An increase in neutrophils and a decrease in platelets have been correlated with a heightened risk of acute kidney injury (AKI) following cardiac surgery.
However, the combined metric of neutrophil-to-platelet ratio (NPR) and its association with post-surgery AKI risk has not yet been investigated.
ObjectiveTo explore the relationship between NPR and AKI risk within seven days following cardiac surgery.
MethodsData were downloaded from Medical Information Mart for Intensive Care, including patients after cardiac surgery. Both univariate and multivariate logistic regression models were employed to explore association between NPR and AKI risk within seven days post-operatively. A restricted cubic spline was employed to evaluate non-linear nature of this association. Subgroup analyses were performed to examine variations across different cohorts.
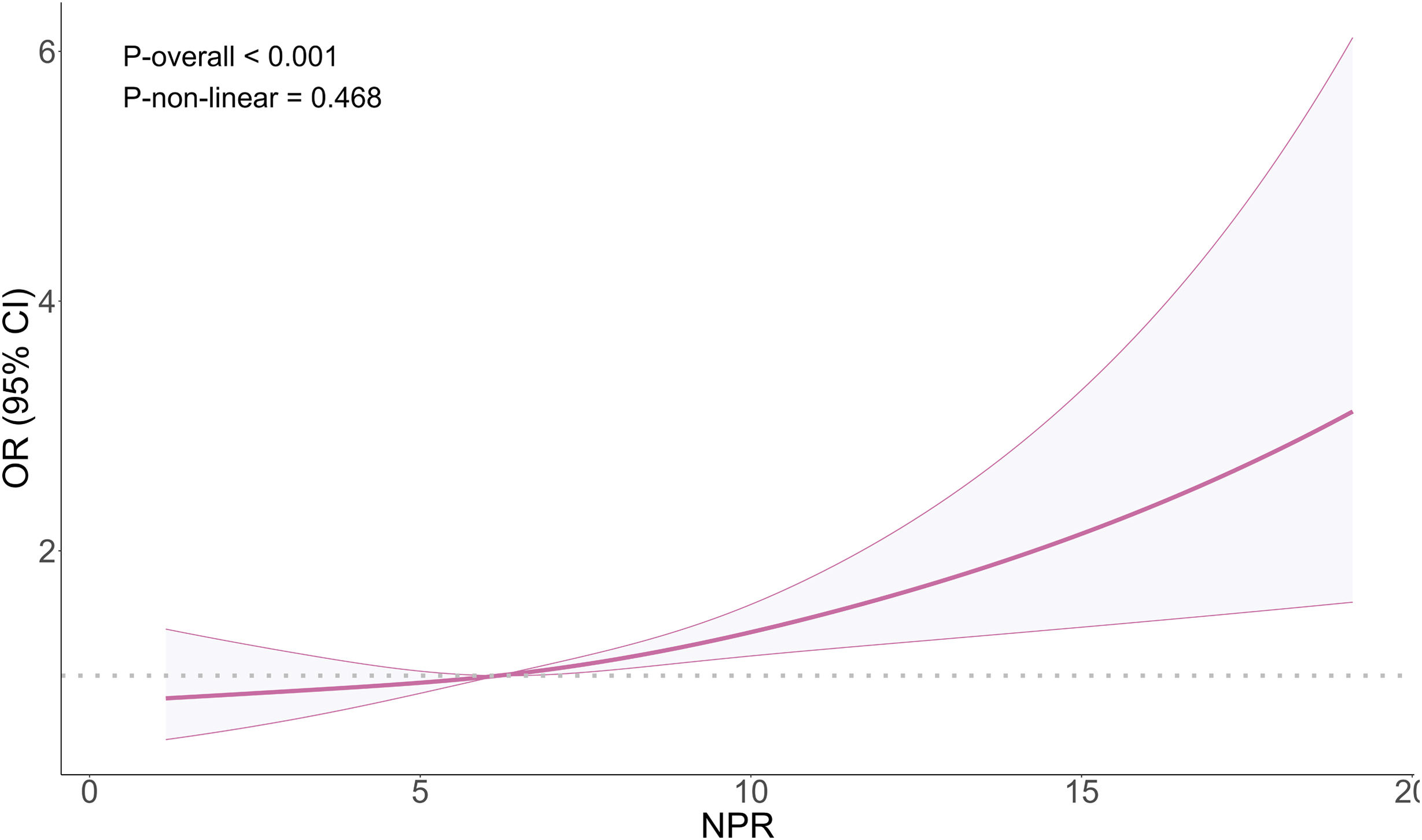
Results1702 patients were included, with an AKI incidence of 20.21% within the postoperative seven-day period. Logistic regression analysis revealed that, in fully adjusted models, the highest tertile (T3, NPR≥7.453) was significantly associated with an elevated AKI risk within seven days post-surgery (OR=1.500, 95%CI: 1.086–2.076, P=0.014). There was no significant non-linear relationship between NPR and AKI risk (P-overall=<0.001, P-non-linear=0.468). Notably, a significant interaction was observed in the subgroup receiving platelet transfusion (P interaction=0.005).
ConclusionIn adults undergoing cardiac surgery, an elevated NPR was linked to higher AKI risk. This finding offers a novel marker for the early identification of patients at high risk for AKI post-surgery.
Se han correlacionado el incremento de neutrófilos y la reducción de plaquetas con un aumento del riesgo de lesión renal aguda (LRA) tras la cirugía cardiaca.
Sin embargo, no se ha investigado la métrica combinada de la relación neutrófilos-plaquetas (NPR) y su asociación con el riesgo posquirúrgico de LRA.
