Evaluation of in-patient hypertensionHerzog et al. classified in-patient hypertension to “significant hypertension” and “reactive hypertension where significant hypertension was defined as an acutely elevated BP which could lead to adverse outcomes.7 Reactive hypertension is an innocent bystander which resolves spontaneously and is unlikely to affect the hospital course.7 Most instances of elevated BP in the hospital are asymptomatic and do not need urgent pharmacotherapy. Differentiating significant hypertension from reactive hypertension should form the basis for investigating in-patient hypertension.
Causes of acute elevated BP in hospitalized patientApart from essential hypertension and secondary hypertension resulting from renal parenchymal/vascular disease, endocrine and cardiac disorders, certain secondary factors may cause acute elevation of BP in the hospitalized patient8,9 (Table 1).
Factors causing acute elevation of BP in hospitalized patients.
| 1. Pain |
| 2. Anxiety |
| 3. Urinary retention |
| 4. Acute distress |
| 5. Anti-hypertensive withdrawal |
| 6. Alcohol or narcotic withdrawal |
| 7. Peri-operative period |
| 8. Poorly controlled or undiagnosed pre-existing hypertension. |
| 9. Hypervolemia/inadvertent use of sodium containing intravenous fluids. |
| 10. Medications (erythropoietin, steroids, cyclosporine sympathomimetics, etc.) |
There is no universally acceptable guideline for BP measurement in bed-ridden hospital patients. An audit at a single centre in UK which closely observed practice of in-patient BP measurement (IPBPM) noted 100% deviation in IPBPM technique compared to BP measurement guidelines recommended by the National Institute for Healthcare Excellence (NICE) and European Society of Hypertension (ESH) for office BP monitoring which resulted in frequent overestimation of BP in the hospital setting.10 Measures to standardize IPBPM have been proposed which need further validation10 (Table 2).
In-patient blood pressure measurement (IPBPM).
| 1. BP monitor should be validated for clinical accuracy. |
| 2. Avoid automated BP monitoring in patients with arrhythmia or bradycardia. |
| 3. Document upper mid arm circumference, cuff size and patient posture during BP measurement. |
| 4. Measure BP in both arms and document the higher reading and arm. |
| 5. Ensure placement of cuff at heart level with arm and back supported. |
| 6. Document circumstances which influence BP like pain, anxiety, temperature or sleep. |
| 7. BP monitoring to be preferably done in silent environment. |
| 8. Repeat BP measurement and consider a third measurement if BP values are at extremes or substantially discordant (SBP>10mm Hg or DBP>5mm Hg. Record all measurements. |
| 9. Consider Manuel BP measurement by trained observers when automated BP not feasible. |
| 10. Ensure empty bladder before BP monitoring. |
Preliminary history and physical exam should be focused on identification of underlying hypertensive emergency. Once the possibility of hypertensive emergency has been excluded, history should be directed to understand the background for current admission, duration of hypertension, presence of pertinent symptoms, concurrent medication, alteration in treatment regimen, presence of comorbidities and any substance abuse (Table 3). A systematic physical exam can assist in confirming diagnosis of hypertension, possible duration (acute/chronic), HMOD and evidence of a cause of identifiable hypertension (Table 3).
History and physical examination of the hospitalized hypertensive patient.
