Elderly patients have higher incidence rates of end-stage renal disease (ESKD) than younger individuals and represent the fastest-growing segment of the ESKD population worldwide.1–3 The decision to recommend kidney transplantation (KT) in elderly patients with ESKD is complex due to the high associated morbidity and mortality.4 Dusseux et al.5 developed a simple clinical screening score in France to identify elderly incident dialysis patients over 70 years old with an acceptable long-term prognosis, aiding in the selection of candidates for KT evaluation. This study aimed to assess the utility of this score in predicting 1-year post-KT mortality in patients older than 60 years and to determine the optimal cut-off point.
A retrospective cohort study was conducted, including all patients over 60 years who underwent KT at Hospital Privado Universitario de Córdoba between January 2009 and December 2015. The Dusseux et al. score5 was calculated at the time of transplantation. Points were assigned based on the following criteria: male (1 pt); age 75–80 (2 pts), 80–85 (5 pts), ≥85 (9 pts); diabetes (2 pts); ischemic heart disease (2 pts); peripheral vascular disease stage III–IV (5 pts); congestive heart failure stage I–II (2 pts), III–IV (4 pts); dysrhythmia (2 pts); chronic respiratory disease (2 pts); active malignancy (5 pts); severe behavioral disorder (6 pts); cardiovascular disease (1 pt); mobility: requires assistance with transfers (4 pts), totally dependent (9 pts); BMI 21–25 (1 pt), BMI <21 (3 pts); and temporary central vascular catheter (3 pts). A one-year follow-up was conducted, analyzing variables associated with mortality. Statistical analyses included t-tests or Mann–Whitney tests for continuous variables, and chi-square or Fisher's tests for categorical variables, as appropriate. Predictive capacity was assessed using the area under the curve (AUC), and the Youden Index J was applied to determine the optimal cut-off point, with corresponding sensitivity and specificity. Kaplan–Meier survival curves were constructed and compared using the log-rank test. Statistical significance was set at p<0.05.
