Hemodialysis patients, particularly the elderly, present challenges for vascular access (VA) creation due to age-related vascular changes and comorbidities. This study aimed to characterize outcomes related to VA in elderly patients (≥75 years) and compare them with younger patients, focusing on primary failure, maturation failure, and patency rates.
MethodsThis retrospective study included patients evaluated in VA consultations between January 2019 and December 2021; patients were evaluated through physical examination and Color Doppler Ultrasound to determine the suitability of vessels for VA construction. Demographic data, proposed and created VA types were assessed. The primary outcomes were the evaluation and comparison of primary failure and maturation failure of VA in the elderly (O) and younger (Y) groups. Secondary outcomes included the assessment of primary patency and primary assisted patency at 6, 12, and 24 months in both groups.
ResultsAmong 167 patients, 36 were elderly. There were no significant differences in proposed and created VA types between the Y and O groups and radial-cephalic AVFs were the most commonly constructed VA in both groups.
Primary and maturation failure rates were similar (Y group: 17.3% and 5.6%; O group: 9.7% and 10.7%, respectively). Primary patency and primary assisted patency rates did not significantly differ between groups at 6, 12, and 24 months.
ConclusionThe impact of age on the feasibility of VA should not be exaggerated. Preoperative assessment and a tailored approach enable successful autologous access creation in elderly patients, resulting in outcomes comparable to those of younger patients.
Los pacientes en hemodiálisis, particularmente los ancianos, presentan desafíos para la creación de acceso vascular (AV) debido a cambios vasculares relacionados con la edad y comorbilidades. Este estudio tuvo como objetivo caracterizar los resultados relacionados con el acceso vascular en pacientes ancianos (≥75 años) y compararlos con pacientes más jóvenes, enfocándose en el fracaso primario, el fracaso de maduración y las tasas de permeabilidad.
MétodosEste estudio retrospectivo incluyó pacientes evaluados en consultas de acceso vascular entre enero de 2019 y diciembre de 2021. Los pacientes fueron evaluados mediante examen físico y ecografía Doppler para determinar la adecuación de los vasos para la construcción de AV. Se evaluaron datos demográficos y los tipos de acceso vascular propuestos y creados. Los resultados principales fueron la evaluación y comparación del fracaso primario y el fracaso de maduración del acceso vascular en los grupos de ancianos (O) y jóvenes (Y). Los resultados secundarios incluyeron la evaluación de la permeabilidad primaria y la permeabilidad primaria asistida a los 6, 12 y 24 meses en ambos grupos.
ResultadosEntre 167 pacientes, 36 eran ancianos. No hubo diferencias significativas en los tipos de AV propuestos y creados entre los grupos (O vs Y) y las FAV radiocefálicas fueron las VA más comúnmente construidas en ambos grupos. Las tasas de fracaso primario y de maduración fueron similares (grupo Y: 17,3% y 5,6%; grupo O: 9,7% y 10,7%, respectivamente). Las tasas de permeabilidad primaria y permeabilidad primaria asistida no difirieron significativamente entre los grupos a los 6, 12 y 24 meses.
ConclusiónEl impacto de la edad en la viabilidad del acceso vascular no debe ser exagerado. La evaluación preoperatoria y un enfoque personalizado permiten la creación exitosa de acceso autólogo en pacientes ancianos, obteniendo resultados comparables a los de pacientes más jóvenes.