ObjetivoExplorar la relación entre NPR y el riesgo de LRA dentro del plazo de 7 días desde la cirugía cardiaca.
MétodosLos datos fueron descargados de Medical Information Mart for Intensive Care (MIMIC), incluyendo los pacientes tras la cirugía cardiaca. Se utilizaron modelos de regresión logística tanto univariantes como multivariantes para explorar la asociación ente NPR y el riesgo de LRA dentro del plazo posquirúrgico de 7 días. Se utilizó un spline cúbico restringido para evaluar la naturaleza no lineal de esta asociación. Se realizaron análisis de subgrupo para examinar las variaciones en las diferentes cohortes.
ResultadosSe incluyeron 1.702 pacientes, con una incidencia de LRA del 20,21% dentro del periodo postoperatorio de 7 días. El análisis de regresión logística reveló que, en modelos totalmente ajustados, el tercil más alto (T3, NPR≥7,453) estuvo significativamente asociado a la elevación del riesgo de LRA dentro del plazo posquirúrgico de 7 días (OR=1,500; IC 95%: 1,086-2,076; p=0,014). No existió relación no lineal significativa entre NPR y el riesgo de LRA (P-general ≤0,001; P-no lineal=0,468. De manera notable, se observó una interacción significativa en el subgrupo que recibió la trasfusión de plaquetas (P interacción=0,005).
ConclusiónEn los adultos sometidos a cirugía cardiaca, se vincula una NPR elevada a un mayor riesgo de LRA. Este hallazgo ofrece un marcador novedoso para la identificación temprana de los pacientes con alto riesgo de LRA posquirúrgica.
Cardiovascular diseases are among the most serious dangers to human health in the twenty-first century.1 It is predicted that 1.5million cardiac operations are conducted worldwide each year.2 Acute kidney injury (AKI) is a common complication following cardiac surgery.3 A meta-analysis involving 320,086 patients revealed a global incidence rate of 22.3% for AKI associated with cardiac surgery.4 Due to the lack of effective treatment options, postoperative AKI is linked to higher morbidity and mortality, prolonged hospital stays, and increased healthcare expenses,5,6 imposing a substantial burden on patients and healthcare systems. Therefore, it is crucial to detect AKI risk early following cardiac surgery and implement appropriate preventive interventions.
Growing evidence suggests that biomarkers reflecting inflammatory status predict AKI occurrence following cardiac surgery. Increased neutrophil counts and reduced platelet counts have both been implicated in a higher AKI incidence after such procedures.7,8 However, individual indicators can be influenced by confounding variables. Consequently, neutrophil-to-platelet ratio (NPR) has evolved as a composite measure often used to evaluate inflammatory state and immune function in critically ill patients.9 Its predictive value in critical illness and cardiac surgery has also been established. Retrospective studies have indicated that elevated NPR is linked to elevated mortality in patients with acute aortic dissection and infective endocarditis.10,11 Furthermore, NPR can predict postoperative mortality risk in patients undergoing cardiac interventions following myocardial infarction, with higher NPR indicating a rising risk of all-cause mortality.12 Given this context, NPR may also serve as a predictor of AKI risk following cardiac surgery.
Thus, this study intended to delve into associations between NPR and postoperative AKI among patients who had cardiac surgery, utilizing data from Medical Information Mart for Intensive Care (MIMIC), so as to provide clinicians with a more reliable predictor for early screening of patients at high risk for AKI following cardiac surgery.
MethodsData SourceData was extracted from MIMIC-IV (https://mimic.mit.edu/). This publicly accessible resource contained patient data admitted to the intensive care unit of Beth Israel Deaconess Medical Center between 2008 and 2019. It has been approved for research purposes by the Institutional Review Board of the Massachusetts Institute of Technology and Beth Israel Deaconess Medical Center, and it has received a waiver for informed consent; thus, ethical approval was not required.13
Study populationDefinitions of cardiac surgery and diseasePatients who underwent cardiac surgery were screened using the International Classification of Diseases Ninth and Tenth Revision codes from the “procedures_icd” table in MIMIC-IV database14 (Table S1). The main outcome of this study was AKI occurring within 7 days after surgery, and its diagnosis was based on the Improved Global Kidney Disease Prognostic Organization Guidelines. More specifically, AKI following cardiac surgery was defined as an elevation in serum creatinine of 0.3mg/dL within 48h postoperative, or an increase to 1.5 times the baseline creatinine level (the lowest value recorded in the 24h prior to surgery) within seven days postoperatively.15 We did not utilize urine output criteria from guidelines, as prior evidence indicates that these standards are overly sensitive and non-specific for patients following cardiac surgery.16,17 To further analyze the pathogenesis of AKI, we divided patients into early AKI (≤72h after surgery) and late AKI (>72h after surgery) based on the time to first meeting AKI criteria. In addition, to provide a more comprehensive description of the clinical background of the study cohort, we defined the level of surgical urgency based on the admissions.admission_type field: “EMERGENCE”, “URGENT”, and “Directive EMER” were classified as emergency surgeries; “ELECTION”, “SURFACE SAME DAY ADMISSION”, and “OBSERVATION ADMIT” were classified as elective surgeries. Some patients have missing data in this field and cannot be classified.