| History |
| 1. Prior hypertension (duration, dosing and compliance with antihypertensive mediations) |
| 2. Past History: coronary artery disease, heart failure, stroke, chronic kidney disease, sleep thyroid disease, diabetes. |
| 3. Target organ injury: chest pain, shortness of breath, palpitations, headache, vision changes, seizures, reduced urine output, claudication. |
| 4. Family history: Family history of hypertension and kidney disease. |
| 5. Medication use: Non steroidal anti-inflammatory drugs (NSAID), oral contraceptives, anti depressants, corticosteroids, sympathomimetics (amphetamine, cocaine, phencyclidine). |
| 6. Risk factors: Smoking, alcohol, processed foods, physical inactivity. |
| Physical examination |
| 1. General exam: height, weight, waist circumference, abdominal circumference, body mass index (BMI) |
| 2. Optic fundus to identify hypertensive retinal changes, papilledema. |
| 3. Palpate for thyroid enlargement. |
| 4. Cardiopulmonary: left ventricular hypertrophy, cardiomegaly, auscultate for rales, cardiac gallop, inter scapular murmur, carotid bruit. |
| 5. Abdomen: palpable enlarged kidneys, masses, distended urinary bladder, mid-epigastric bruits or abnormal aortic pulsations. |
| 6. Neurology: signs of previous stroke, reduced grip, spasticity, hyperreflexia, Babinski sign, gait abnormality. |
| 7. Others: moon face, oedema, striae. |
Routine diagnostics are performed to evaluate for any underlying causes, end-organ damage and ascertain cardiovascular risk. These include glucose, urinalysis, creatinine with an estimated glomerular filtration rate (eGFR), electrolytes, thyroid profile, lipid profile and electrocardiogram (ECG). Ancillary testing is not recommended when managing acute hypertensive episodes unless indicated for other clinical reasons.11
Approach to treatment of in-patient hypertensionThere is no evidence-based approach to guide intervention thresholds or pharmacotherapy in hospitalized patients with elevated BP. A study on resident physicians’ approach to elevated in-patient BP showed that majority of residents based their decision of treatment on standard guidelines intended for out-patient hypertension management with a high discordance between medical and surgical residents (70–90% vs 19%, p<0.001) adapting this approach.12 Overall respondents were fairly aggressive in managing acute in-patient hypertension, with majority of them initiating pharmacotherapy of BP in excess of 160/100mm Hg and frequently adjusting anti-hypertensive regimens.12 The efficacy and safety of this approach is unclear.
Treatment of hypertensive emergencyWhen confronted with a hypertensive emergency there is a perceived need for intensification of antihypertensive therapy. The estimated in-hospital and one-year mortality for those with hypertensive emergency is 13% and 39%, respectively.13 All such patients need to be closely monitored in intensive care and treated with intravenous antihypertensives. The optimal therapy, choice of drug and goal of BP depends on etiologic factors causing the hypertensive emergency. However, there is insufficient evidence to conclude that lowering BP in hypertensive emergency reduces morbidity or mortality, except in conditions of abdominal aortic dissection and cerebrovascular accident.14–16 A Cochrane systematic review in 2008 found insufficient evidence to determine which drug or drug class is most effective for reducing mortality and morbidity due to hypertensive emergency.16 Rate of BP reduction is guided by autoregulatory principles and guidelines recommend BP to be reduced no more than 20–25% during the first hour and to be maintained at 160/100–110mm Hg during the next 6h.17 Therapy should be gradually transitioned from intravenous therapy to long acting antihypertensives to minimize risk of rebound hypertension.
Treatment of acute severe hypertension (hypertensive urgency)The one-year mortality of hypertensive urgency is around 9%.13 A retrospective propensity matched cohort study in patients with hypertensive urgency showed no significant difference in major adverse cardiac events (MACE) between those managed as out-patient compared to those referred to a hospital over 1week, 1 month and 6 month period.18 Another study of 549 patients with hypertensive urgency attending emergency room, reported a reduction in BP (20mm Hg decrease in systolic and 10mm Hg decrease in diastolic BP) in 32% patients with a 30-min rest period alone. The remaining patients who did not have reduction in BP with rest had satisfactory response with oral anti-hypertensives in a 2-h average follow-up period.19 In a retrospective cohort of 1016 adult primary hypertension patients, presenting with an initial BP>180/100mm Hg and no HMOD there was no difference between hospital revisits and mortality over a follow up of 30 days whether they were treated with anti-hypertensives or not.20 However, even in the absence of acute HMOD, hypertensive urgency has long term implications with increased risk of cardiovascular events in 2 years and five times higher risk of stroke in 3 years.21,22
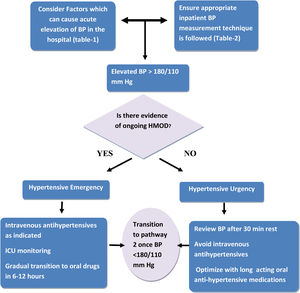
Despite the lack of evidence to support reduced short term morbidity and mortality with antihypertensives in acute elevated BP>180/100mm Hg, without target organ damage physicians feel compelled to treat the numbers, often with intravenous antihypertensives.12 There are concerns that using the term “hypertensive urgency” has led to overly aggressive management of severe uncomplicated hypertension.23 The 2017 American guidelines on hypertension advocate reinstitution or intensification of anti-hypertensive drugs with treatment of anxiety in treatment of hypertensive urgency.17 There is no indication for intravenous antihypertensives or immediate reduction of BP in such patients.17,24 We propose the approach shown in Fig. 1 for the management of acute severe hypertension in the hospitalized patient.