Hemodialysis (HD) is the most widespread renal replacement therapy.1 Functional and durable vascular access (VA) is needed for adequate treatment, leading to a better long-term patient prognosis.2
In the last 20 years, the global aging of hemodialysis patients has been documented, bringing difficulties to the creation and maintenance of VA.3,4 Older patients present challenges to nephrologists and vascular surgeons: they have an expectedly short lifespan, poor-quality veins from repeated punctures and multiple hospitalizations, and are more prone to atheroma and medial calcification of the radial or humeral arteries.5
Arteriovenous fistula (AVF) is classically preferred over prosthetic grafts or central venous catheters because it is associated with lower mortality, infection risk, and cardiovascular events.2 The vast majority of authors have shown that elderly patients have worse AVF outcomes, namely longer AVF maturation times, high risk of primary failure (up to 72%),6 and increased risk of patency loss.7 However, outcomes are difficult to compare since there is a wide range of reported VA patency rates, different classifications by age, comorbidities, definitions for patency, preoperative mapping, and the location of the VA.3,8
Primary failure and maturation failure increase the number of days of exposure to the central venous catheter, increase the number of interventions with VA, increase the costs, and shorten its lifespan. Considering the complications of AVF, the lower patient survival, and frailty, some authors prefer arteriovenous grafts or central venous catheters as a first-line approach in elderly patients.9
The proper functioning of AVF depends on the adequacy of vessels.10 Preoperative mapping of arm vessels with Color Doppler Ultrasound (CDU) before the creation of VA helps achieve a higher percentage of arteriovenous fistula, determine the feasibility of creating the VA and its best location, avoiding futile surgeries, and improve long-term outcomes.11–14 Preoperative evaluation with CDU in elderly patients can overcome challenges in this population.15 These data question whether age is a reason to exclude patients from access to the construction of autologous VA.
The primary objective of the study is to characterize the outcomes of VA in elderly patients, specifically, primary failure, maturation failure, and patency and to compare these results with those of a younger patient group.
Materials and methodsStudy design and participantsThis single-center retrospective study includes patients who attended VA consultations at Santo António University Hospital Center between January 2019 and December 2021. Inclusion criteria were: (a) age over 18 years; (b) the purpose of the consultation is vascular mapping for creating VA. All patients are advised to attend this consultation for VA planning before or after starting urgent hemodialysis with CVC.
A single nephrologist evaluated the patients and performed the physical exam and vascular mapping through CDU. After patient evaluation, the nephrologist proposed to the vascular surgeon team a specific type and location of VA: the proposed VA could be an AVF, arteriovenous graft (AVG), or CVC (the nephrologist will not suggest the construction of VA if the patient was a candidate for short-term kidney transplantation or if the patient chose peritoneal dialysis). Given the stability of renal function in some patients, it was suggested that the construction of VA be delayed.
Demographic data, weight, height, medical history, and specific information about chronic kidney disease were collected. During follow-up, we recorded the date and type of VA proposed by the nephrology team, the type of access created by the vascular surgery team, the date of hemodialysis initiation, and the access used during the first hemodialysis session.
The nephrologist followed patients in VA consultation until one month after the first hemodialysis through functioning VA. VA complications, the number and type of vascular interventions, and the need for subsequent VA creation were evaluated during follow-up.
Preoperative vascular evaluationA General Electric® ultrasound with a high frequency (7–15MHz) linear probe was used for measurements.
Physical and CDU assessment always began with non-dominant arm blood vessels; patients were supine without angling the elbow joint to avoid vessel compression. If technically possible, the superficial and deep venous systems were examined from the wrist to the axillary vein and axillary artery.
When the venous anatomy was acceptable for an AVF, the arterial examination was performed by palpating arterial pulses. The ulnar and brachial arteries were examined as alternative sources if the radial artery was unsuitable. The dominant arm was evaluated only when the non-dominant arm evaluation was unsatisfactory.
In our study, only vessels that met the minimum criteria were chosen – a venous luminal diameter of ≥2.5mm for radial-cephalic AVF and ≥3.0mm for proximal AVF (using a tourniquet) and continuity with proximal veins in the arm and arterial luminal diameter of ≥2.0mm. Vein compressibility and distensibility, distance from the skin surface, continuity with the deep venous system in the upper arm, and confirmation of the absence of ipsilateral central venous stenosis or occlusion were performed.
Vein distensibility was evaluated subjectively before and after tourniquet placement, and we did not measure vein distensibility by CDU. The presence of venous congestion and a reduced or absent respiratory variability in the axillary vein implied central stenosis exclusion by angiography before AV access creation.
The distensibility of the arterial wall was assessed by evaluation of the Doppler waveform in the radial artery during reactive hyperemia induced by reopening the fist after it had been clenched for two minutes (change from the high-resistance triphasic to low-resistance biphasic waveform) and resistance index (RI) was measured and considered the target <0.7.