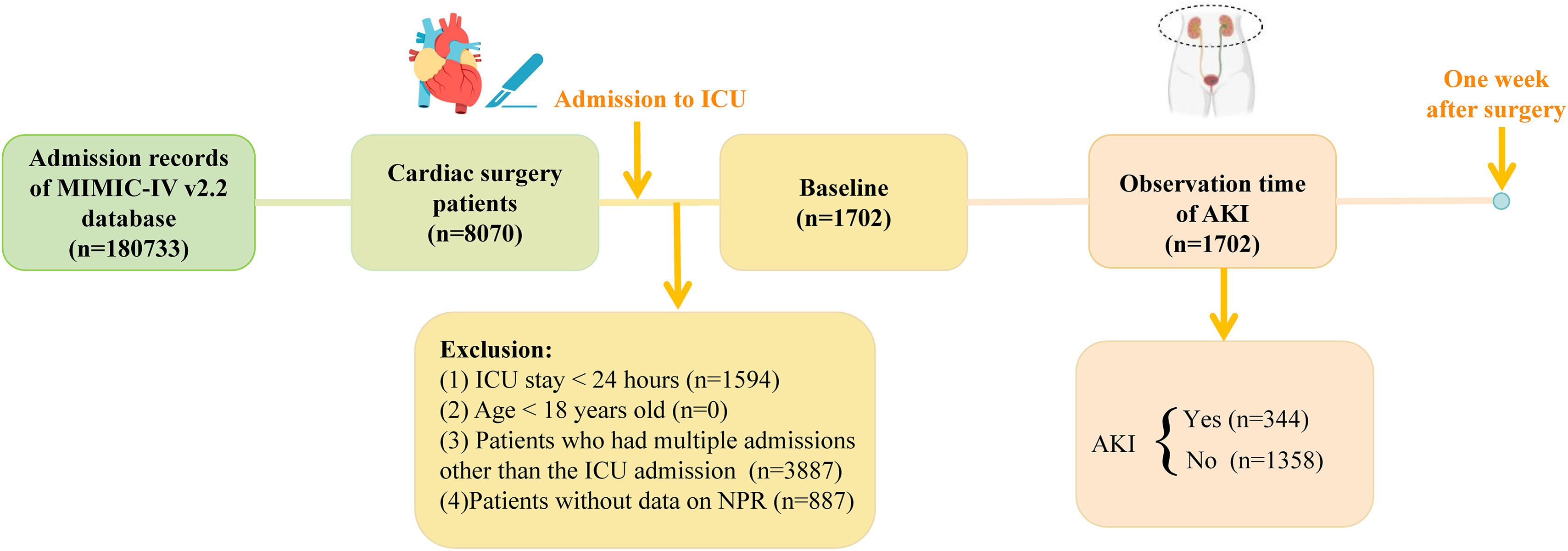
Inclusion and exclusion criteria8007 patients who had cardiac surgery were screened based on the following exclusion criteria: (1) patients with an ICU stay<24h (n=1594); (2) patients under 18 years of age (n=0); (3) patients with multiple ICU admissions beyond the first (n=3887); and (4) patients lacking NPR data (n=887). Ultimately, 1702 patients were included in the analysis, among whom 344 developed AKI within seven days post-surgery (Fig. 1).
Definition of NPRNPR is defined as the ratio of neutrophil count to platelet count, calculated using the formula: NPR=(Neutrophil count×100)/Platelet count.18
Variable informationIn this study, the structured query language of the Navicat Premium (version 16) platform was used to extract all variables from the MIMIC-IV database. The variables collected included the following dimensions: demographic information (age, gender, race, marital status), complications (diabetes, hypertension, heart failure, myocardial infarction, cerebrovascular disease and infective endocarditis), preoperative baseline indicators (baseline estimated glomerular filtration rate (eGFR), preoperative hemoglobin), early postoperative indicators (vital signs included heart rate, body temperature and blood oxygen saturation; laboratory examinations included blood glucose, anion gap, blood urea nitrogen, red blood cell count, creatinine, lymphocyte count and neutrophil count), and treatment measures (diuretic use, vasoactive drug use, red blood cell infusion, platelet transfusion and intra-aortic balloon counterpulsation (IABP). Regarding data integrity, for vital signs and laboratory indicators, we excluded data with missing values of more than 20% of the total sample size, and no other variables were missing (Table S2).
Statistical analysisAll statistical analyses in this study were conducted using R software (version 4.4.1). Baseline characteristics were summarized using the “tableone” package, with categorical variables expressed as percentages (%), and inter-group comparisons tested by Chi-square test. Continuous variables underwent skewness testing; severely skewed data (Mean/SD<2) were represented as median (IQR), with Wilcoxon–Mann–Whitney tests for group comparisons. Normally distributed data were shown as mean±SD, with comparisons made using t-tests.
To investigate the association between NPR and AKI within 7 days after surgery, we established univariate and multivariate logistic regression models. The variables included in the multivariate model were systematically screened. Firstly, based on previous literature and clinical knowledge, the variables must be known risk factors or important potential confounding factors for AKI. Considering data integrity, only variables with a missing rate of less than 20% were retained. In addition, the collinearity between variables was evaluated by the variance inflation factor (VIF) to ensure that all selected variables had VIFs<4 (Table S3).
In terms of model construction, we adopted a hierarchical adjustment strategy: first, we established a Crude model without adjusting any factors, then adjusted demographic variables (age, gender, race, marital status) in Model 1, and finally further included all clinical variables that met the above screening criteria in Model 2, including preoperative complications, baseline renal function, laboratory indicators, vital signs, and treatment measures, to comprehensively control the confounding effect.
In addition, the “rms” package was employed to develop RCS to investigate non-linear relationship between NPR and AKI risk. Subgroup analyses examined variations in the association between NPR and AKI risk across cohorts.
All statistical tests were bilateral, with a P<0.05 meaning statistically significant.