Treatment of acute hypertensionAccording to statistics of the American heart association (AHA), in 2005 there were 301,000 with a primary diagnosis of essential hypertension compared to 9,000,300 hospitalizations as a secondary diagnosis.25 Patients admitted for reasons other than a primary diagnosis of hypertension frequently have transient elevations in BP which are not categorized as acute severe hypertension (<180/110mm Hg). This often results in modification of their out-patient anti-hypertensive regimen or new prescriptions “as needed”. There are no studies designed to evaluate if this practice improves outcomes.
A study reported that 11% patients admitted to ICU with ≥1 episode of asymptomatic hypertension (BP>160/90mm Hg) were treated inappropriately with intravenous antihypertensives with a converse increase in BP in 14% of them.26 A report estimates 8.3 inappropriate intravenous anti-hypertensive orders per 1000 patient days with nearly half of them having an adverse event. They also designed an intervention by providing guidance for nurses on assessment for precipitating factors of hypertension such as anxiety, pain and HMOD through specific guided algorithms before contacting physicians. This intervention reduced intravenous hypertensive orders by 60% and number of adverse events (defined as>25% reduction in BP, change in heart rate by>20 beats per minute, or need for IV fluids) by 57% per 1000 patient days.27
In a retrospective propensity matched cohort of 4056 older adults (>65 years) with admission for three non-cardiac conditions (pneumonia, urinary tract infection or venous thromboembolism), discharge with intensified anti-hypertensive regimen was associated with increased risk of re-admissions and serious adverse events defined as hypotension, syncope, electrolyte abnormalities or acute kidney injury (AKI) at 30 days.28 Moreover there was no reduction in cardiovascular events or BP at 1-year follow-up.
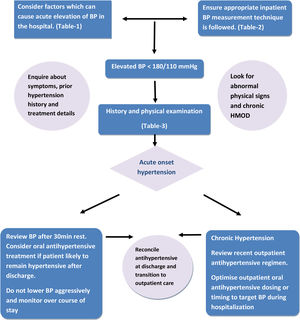
Overall current evidence does not support use of intravenous antihypertensives or intensive lowering of BP in these patients and suggests potential harm if BP is lowered rapidly. When considering treating acute hypertension in hospital physicians should meticulously exclude secondary factors (Table 1) resulting in increased BP followed by rest for at least 30min. The BP should be measured by correct technique and if the patient remains hypertensive, and likely to remain hypertensive post hospitalization, oral antihypertensives should be optimized. We propose the approach shown in Fig. 2 for the management of non-emergent hypertension in hospital.
Transition to out-patient hypertension careOverwhelming majority of physicians believe that is appropriate to discharge patients on the final anti-hypertensive regimen established during hospital course.12 Though this practice is reasonable for a diagnosis of ‘de novo’ hypertension during hospitalization, changing a previously established antihypertensive regimen prescribed by out-patient care provider may disrupt continuity of care.29 Patients may also stop the new medications due to adverse effects, unawareness of new regimen, pill burden or based on the advice of out-patient care provider who felt they were not indicated. Application of evidence-based knowledge by treating clinician, anti-hypertensive medication reconciliation at discharge, accurate communication between care providers with active patient and family involvement will ensure optimal transition of care.30
ConclusionThe management of hypertension in hospital is different from out-patient management. Acute severe hypertension with associated target organ damage (hypertensive emergency) should be treated promptly with close monitoring. Contrary to common practice, there is no evidence to support that aggressive lowering of BP with intravenous antihypertensives improve short term outcomes in acute severe hypertension without target organ damage (hypertensive urgency) and may result in potential harm. Decision to treat acute hypertension in hospital should be made after considering underlying factors like pain, stress, anxiety, medication side effects, etc. Whenever a new anti-hypertensive regimen is prescribed in hospital, communication and follow up with out-patient care provider may improve outcomes. Well-designed studies and randomized controlled trials are required to validate this proposed approach to manage inpatient hypertension.
Financial support declaredNone.
Conflicts of interestNone.