Arterial inflow was also evaluated to exclude arterial stenosis. We did not propose AVF creation in three specific conditions. First, AVF was not created in the presence of calcifications of the feeding artery wall accompanied by a negative reactive hyperemia test in the artery. Second, anastomosis was not created distal to a stenosis above 50% in the radial artery. Third, we did not advocate AVF creation in the presence of a cubital artery with a stenosis, a diameter<1.5mm, or absence associated with radial artery arteriopathy due to the increased risk of primary failure with radial-cephalic AVF and of ischemia with proximal AVF. When high bifurcation of the brachial artery is found, resulting in a deeper and larger ulnar artery and a smaller and more superficial radial artery, the larger and deeper ulnar artery is recommended for anastomosis.
The forearm AVF location was preferred over the upper arm location. The patient's age alone is not an exclusion factor for constructing any VA. Clinical data, risk factors associated with maturation failure, and CDU findings were considered before making a final decision. The aim was to create a VA with a higher probability of success, reducing the time of dialysis CVC and the risk of maturation failure with the need for subsequent interventions.
When patients did not have arteries and veins suitable for AVF, we immediately attempted an AVG. The criteria for good arterial inflow and venous outflow for AVG were brachial artery lumen diameter≥3.0mm and axillary vein lumen diameter≥4.0mm, respectively.
A postoperative surveillance scan was planned 4–6 weeks after access creation to assess access maturation: patency, Qa, artery and vein diameter, presence of stenosis formation and measured flow in the fistula (ml/min), the vein diameter, and any abnormalities.
The creation of AV access involved a multidisciplinary strategy. The nephrologist made the type and location of the AV access proposal. Still, the surgeon in the perioperative period had the final word about AV access.
Definition of variables and outcomesThe primary objective of the study was to evaluate VA outcomes in elderly patients (aged 75 years and older, O group) and compare them with those in younger patients (under 75 years, Y group).
Five types of possible VA were recorded: radial-cephalic AVF (fed by the radial artery), proximal AVF (brachio-cephalic or brachio-basilic, fed by the humeral artery), AVG, and CVC.
The primary outcomes were the evaluation and comparison of primary failure and failure of VA maturation at eight weeks in the O and Y groups. Secondary outcomes were the evaluation of primary patency (PP) and primary assisted patency (PAP) at 6, 12, and 24 months in both groups.
Primary failure was defined as access failure due to early technical failures (intra-operative thrombosis or other complications or abandonment of the newly created AVF).
Maturation failure is defined as insufficient access flow to maintain dialysis or the inability to cannulate an AVF, if required, at eight weeks after surgery.
Primary patency is the interval from the time of access placement until any intervention designed to maintain or reestablish patency, access thrombosis, or the time of measurement of patency. Assisted primary patency is the interval from the time of access placement until access thrombosis or the time of measurement of patency, including surgical or endovascular interventions designed to maintain the functionality of a patent access.16
A sub-analysis was also conducted to compare patients who, during follow-up, did not undergo VA construction with those who did, to determine if any differences between these groups could explain the outcomes observed in the comparison of VA outcomes between O group and Y group.
Statistical analysisData were analyzed in each group (O group and Y group) and compared between them. Categorical variables were expressed as absolute counts and percentages. Continuous variables were presented as mean±standard deviation if normally distributed.
Both groups used survival evaluations to estimate PP and PAP with Kaplan–Meier curves. The log-rank test assessed the differences between the groups in the Kaplan–Meier analysis.
The association between the variables and each outcome was studied using the Chi-square and Fisher exact tests in nominal variables, according to the sample size. We used univariate logistic regression to continuous variables.
In all these tests, we obtained the odds ratio with a confidence interval of 95%; the significance level was 0.05. All statistical analyses were performed using SPSS-IBM.
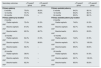
ResultsDemographic characteristicsIn this study 167 patients were evaluated and divided into two study groups according to their age at the first evaluation: younger than 75 years (“Y” group) and older than or equal to 75 years (“O” group) (Table 1).