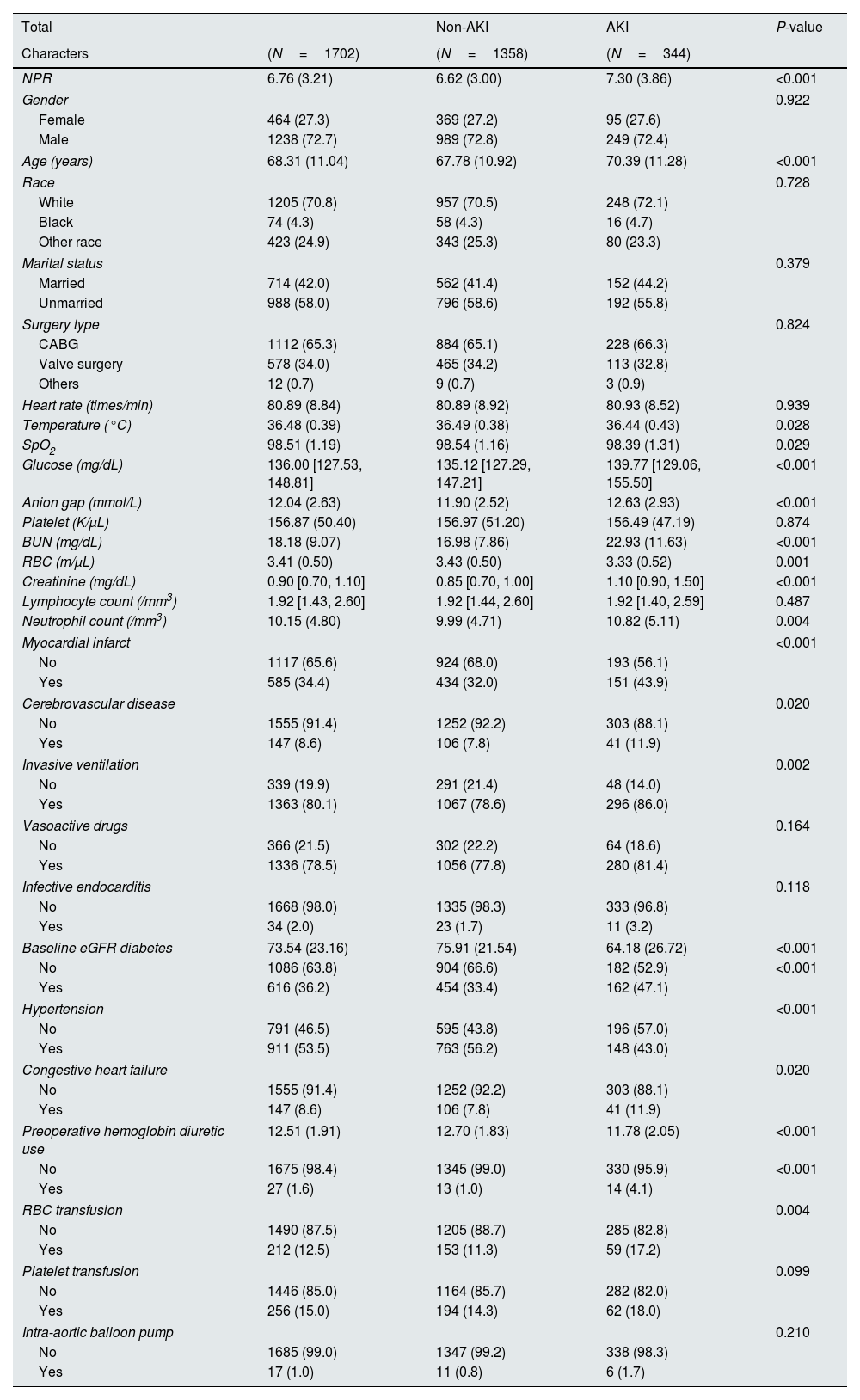
ResultsBaseline characteristicsThis study included 1702 patients who underwent cardiac surgery. Among them, 344 cases (20.21%) developed AKI within 7 days after surgery. Table 1 presents in detail the baseline characteristics of all patients. The overall cohort was dominated by males (72.7%), with an average age of 68.31±11.04 years. According to the classification of surgical urgency, there were 756 cases (44.4% each) of emergency surgery and elective surgery patients, with an additional 190 cases (11.2%) that could not be classified. Preliminary analysis showed that the incidence of AKI in the emergency surgery group was higher than that in the elective surgery group (22.4% [169/756] vs 18.9% [143/756]). Among all AKI patients, early AKI (≤72h postoperatively) accounted for the vast majority (299/344, 86.9%), while late AKI (>72h postoperatively) accounted for only 45 cases (13.1%). In addition, 17 patients (1.0%) used IABP, and there was no significant difference in its use between the AKI and non-AKI groups (P=0.210).
Participants characteristics of included patients when first ICU admission.