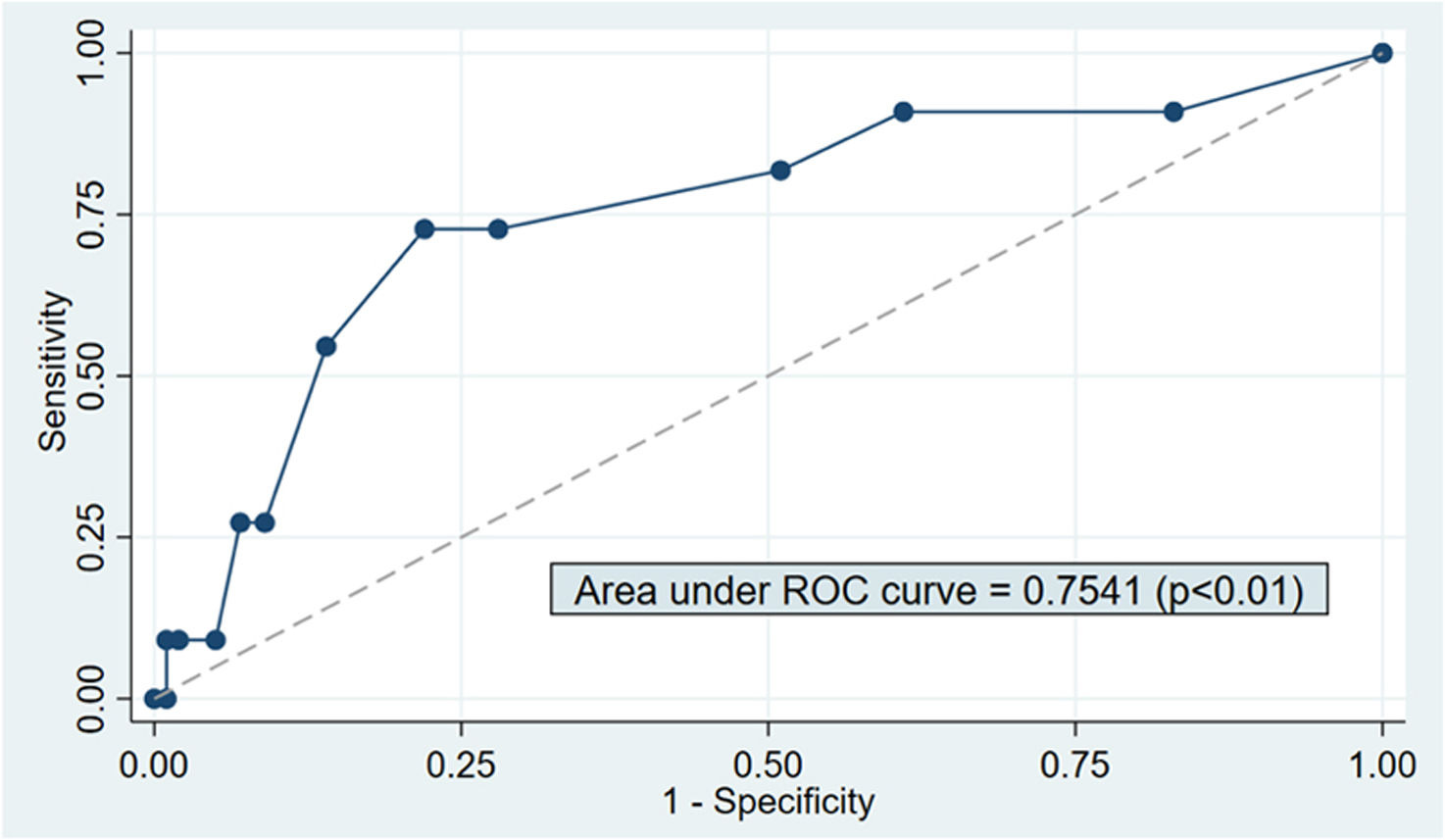
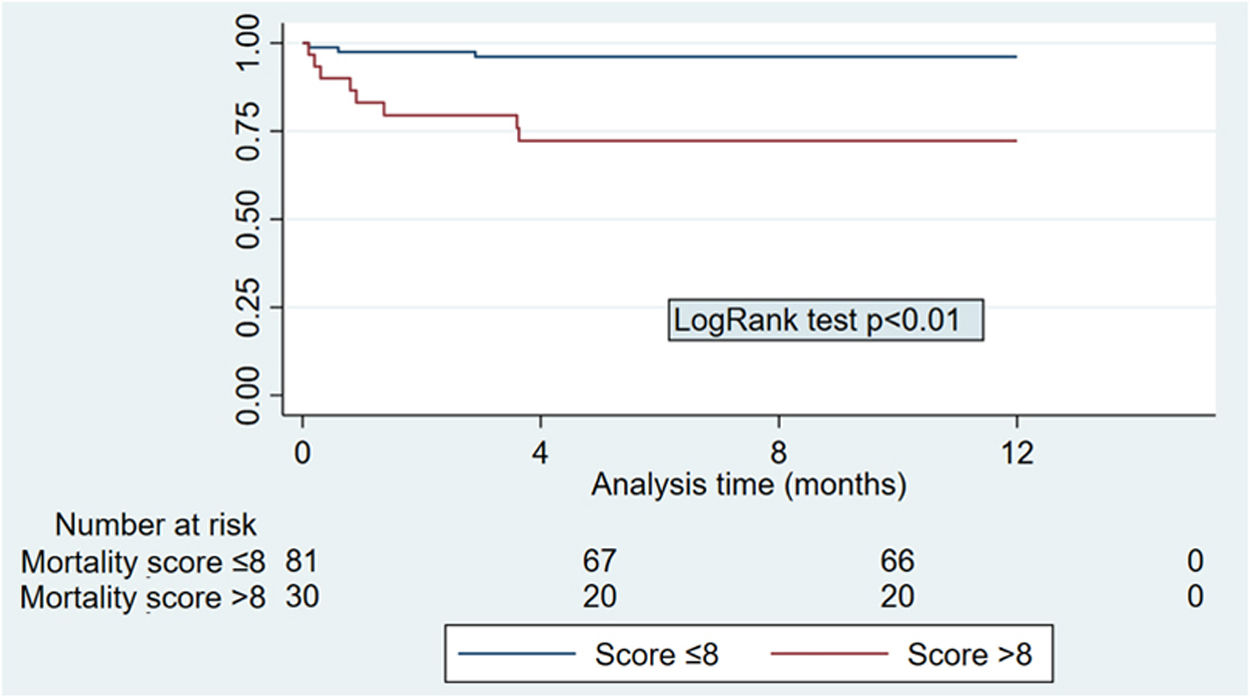
A total of 111 patients were included, with a mean age of 66.2±5.2 years; 54.9% were male. Relevant comorbidities included diabetes (30.7%) and ischemic heart disease (13.5%). The majority (82%) received a cadaveric KT. Induction therapy included steroids (100%), basiliximab (60.3%), thymoglobulin (22.5%), and gamma globulin (9.9%). Maintenance therapy consisted of steroids, tacrolimus, and mycophenolate (93.7%). The overall 1-year mortality rate was 9.9% (n=11), with infection being the leading cause (n=8), followed by cardiovascular disease (n=3). Patients who died were older (70.3±6.6 vs. 65.8±4.9 years; p=0.05), had a higher prevalence of ischemic heart disease (36.7% vs. 11%; p=0.04), and had a significantly higher Dusseux score at transplantation (9.4±3 vs. 6.8±2.5; p=0.02). No other significant differences were observed. The score demonstrated a strong predictive capacity for mortality (AUC=0.75; p<0.01; Fig. 1), with an optimal cut-off point of 8, yielding a sensitivity of 72.7% and specificity of 78%. Patients with a score >8 had a significantly higher mortality rate compared to those with a score ≤8 (26.7% vs. 3.7%; p<0.01). Survival curves differed significantly between these groups (p<0.01; Fig. 2).
The 1-year post-KT mortality rate in patients over 60 years in our study was approximately 10%, significantly lower than the 20–40% mortality rate reported for dialysis patients of the same age who do not undergo transplantation, as per the 2024 Argentine Chronic Dialysis Registry.6 However, this comparison should consider that some dialysis patients are not eligible for KT. The only significant mortality predictors identified were age, history of ischemic heart disease, and the Dusseux score. Originally developed to predict 3-year mortality in incident dialysis patients,5 this score also appears useful in predicting 1-year mortality post-KT. Furthermore, an optimal cut-off point (>8) was identified, demonstrating high