Demographic characteristics distributed by groups.
| Demographic characteristics | <75 yearsY group | ≥75 yearsO group | p value |
|---|---|---|---|
| Patients, n (%) | 131 (78.4)1 | 36 (21.6)1 | |
| Age, years | 57.3±13.70 | 81.1±4.80 | |
| Sex | |||
| Male | 77 (58.8)1 | 23 (63.9)1 | 0.580+ |
| Female | 54 (41.2)1 | 13 (36.1)1 | |
| Proteinuria, g/g creatinine | 2.0±2.70 | 2.1±2.20 | 0.764* |
| Body mass index (BMI), kg/m2 | 26.3±5.40 | 25.0±4.30 | 0.235* |
| Time between the first consultation and the decision to creation VA, months | 3.0±6.30 | 1.1±3.50 | 0.028* |
| Time between decision and construction of VA, days | 26.5±24.60 | 30.5±40.20 | 0.490* |
| Time between the first consultation and creation of VA, months | 3.4±5.90 | 1.8±3.90 | 0.083* |
| Glomerular filtration rate (GFR) at first evaluation, ml/min | 16.2±9.30 | 12.8±4.00 | 0.055* |
| Serum creatinine at first evaluation, mg/dl | 4.6±2.20 | 4.6±1.60 | 0.953* |
| Glomerular filtration rate at the time of construction of the first VA, ml/min | 13.1±4.40 | 12.1±2.70 | 0.321* |
| Serum creatinine at the date of construction of the first VA, ml/min | 5.5±2.50 | 4.9±1.40 | 0.113* |
| Etiology of chronic kidney disease | |||
| Diabetic nephropathy | 35 (26.7)1 | 12 (33.3)1 | 0.434+ |
| Glomerulonephritis | 26 (19.8)1 | 4 (11.1)1 | 0.227+ |
| Pyelonephritis/interstitial nephritis/tubulointerstitial nephritis | 9 (6.9)1 | 2 (5.6)1 | 1.000 |
| Polycystic kidney disease | 11 (8.4)1 | 1 (2.8)1 | 0.465 |
| Amyloidosis | 5 (3.8)1 | 3 (8.3)1 | 0.371 |
| Other | 18 (13.7)1 | 5 (16.7)1 | 0.658+ |
| Not determined | 27 (20.6)1 | 8 (22.2)1 | 0.833+ |
| Comorbidities | |||
| Diabetes mellitus | 50 (38.2)1 | 18 (50.0)1 | 0.201+ |
| Ischemic coronary disease | 25 (19.1)1 | 15 (41.7)1 | 0.005+ |
| Peripheral arterial disease | 16 (12.2)1 | 8 (22.2)1 | 0.129+ |
| Stroke | 13 (9.9)1 | 5 (13.9)1 | 0.545 |
| Renal transplant | 29 (22.1)1 | 1 (2.8)1 | 0.006 |
The Y group consisted of 131 patients with a mean age of 57.3±13.7 years, predominantly male (58.8% male; 41.2% female). The O group included 36 patients with a mean age of 81.1±4.8 years, with a higher proportion of males (63.9% male; 36.1% female).
Regarding the etiology of chronic kidney disease (CKD), the leading cause in both groups was diabetic nephropathy (26.7% in the Y group and 33.3% in the O group, p=0.434). A considerable percentage of patients did not have a known etiology of CKD (20.6% in the Y group vs 22.2% in the O group). No differences were observed between the two groups regarding the etiology of kidney disease.
The most frequent comorbidity in both groups was diabetes mellitus (38.2% and 50.0% in Y and O groups, respectively, p=0.201); ischemic coronary heart disease was much more prevalent in the elderly group (19.1% vs 41.7%, p=0.005). The prevalence of diabetes mellitus, peripheral arterial disease, and prior stroke did not differ significantly between the two groups. Younger patients had a higher prevalence of previous kidney transplant (22.1% in the Y group vs 2.8% in the O group, p=0.006).
Among the 167 patients evaluated, 141 (83.4%) underwent VA construction, while 26 did not proceed due to stable kidney function, death, or a change in treatment option. When comparing these two patient groups, except for serum creatinine at the initial evaluation, which was significantly higher in the group that underwent VA construction (4.9±0.2mg/dl vs. 3.5±0.3mg/dl, p=0.003), no other significant differences were observed (Table 2). The demographic characteristics, the etiology of chronic kidney disease, as well as the presence of comorbidities such as diabetes mellitus, ischemic coronary disease, peripheral arterial disease, stroke, and previous renal transplant, were comparable between patients who did or did not undergo VA construction during follow-up.