| Total | Non-AKI | AKI | P-value | |
|---|---|---|---|---|
| Characters | (N=1702) | (N=1358) | (N=344) | |
| NPR | 6.76 (3.21) | 6.62 (3.00) | 7.30 (3.86) | <0.001 |
| Gender | 0.922 | |||
| Female | 464 (27.3) | 369 (27.2) | 95 (27.6) | |
| Male | 1238 (72.7) | 989 (72.8) | 249 (72.4) | |
| Age (years) | 68.31 (11.04) | 67.78 (10.92) | 70.39 (11.28) | <0.001 |
| Race | 0.728 | |||
| White | 1205 (70.8) | 957 (70.5) | 248 (72.1) | |
| Black | 74 (4.3) | 58 (4.3) | 16 (4.7) | |
| Other race | 423 (24.9) | 343 (25.3) | 80 (23.3) | |
| Marital status | 0.379 | |||
| Married | 714 (42.0) | 562 (41.4) | 152 (44.2) | |
| Unmarried | 988 (58.0) | 796 (58.6) | 192 (55.8) | |
| Surgery type | 0.824 | |||
| CABG | 1112 (65.3) | 884 (65.1) | 228 (66.3) | |
| Valve surgery | 578 (34.0) | 465 (34.2) | 113 (32.8) | |
| Others | 12 (0.7) | 9 (0.7) | 3 (0.9) | |
| Heart rate (times/min) | 80.89 (8.84) | 80.89 (8.92) | 80.93 (8.52) | 0.939 |
| Temperature (°C) | 36.48 (0.39) | 36.49 (0.38) | 36.44 (0.43) | 0.028 |
| SpO2 | 98.51 (1.19) | 98.54 (1.16) | 98.39 (1.31) | 0.029 |
| Glucose (mg/dL) | 136.00 [127.53, 148.81] | 135.12 [127.29, 147.21] | 139.77 [129.06, 155.50] | <0.001 |
| Anion gap (mmol/L) | 12.04 (2.63) | 11.90 (2.52) | 12.63 (2.93) | <0.001 |
| Platelet (K/μL) | 156.87 (50.40) | 156.97 (51.20) | 156.49 (47.19) | 0.874 |
| BUN (mg/dL) | 18.18 (9.07) | 16.98 (7.86) | 22.93 (11.63) | <0.001 |
| RBC (m/μL) | 3.41 (0.50) | 3.43 (0.50) | 3.33 (0.52) | 0.001 |
| Creatinine (mg/dL) | 0.90 [0.70, 1.10] | 0.85 [0.70, 1.00] | 1.10 [0.90, 1.50] | <0.001 |
| Lymphocyte count (/mm3) | 1.92 [1.43, 2.60] | 1.92 [1.44, 2.60] | 1.92 [1.40, 2.59] | 0.487 |
| Neutrophil count (/mm3) | 10.15 (4.80) | 9.99 (4.71) | 10.82 (5.11) | 0.004 |
| Myocardial infarct | <0.001 | |||
| No | 1117 (65.6) | 924 (68.0) | 193 (56.1) | |
| Yes | 585 (34.4) | 434 (32.0) | 151 (43.9) | |
| Cerebrovascular disease | 0.020 | |||
| No | 1555 (91.4) | 1252 (92.2) | 303 (88.1) | |
| Yes | 147 (8.6) | 106 (7.8) | 41 (11.9) | |
| Invasive ventilation | 0.002 | |||
| No | 339 (19.9) | 291 (21.4) | 48 (14.0) | |
| Yes | 1363 (80.1) | 1067 (78.6) | 296 (86.0) | |
| Vasoactive drugs | 0.164 | |||
| No | 366 (21.5) | 302 (22.2) | 64 (18.6) | |
| Yes | 1336 (78.5) | 1056 (77.8) | 280 (81.4) | |
| Infective endocarditis | 0.118 | |||
| No | 1668 (98.0) | 1335 (98.3) | 333 (96.8) | |
| Yes | 34 (2.0) | 23 (1.7) | 11 (3.2) | |
| Baseline eGFR diabetes | 73.54 (23.16) | 75.91 (21.54) | 64.18 (26.72) | <0.001 |
| No | 1086 (63.8) | 904 (66.6) | 182 (52.9) | <0.001 |
| Yes | 616 (36.2) | 454 (33.4) | 162 (47.1) | |
| Hypertension | <0.001 | |||
| No | 791 (46.5) | 595 (43.8) | 196 (57.0) | |
| Yes | 911 (53.5) | 763 (56.2) | 148 (43.0) | |
| Congestive heart failure | 0.020 | |||
| No | 1555 (91.4) | 1252 (92.2) | 303 (88.1) | |
| Yes | 147 (8.6) | 106 (7.8) | 41 (11.9) | |
| Preoperative hemoglobin diuretic use | 12.51 (1.91) | 12.70 (1.83) | 11.78 (2.05) | <0.001 |
| No | 1675 (98.4) | 1345 (99.0) | 330 (95.9) | <0.001 |
| Yes | 27 (1.6) | 13 (1.0) | 14 (4.1) | |
| RBC transfusion | 0.004 | |||
| No | 1490 (87.5) | 1205 (88.7) | 285 (82.8) | |
| Yes | 212 (12.5) | 153 (11.3) | 59 (17.2) | |
| Platelet transfusion | 0.099 | |||
| No | 1446 (85.0) | 1164 (85.7) | 282 (82.0) | |
| Yes | 256 (15.0) | 194 (14.3) | 62 (18.0) | |
| Intra-aortic balloon pump | 0.210 | |||
| No | 1685 (99.0) | 1347 (99.2) | 338 (98.3) | |
| Yes | 17 (1.0) | 11 (0.8) | 6 (1.7) | |
NPR, neutrophil-to-platelet ratio; BUN, blood urea nitrogen; RBC, red blood cells; eGFR, estimated glomerular filtration rate.
The comparison between groups showed that the patients in the AKI group were older than those in the non-AKI group, and the proportion of patients with diabetes, myocardial infarction, heart failure, and cerebrovascular disease was higher (all P<0.05). In terms of laboratory indicators, patients in the AKI group showed higher blood glucose, anion gap, blood urea nitrogen, creatinine, neutrophil count, and NPR, but their eGFR, preoperative hemoglobin, body temperature, blood oxygen saturation, and red blood cell count were significantly lower (all P<0.05). In terms of treatment measures, the proportion of AKI patients receiving invasive ventilation, red blood cell transfusion, and diuretic therapy was significantly higher (all P<0.05).