sensitivity and specificity (70–80%). In Argentina, individuals are considered elderly from the age of 60, according to the definition established by the Inter-American Convention on the Protection of the Human Rights of Older Persons.7 This age threshold is also commonly used in the medical literature to define elderly kidney transplant recipients.8,9 Between 2015 and 2025, 25.6% of patients who received a kidney transplant in Argentina were aged 60 years or older, while only 6.4% were over 70.10 We chose to evaluate the score in recipients over 60 rather than over 70, as it may have broader applicability and clinical utility in our setting. Additionally, we applied the score exclusively to kidney transplant recipients, rather than to dialysis patients, given that we are a transplant center receiving referrals from across the country. Our aim was to assess a simple clinical tool capable of identifying high-risk patients, thereby facilitating personalized treatment and follow-up strategies.
The limitations of this study include its retrospective design, the small size of a single-center cohort, and a relatively low number of events. These factors limit the statistical power of the analysis and preclude the use of multivariate models, so the findings should be interpreted as exploratory. However, its strengths lie in providing local data on outcomes in this high-risk population and evaluating a mortality predictive score not previously validated in transplant recipients.
In conclusion, the Dusseux clinical score is a valuable predictor of 1-year post-KT mortality in patients over 60 years old. A score >8 effectively identifies high-risk patients, potentially guiding treatment and follow-up strategies to improve outcomes.
Ethical approvalTeaching and Research Committee of the Hospital Privado Universitario de Córdoba.
FundingThis research has not received any specific funding from public sector agencies, commercial sector or non-profit entities.
Conflicts of interestAll authors declare that they have no conflicts of interest.
To the Fundación Nefrológica de Córdoba.