Demographic characteristics distributed by vascular access construction status.
| Demographic characteristics | Patients without vascular access construction | Patients with vascular access construction | p value |
|---|---|---|---|
| Patients, n (%) | 26 (15.4) | 141 (83.4) | – |
| Age, years | 63.2±3.0 | 62.2±1.3 | 0.787* |
| Sex | |||
| Male | 19.0 (73.1) | 81.0 (57.4) | 0.135+ |
| Female | 7.0 (26.9) | 60 (42.6) | |
| Proteinuria, g/g creatinine | 1.2±0.2 | 2.2±0.2 | 0.099* |
| Body mass index (BMI), kg/m2 | 25.9±1.2 | 26.0±0.5 | 0.907* |
| Glomerular filtration rate (GFR) at first evaluation, ml/min | 18.6±1.9 | 14.9±0.8 | 0.065* |
| Serum creatinine at first evaluation, mg/dl | 3.5±0.3 | 4.9±0.2 | 0.003* |
| Etiology of chronic kidney disease | |||
| Diabetic nephropathy | 5 (19.2) | 42 (29.8) | 0.271 |
| Glomerulonephritis | 6 (23.1) | 24 (17.0) | 0.420 |
| Pyelonephritis/interstitial nephritis/tubulointerstitial nephritis | 1 (3.8) | 10 (7.1) | 1.000 |
| Polycystic kidney disease | 0 (0.0) | 12 (8.5) | 0.217 |
| Amyloidosis | 2 (7.7) | 6 (4.3) | 0.612 |
| Other | 6 (23.1) | 18 (12.8) | 0.219 |
| Not determined | 6 (23.1) | 29 (20.6) | 0.773+ |
| Comorbidities | |||
| Diabetes mellitus | 9 (34.6) | 59 (41.8) | 0.491+ |
| Ischemic coronary disease | 8 (30.8) | 32 (22.7) | 0.375+ |
| Peripheral arterial disease | 2 (7.7) | 22 (15.6) | 0.376 |
| Stroke | 3 (11.5) | 15 (10.6) | 1.000 |
| Renal transplant | 6 (23.1) | 24 (17.0) | 0.420 |
No statistically significant differences in proposed access were documented between the Y and O groups (Table 3). In both groups, the main VA proposed by the nephrology team was the radial-cephalic AVF (41.2% in the Y group vs. 44.4% in the O group, p=0.729), followed by the brachio-cephalic AVF (29.8% vs. 30.6%, p=0.927) and the brachio-basilic AVF (20.6% vs. 19.4%, p=0.878). AVG was proposed for a small number of patients in both groups (5.3% vs. 2.8%, p=1.000).
Proposed and created VA and primary outcomes by groups.
| Proposed and created vascular access | <75 yearsY group | ≥75 yearsO group | p value |
|---|---|---|---|
| Proposed access by nephrologist, n (%) | |||
| Radial-cephalic arteriovenous fistula | 54 (41.2)1 | 16 (44.4)1 | 0.729+ |
| Brachio-cephalic arteriovenous fistula | 39 (29.8)1 | 11 (30.6)1 | 0.927+ |
| Brachio-basilic arteriovenous fistula | 27 (20.6)1 | 7 (19.4)1 | 0.878+ |
| Arteriovenous graft | 7 (5.3)1 | 1 (2.8)1 | 1.000 |
| Central venous catheter | 1 (0.8)1 | 1 (2.8)1 | 0.386 |
| Do not create a VA (kidney transplantation or peritoneal dialysis) | 3 (2.3)1 | 0 (0.0)1 | 1.000 |
| Created vascular access, n (%) | |||
| Distal arteriovenous fistula | 45 (40.9)1 | 12 (38.7)1 | 0.826+ |
| Brachio-cephalic arteriovenous fistula | 42 (38.2)1 | 12 (38.7)1 | 0.957+ |
| Brachio-basilic arteriovenous fistula | 20 (18.2)1 | 7 (22.6)1 | 0.582+ |
| Arteriovenous graft | 3 (2.7)1 | 0 (0.0)1 | 1.000 |
| Created access corresponded to proposed access, n (%) | 97 (88.2)1 | 27 (97.1)1 | 1.000 |
| Primary outcomes | |||
| Primary failure, n (%) | 19 (17.3)1 | 3 (9.7)1 | 0.407 |
| Maturation failure, n (%) | 5 (5.6)1 | 3 (10.7)1 | 0.392 |
Central venous catheters were proposed for only one patient in each group: in one case (Y group), the patient was awaiting a living donor kidney transplant in the near future; in the other case (O group), the patient was frail and had a poor short-to-medium-term prognosis. In three patients from the Y group, VA was not proposed because they were candidates for preemptive kidney transplantation or had recently chosen peritoneal dialysis.