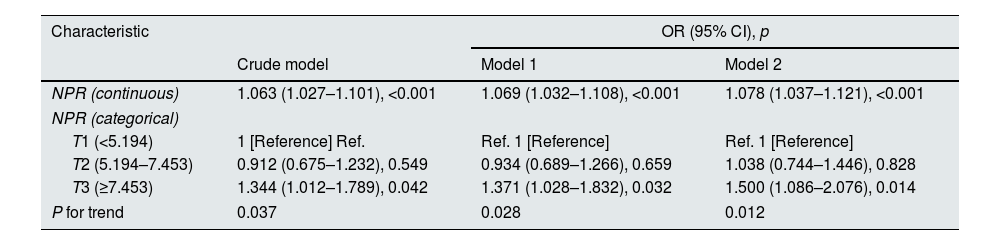
Association analysis between NPR and AKI risk within seven days post-surgeryLogistic regression analysis was conducted to investigate the relationship between NPR and AKI risk within seven days following cardiac surgery. The results are listed in Table 2. When NPR was analyzed as a continuous variable, three models adjusted for various confounding factors demonstrated a positive association between NPR and AKI risk: the crude model (OR: 1.063, 95% CI: 1.027–1.101, P<0.001), model 1 (OR: 1.069, 95% CI: 1.032–1.108, P<0.001), and model 2 (OR=1.078, 95% CI: 1.037–1.121, P<0.001).
Association analysis between NPR and postoperative acute kidney injury in patients undergoing cardiac surgery.
| Characteristic | OR (95% CI), p | ||
|---|---|---|---|
| Crude model | Model 1 | Model 2 | |
| NPR (continuous) | 1.063 (1.027–1.101), <0.001 | 1.069 (1.032–1.108), <0.001 | 1.078 (1.037–1.121), <0.001 |
| NPR (categorical) | |||
| T1 (<5.194) | 1 [Reference] Ref. | Ref. 1 [Reference] | Ref. 1 [Reference] |
| T2 (5.194–7.453) | 0.912 (0.675–1.232), 0.549 | 0.934 (0.689–1.266), 0.659 | 1.038 (0.744–1.446), 0.828 |
| T3 (≥7.453) | 1.344 (1.012–1.789), 0.042 | 1.371 (1.028–1.832), 0.032 | 1.500 (1.086–2.076), 0.014 |
| P for trend | 0.037 | 0.028 | 0.012 |
Note: Crude is unadjusted; model 1 adjusts age, race, gender and marital status; model 2 adjusts age, race, gender, marital status, heart rate, temperature, SpO2, glucose, anion gap, blood urea nitrogen, and red blood cells, creatinine, lymphocyte count, invasive ventilation, myocardial infarct, cerebrovascular disease, infective endocarditis, baseline eGFR, diabetes, hypertension, congestive heart failure, preoperative hemoglobin, diuretic, RBc transfusion, platelet transfusion, vasoactive drugs.
Further analysis of NPR stratified by tertiles revealed that with the increase of NPR percentile, the risk of AKI showed a significant upward trend (trend P values were all<0.05). In the fully adjusted model, patients had a significantly higher AKI risk in the highest tertile (T3, NPR≥7.453) than in the lowest tertile (T1, NPR<5.194) (OR=1.500, 95%CI: 1.086–2.076, P=0.014) (Table 2).
RCS assessed non-linear relationship between NPR and AKI risk. Results indicated a significant overall trend between NPR and AKI risk within seven days post-surgery (P<0.001), although no significant non-linear relationship was detected in the model adjusted for all confounding factors (P-non-linear=0.468) (Fig. 2).
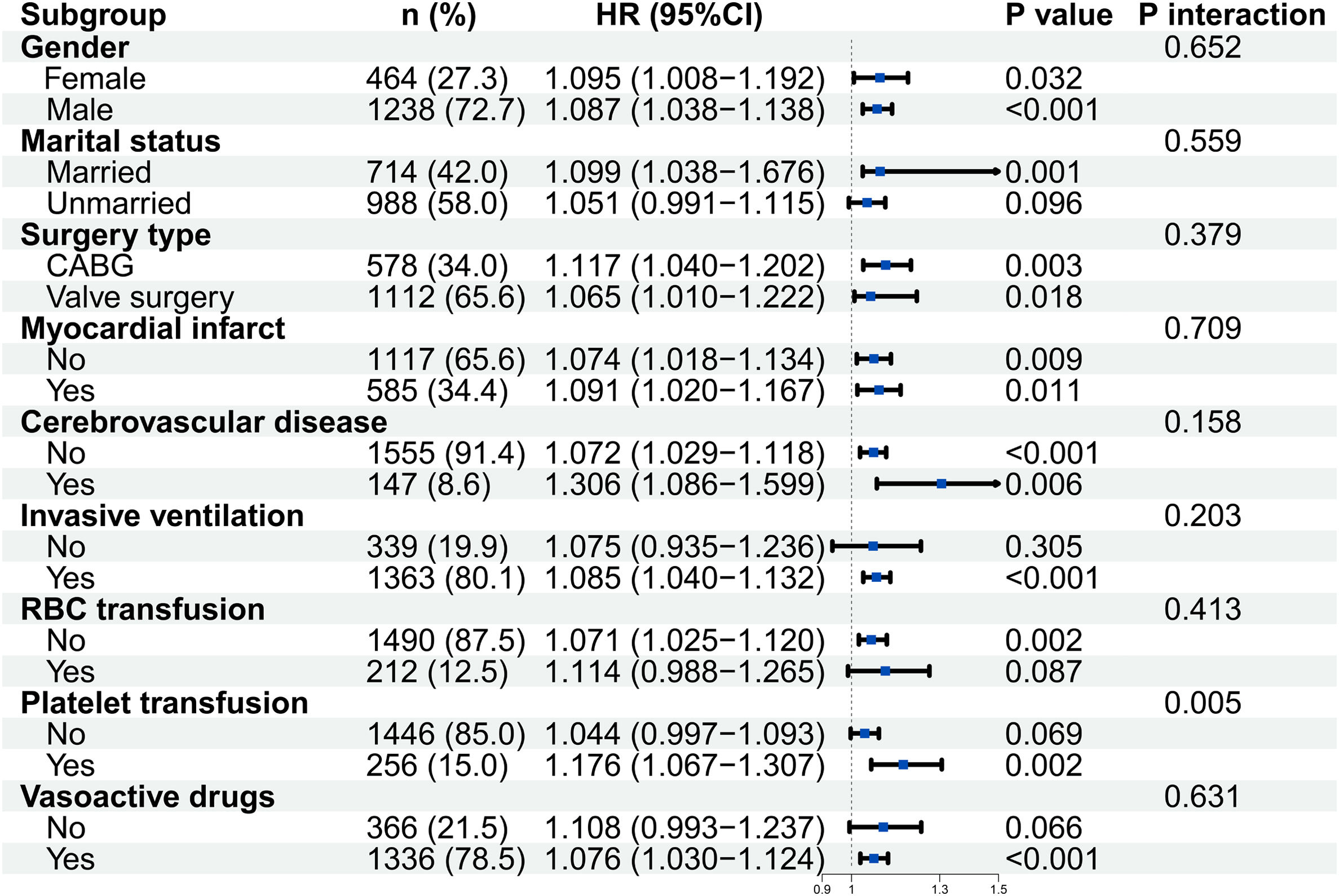
Subgroup analysisWe evaluated the stability of the association between NPR and postoperative AKI risk in different patient characteristics through subgroup analysis (Fig. 3). The interaction test showed that platelet transfusion was the only subgroup variable with significant interaction (P for interaction=0.005). In this subgroup, patients receiving platelet transfusion showed a stronger positive correlation between NPR and AKI risk (HR=1.176, 95% CI: 1.067–1.307, P=0.002). Although no significant interaction was observed in most other predetermined subgroups (all P for interaction>0.05), the positive correlation trend between NPR and increased AKI risk remained consistent and statistically significant in the vast majority of subgroups.
DiscussionThis study was based on a large intensive care database and systematically explored for the first time the association between NPR and AKI risk within 7 days after cardiac surgery. Our main findings are: (1) Elevated NPR was independently associated with the risk of AKI after cardiac surgery, and there was a dose-response relationship; (2) There was a linear positive correlation between NPR and AKI risk, and no significant nonlinear trend was found; (3) The vast majority (86.9%) of postoperative AKI were early events (occurring within 72h after surgery), highlighting the importance of direct surgical injury; (4) Subgroup analysis revealed that platelet transfusion was an important effector modifier associated with NPR and AKI, and NPR's predictive role in AKI risk was significantly enhanced in patients receiving platelet transfusion.
The pathophysiological mechanism of AKI after cardiac surgery is complex, with inflammatory response and microcirculatory dysfunction considered the core parts.19,20 Our research confirmed that NPR, a comprehensive indicator of neutropenia (representing inflammatory activation) and thrombocytopenia (possibly reflecting consumptive coagulation disease or bone marrow suppression), is a potent predictor of postoperative AKI. After adjusting for a wide range of confounding factors, including demographic characteristics, comorbidities, baseline renal function, and intraoperative and postoperative treatment measures, the AKI risk of patients in the highest NPR triplet (T3) was still 50% higher than that of the lowest group (T1) (OR=1.500). The robustness of this association suggested that the pathophysiological state represented by NPR, namely intense inflammatory storms accompanied by potential microcirculatory hypoperfusion, is independent of other traditional risk factors and directly involved in the pathogenesis of AKI.21 In addition, neutrophils directly cause kidney tissue damage by releasing reactive oxygen species, pro-inflammatory cytokines, and forming neutrophil extracellular traps (NETs).22,23 Thrombocytopenia may be related to sustained microvascular coagulation activation and platelet consumption after surgery, leading to a decrease in renal microcirculation blood flow.24 NPR integrates these two key aspects into a single indicator, which may be more comprehensive in reflecting the environment of AKI occurrence than any single indicator, which may be the reason for its independent predictive ability in multivariate models.
Through analysis of the onset time of AKI, we found a key feature: over 86% of cases occur within 72h after surgery. This highly concentrated time distribution strongly suggests that most postoperative AKIs are driven by direct injuries during the surgery itself and the perioperative process, such as renal ischemia–reperfusion caused by extracorporeal circulation and acute systemic inflammatory reactions induced by surgical trauma.19,25,26 This perfectly matches the characteristics of NPR as a rapidly obtainable inflammatory indicator in the early postoperative period. Our results indicate that NPR can effectively identify patients at risk of early kidney injury due to direct surgical impact, providing strong temporal logic support for its clinical application. In contrast, a small number of late-stage AKIs that occur 72h later may be more caused by postoperative secondary infections or delayed events such as drug nephrotoxicity.27,28 The predictive ability of NPR for this type of late AKI may be limited, which deserves further exploration in future research.