We did not identify any patient with a clear absolute contraindication to the construction of a VA due to cardiovascular reasons.
Created vascular accessIn the operating room, the vascular surgeon ultimately decides the type of VA. In the vast majority of cases, the constructed access matched the nephrologist's proposal in both groups, with no statistically significant differences (88.2% in the Y group vs. 97.1% in the O group, p=1.000). Patients who did not proceed with VA construction did so for the reasons previously described; importantly, none of these cases resulted from refusal by the vascular surgery team.
The main VA constructed in both groups was radial-cephalic AVFs (40.9% in the Y group vs. 38.7% in the O group, p=0.826) (Table 3). Only three AVGs were constructed, all in the younger group. One patient in the elderly group was proposed for a AVG but died before the procedure could be performed.
The interval between the first nephrological evaluation and the decision to create VA was longer in the younger group (3.0 months±6.3 vs. 1.1 months±3.5, p=0.028). However, the time between the decision and the surgical construction of the VA was short and similar in both groups (26.5±24.6 days in the Y group vs. 30.5±40.2 days in the O group, p=0.490).
Primary outcomePrimary failure and maturation failurePrimary failure was documented in 17.3% (n=19) of the patients in the Y group and 9.7% (n=3) of the patients in the O group, with no statistically significant differences (p=0.407). Maturation failure tended to be less frequent in the Y group (5.6%, n=5) compared to the O group (10.7%, n=3), but there were no statistically significant differences (p=0.407).
In the overall study population, the rates of primary and maturation failures were 15.6% and 5.7%, respectively.
Secondary outcomesPrimary patency and primary assisted patencyIn the Y group, primary patency at 6, 12, and 24 months was 75.6%, 70.7%, and 51.6%, respectively (Table 4; Fig. 1). In the O group, primary patency was 80.0% at six months and 72.0% at 12 months. No statistically significant differences between the groups were documented.
Description of primary patency and primary assisted patency at 6, 12, and 24 months.
| Secondary outcomes | <75 yearsY group | ≥75 yearsO group | <75 yearsY group | ≥75 yearsO group | |
|---|---|---|---|---|---|
| Primary patency | Primary assisted patency | ||||
| 6 months | 75.6% | 80.0% | 6 months | 84.2% | 88.1% |
| 12 months | 70.7% | 72.0% | 12 months | 84.2% | 88.1% |
| 24 months | 51.6% | – | 24 months | 80.0% | 88.1% |
| Primary patency by location | Primary assisted patency by location | ||||
| 6 months | 6 months | ||||
| Radial-cephalic AVF | 72.4% | 81.5% | Radial-cephalic AVF | 74.8% | 81.5% |
| Brachio-cephalic AVF | 81.8% | 88.9% | Brachio-cephalic AVF | 92.7% | 100.0% |
| Brachio-basilic AVF | 62.3% | 66.7% | Brachio-basilic AVF | 85.0% | 83.3% |
| 12 months | 12 months | ||||
| Radial-cephalic AVF | 64.3% | 81.5% | Radial-cephalic AVF | 74.8% | 81.5% |
| Brachio-cephalic AVF | 77.3% | 88.9% | Brachio-cephalic AVF | 92.7% | 100.0% |
| Brachio-basilic AVF | 62.3% | – | Brachio-basilic AVF | 85.0% | 83.3% |
| 24 months | 24 months | ||||
| Radial-cephalic AVF | 38.6% | – | Radial-cephalic AVF | 62.3% | 81.5% |
| Brachio-cephalic AVF | 57.9% | – | Brachio-cephalic AVF | 92.7% | 100.0% |
| Brachio-basilic AVF | 62.3% | – | Brachio-basilic AVF | 85.0% | 83.3% |
No statistically significant differences were documented between the Y and O groups in primary assisted patency. The primary assisted patency in the Y group was 84.2% at 6 and 12 months, and 80% at 24 months. In the O group, primary assisted patency at 6, 12, and 24 months was 88.1%.