The results of this study are consistent with previous literature. Multiple studies have confirmed that an increase in neutrophil percentage is positively correlated with the risk and mortality of AKI after cardiac intervention,29 and thrombocytopenia is also an independent risk factor for AKI after apical aortic valve implantation30 and aortic dissection surgery.31 This phenomenon exists in both adult and pediatric patients.32 As a comprehensive indicator, the predictive value of NPR has been preliminarily confirmed in the field of heart disease, such as identifying short-term mortality risk (HR=2.37) in patients undergoing cardiac intervention therapy,33 and being associated with in-hospital adverse events (OR=1.602) and long-term adverse prognosis (HR=1.22) after cardiac surgery.34 Further research has shown that in critically ill COVID-19 patients, NPR has a better predictive ability for early AKI than other inflammatory markers.18 These pieces of evidence collectively support the potential of NPR as a comprehensive assessment tool for inflammation and coagulation/microcirculation status. This study provides the first systematic confirmation of the independent association between NPR and AKI in the cardiac surgery population, and further reveals its interaction with platelet transfusion, expanding the clinical applicability of this indicator.
This study found that platelet transfusion significantly enhanced the association between NPR and postoperative AKI risk (P for interaction=0.005). We believe that this phenomenon may stem from the cumulative effect of risk: preoperative high NPR values typically indicate significant inflammatory activation and potential microcirculatory disorders in patients, which constitute the initial high-risk background for AKI. On this basis, although platelet transfusion aims to correct coagulation function,35,36 the transfusion process itself may exacerbate systemic inflammation and renal microcirculation disorders by activating exogenous platelets, promoting their release of more inflammatory mediators and procoagulants.37–39 The combination of these two factors ultimately leads to a significant amplification of the risk of AKI occurrence.
The findings of this study have clear guiding significance for clinical practice. As an easily accessible perioperative inflammatory biomarker, the core value of NPR lies in its ability to identify high-risk patients for AKI after cardiac surgery at an early stage. Subgroup analysis indicates that platelet transfusion is a key factor affecting the association between NPR and AKI. In patients receiving platelet transfusions, the predictive effect of NPR on AKI risk is significantly enhanced, indicating that special attention should be paid to such patients. For high-risk populations identified by NPR, especially those who receive platelet transfusions during surgery, it is recommended to immediately initiate evidence-based AKI prevention bundling strategies. The prudent goal-directed hemodynamic management is required to optimize renal perfusion. Nephrotoxic drugs should be avoided, and special attention should be paid to strict perioperative blood glucose control since our research data also supports the correlation between blood glucose levels and AKI risk. It should be noted that this study has fully considered potential confounding factors such as sociodemographic variables in the statistical analysis. The results showed that even after controlling for these factors, the association between NPR and AKI remained significant and robust, indicating that its predictive value mainly stems from the perioperative inflammatory status it reflects and has independent clinical significance. In summary, by incorporating NPR into the preoperative and early postoperative risk assessment system, the precision of AKI prevention measures can be achieved, the allocation of medical resources can be optimized, and it is expected to improve the postoperative prognosis of cardiac surgery patients.
Our study has a number of drawbacks. First, since this study was a retrospective investigation conducted in a single tertiary medical center, our findings might not be as applicable to different populations or healthcare environments. Our findings will be validated by future multicenter prospective studies with larger sample populations. Second, although we have comprehensively adjusted for multiple known perioperative risk factors, the potential for unmeasured residual confounding factors remains. Notably, cardiopulmonary bypass time represents a critical unadjusted variable, as it is a well-established strong predictor of AKI following cardiac surgery. Furthermore, other potential details that may influence NPR values or renal outcomes, such as specific patient lifestyle factors and medication history (e.g., thrombopoietin, non-steroidal anti-inflammatory drugs), were not incorporated into the analysis due to data availability constraints. Third, considering the intricate connection between inflammation and AKI after cardiac surgery, research should explore additional inflammatory biomarkers and their relationship with AKI, assessing the predictive value of various biomarkers to identify those with greater sensitivity for risk assessment. Lastly, we focused solely on association between NPR and AKI risk within seven days post-surgery. Conducting prospective studies that follow patients and assess relationship between NPR and long-term renal recovery in AKI patients after cardiac surgery would also be important.
ConclusionOur study revealed that an increase in NPR is associated with an increased risk of AKI within 7 days after cardiac surgery. Subgroup analysis further reveals that the positive association between NPR and AKI risk is significantly enhanced in patients receiving platelet transfusions. As an easily accessible, comprehensive indicator of inflammation, NPR provides valuable clinical tools for early identification of AKI high-risk patients and implementation of targeted prevention strategies, which is of great significance for improving the prognosis of cardiac surgery patients.
Authors’ contributionsConceptualization: Mingwu Tian, Liqiang Yuan.
Data curation: Jianqiang Wu, Zheng Wang.
Formal analysis: Mingwu Tian, Liqiang Yuan.
Investigation: Zhi Wen, Jianqiang Wu.
Methodology: Zheng Wang, Jian Guo.
Project administration: Changxue Wu.
Resources: Changxue Wu.
Software: Jian Guo.
Supervision: Zheng Wang.
Validation: Zhi Wen.
Visualization: Changxue Wu.
Writing – original draft: Mingwu Tian, Liqiang Yuan, Zhi Wen.
Writing – review & editing: Jianqiang Wu, Zheng Wang, Jian Guo, Changxue Wu.
Ethics approval and consent to participateNot applicable.
FundingThis research was supported by Hospital Incubation Project, FHS202407.
Conflict of interestsThe authors declare that they have no competing interests.
Data availability statementData sharing not applicable to this article as no datasets were generated or analyzed during the current study.