DiscussionMultiple studies have included age as a covariate in the analysis of VA survival, yielding different results and often inconclusive findings.17 In this study, we retrospectively analyzed the main outcomes related to VA in elderly patients compared with younger patients.
Our main findings are as follows:
- -
Most patients over 75 years had vasculature compatible with the construction of autologous VA.
- -
We did not identify statistically significant differences between the approaches proposed by the nephrologist in both groups.
- -
We did not identify statistically significant differences between the VA constructed by the surgical team in both groups.
- -
We did not identify differences between the two groups in primary failure, maturation failure, primary patency, and assisted primary patency.
- -
The overall primary and maturation failure rates were very low.
Among all hemodialysis patients, the elderly is the group whose prevalence has increased the most in recent years.15 Due to the presence of multiple comorbidities, potential complications, and high rates of primary and maturation failure reported in some studies, many elderly patients use a central venous catheter as their VA18; some authors defended this strategy for the elderly population.19 Central venous catheters are associated with a worse prognosis at all ages compared to AVF or AVG20–22; however, some recent studies, particularly those using data from the United States, raise the possibility that this worse prognosis may be partially linked to patient characteristics rather than the type of VA.23,24
In our study, reflecting the philosophy of our center, advanced age alone is not an exclusion criteria for creating VA, and we promote the construction of autologous VA whenever possible; however, we follow an individualized approach for each patient to achieve the optimal VA, rather than adhering strictly to the “fistula first” policy in every case – this practice aligns with a very recently published perspective.25
The vast majority (97.2%) of elderly patients evaluated had vasculature (arteries and veins) compatible with the construction of autologous VA. These data are consistent with some studies in this population using preoperative evaluation with CDU. Olsha et al., in a retrospective analysis, showed that most patients over 80 years had adequate vasculature for autologous accesses, with AVG construction in only 12% of cases.15 In our study, only three AVGs were constructed, and none were in the elderly group (Table 3) – the global low number of AVGs can be explained by the effort to maintain an autologous access and by the center's longer experience with brachio-basilic fistulas,26,27 which, in other centers, are sometimes overlooked in favor of AVGs. Notably, about 20% of the proposed accesses in both groups were brachio-basilic fistulas.
We did not document differences between the types of accesses proposed by the nephrologist in each group. Some studies point to the benefit of proximal fistulas in elderly patients because they have a shorter maturation time28,29; a recent survey of octogenarian patients, with preoperative evaluation by CDU, supports the primary construction of brachio-cephalic AVFs in these patients due to the low rates of primary failure and high rates of patency, when compared to other locations.3 However, proximal fistulas are associated with a greater risk of hemodialysis access-induced distal ischemia and stenosis of the cephalic vein arch.30 In our study, clinical and CDU evaluations were independent of age, and proposals were based solely on clinical and ultrasound characteristics, preferring distal fistulas when possible. This approach justifies the high percentage of distal fistula proposals in both groups (41.2% in the Y group; 44.4% in the O group) (Table 3).
Additionally, we did not observe any differences in the types of VA constructed between the two groups, with a notable emphasis on the high percentage of radial-cephalic AVFs created in the O group (38.7%). This corroborates the alignment of criteria between nephrologist and vascular surgeons, with the proposed access matching the created access in 97% of cases in the elderly group.
One of our most important conclusions is the very low percentage of primary and maturation failure in both groups and the lack of differences between them. Many studies have shown that elderly patients are at increased risk of having poor quality blood vessels and worse surgical outcomes31,32; other studies contradict this,33 showing better results with a good selection of vessels.15 The varying definitions of “elderly,” different comorbidities, and definitions of VA outcomes make it difficult to compare studies with precision. We define advanced age as over 75 (and not “over 65 years old”), considering the increasing number of elderly patients on hemodialysis.
In our study, age does not significantly influence VA primary failure (17.3% in the Y group vs 9.7% in the O group). In a retrospective analysis involving 134 elderly patients, 88% of newly created accesses consisted of arteriovenous fistulas (AVFs) and were successful in most patients15 – the authors only advanced to the construction of VA when the diameter of the vein was greater than 3mm upon CDU assessment; this approach is similar to our methodology.
In this study, we document a very low maturation failure at eight weeks (4.8%) compared to what is described in the literature (6.3–33%),12,34 without differences in maturation failure at eight weeks between the groups. Our rigorous evaluation of vessels before proposing them for surgery may explain our reduced rate of maturation failure: when a vascular alteration that predicts maturation difficulties is identified (e.g., focal vein stenosis or significant lesions from previous punctures), that vein is not proposed for use in surgery. These findings align with evidence in the literature, specifically the study by Hossain et al., which documented the impact of preoperative vascular assessment on arteriovenous fistula maturation, showing an increased rate of maturation failure in the group where ultrasound was not performed (18% and 47%, respectively).14
We did not find statistically significant differences between the two groups in terms of primary and primary assisted patency. Furthermore, primary patency data at the 24-month mark for the “O group” were not included in the analysis due to the absence of follow-up data. At this point, patients in the “O group,” who had maintained vascular access patency without requiring intervention, were no longer under observation, as they had either started hemodialysis or were lost to follow-up due to death.
In elderly patients, primary patency rates at 1 and 2 years vary widely in the literature (43–74% and 29–67%, respectively)17,33,35; in our study, we documented a high primary patency of distal fistulas at 6 and 12 months in both groups. We also documented high primary assisted patency in the O group without statistical differences when compared with the Y group (Table 4).
Notably, in the elderly patient group, the primary assisted patency at 6, 12, and 24 months remained the same. All necessary interventions to maintain patency were performed within the first 6 months after VA construction, with no further interventions or loss of patency observed during the follow-up period.
Some current data suggest that our results in this field are also partially justified by the careful preoperative evaluation; recently, Torres et al. evaluated a prospective cohort that created AVF after CDU and compared the outcomes with previous cohorts without preoperative assessment. Primary patency in the first year increased with CDU (59.5–71.9%) and assisted patency at 1 and 2 years was significantly higher in the CDU group.36
Our findings align with those observed by other authors. Lok et al. studied the effect of age on AVF outcomes, reporting a cumulative 1-year survival of 75.1% in elderly patients and 79.7% in younger patients.17 Swindlehurst et al., using preoperative doppler evaluation, also reported similar results in the elderly compared to the youngest group over a 25-month follow-up period.37 However, in these two studies, the cutoff for “elderly patient” was lower (age over 65 years), which may favor the results in this population.
In the sub-analysis, we compared all evaluated patients who underwent VA construction with those who did not, aiming to evaluate any differing characteristics that could account for the outcomes observed between the Y and O groups. We found no significant differences in demographic characteristics, comorbidities, and the etiology of chronic kidney disease between the patients who did and did not undergo VA construction. This indicates that the observed outcomes between the Y and O groups were not influenced by selection bias related to the construction of VA.
Considering our results and the literature, we believe that no patient should be excluded from the evaluation for VA construction solely based on age, without prior assessment by CDU. Several factors contribute to the positive results observed in our study: the clinical and CDU evaluation by a single experienced nephrologist, the existence of a multidisciplinary team in constant communication, and the high experience of the surgical team.
Despite the favorable results, this study has some limitations:
- -
Although this study was conducted in a tertiary and VA reference center, it is a retrospective, single-center study.
- -
The lack of detailed data on vessel diameters may limit comparisons with other studies.
- -
There was a predominance of men in our population, which may have influenced the results.
- -
There is a significant difference in the number of patients between the two groups, which may affect the comparison and the statistical power of the study.
Prospective, multicentric studies using preoperative assessment in elderly patients are needed to validate these findings.
ConclusionsOur study shows exceptional outcomes in vascular access outcomes, with no significant differences in primary failure and maturation failure between older and younger patients. We believe that age alone should not be a barrier to creating vascular access for hemodialysis.
Preoperative mapping by an experienced professional, careful selection of vessels with appropriate characteristics and close collaboration between Nephrology and Vascular Surgery are crucial for achieving optimal vascular access outcomes.
FundingNo funding was provided.
Conflict of interestsNone.