Valvular calcification (VC) in chronic kidney disease is frequent, although most information derives from prevalent dialysis patients. There are few studies that analyse VC in patients who start dialysis.
ObjectiveTo analyse the presence of VC at the start of dialysis and its relationship with events and/or death from cardiovascular causes in the course of follow-up.
MethodsIn the study, we included patients who started dialysis between November 2003 and September 2007. In the first month of treatment, we assessed the presence of VC by Doppler echocardiography, along with demographic factors and risk factors for cardiovascular disease, coronary artery disease, stroke, atrial fibrillation (AF), and cardiac dimensional and functional electrocardiographic and echocardiographic parameters. The biochemistry values assessed were: haemoglobin, calcium/phosphorous/iPTH metabolism, cholesterol and fractions, triglycerides, troponin I, albumin, CRP and glycosylated haemoglobin. We analysed the association between VC and the presence of myocardial infarction (MI), stroke and/or death from cardiovascular causes up to transplantation, death or the end of the study (December 2012).
ResultsOf 256 enrolled patients (83% haemodialysis, 17% peritoneal dialysis), 128 (50%) had VC (mitral: 39, aortic: 20, both: 69). In the multivariate analysis, VC was associated with older age (OR: 1.110; 95% CI: 1.073–1.148; p = 0.000) and lower albumin levels (OR: 0.29; 95% CI: 0.14–0.61; p = 0.001). In a follow-up lasting 42.1 ± 30.2 months (898.1 patient-years), 68 patients suffered MI, stroke and/or died from cardiovascular causes. In the Cox regression analysis, older age (HR: 1.028; 95% CI: 1.002–1.055; p = 0.037), coronary artery disease and/or stroke (HR: 1.979; 95% CI: 1.111–3.527; p = 0.021), AF (HR: 2.474; 95% CI: 1.331–4.602; p = 0.004), and the presence of VC at the start of dialysis (HR: 1.996; 95% CI: 1.077–3.700; p = 0.028) were the predictor variables for the occurrence of the analysed events.
ConclusionsThe prevalence of VC at the start of dialysis is high and its presence predicts the occurrence of events and/or cardiovascular death in the course of follow-up.
La calcificación valvular (CV) en la enfermedad renal crónica es frecuente, aunque la mayor parte de la información procede de pacientes prevalentes en diálisis. Son pocos los estudios que analicen la CV en los pacientes que inician diálisis.
ObjetivoAnalizar la presencia de CV al inicio de diálisis y su relación con eventos y/o muerte cardiovascular en la evolución.
MétodosIncluimos en el estudio los pacientes incidentes en diálisis entre nov/03 y sept/07. En el 1° mes de tratamiento analizamos la presencia de CV mediante Ecocardiogramadoppler, junto a factores demográficos y de riesgo cardiovascular, enfermedad coronaria, accidente cerebrovascular (ACV), fibrilación auricular (FA) y parámetros de electro y ecocardiográficos dimensionales y funcionales cardiacos. Los valores bioquímicos analizados fueron: hemoglobina, metabolismo calcio/fósforo/iPTH, colesterol y fracciones, triglicéridos, troponina I, albúmina, PCR y hemoglobina glicosilada. Analizamos la asociación de la CV con la presentación de infarto de miocardio (IAM), ACV y/o muerte cardiovascular hasta el trasplante, muerte, o fin del estudio (dic/2012).
ResultadosDe 256 pacientes incluidos (83% hemodiálisis, 17% diálisis peritoneal), 128 (50%) presentaban CV (mitral: 39, aórtica: 20, ambas: 69). En el análisis multivariante la CV se asoció a mayor edad (OR: 1,110; IC 95%: 1,073-1,148; p = 0,000) y menor albúmina (OR: 0,29; IC 95%: 0,14-0,61; p = 0,001). En un seguimiento de 42,1 ± 30,2 meses (898,1 pacientesaño), 68 pacientes presentaron IAM, ACV y/o murieron por causa cardiovascular. En el análisis de regresión de Cox, la mayor edad (HR: 1,028; IC 95%: 1,002-1,055; p = 0,037), la enfermedad coronaria y/o ACV (HR: 1,979; IC95%: 1,111-3,527; p = 0,021), la FA (HR: 2,474; IC 95%: 1,331-4,602; p = 0,004) y la presencia de CV antes de entrar en diálisis (HR: 1,996; IC 95%: 1,077-3,700; p = 0,028), fueron predictores independientes de la presentación de los eventos analizados.
ConclusionesLa prevalencia de CV en el momento de iniciar diálisis es alta y su presencia predice la presentación de eventos y/o muerte cardiovascular en la evolución.
The presence of cardiac valvular calcifications (VC) in chronic kidney disease (CKD) is considered a frequent fact. Population studies have confirmed an association between CKD and mitral or aortic VC from initial stages of decreased glomerular filtration1,2. Nevertheless, most publications derive from studies of prevalent peritoneal dialysis and haemodialysis patients, in which the prevalence of VC is greater than 30% of patients3,4,5. In these studies, VC correlates with the time on replacement therapy, inflammation, malnutrition and atherosclerotic heart disease6,7,8,9,10. VC has been a predictor for mortality from cardiovascular causes and from any other cause3 in some studies, although not in all of them11.
VC and atherosclerosis are frequently observed in a same patient on dialysis, and the association between them has been demonstrated7,12. Based on this association, VC has been considered one of the manifestations of atherosclerosis7,13. However, all patients with VC do not have atherosclerosis. This suggests that, although both processes share pathogenic mechanisms, their pathogenesis and possibly the risk they involve are not identical14.
There are few studies about VC in patients with advanced stages of CKD at the onset of replacement therapy15,16.
The purpose of this study was to analyse the presence of VC in patients who started dialysis for the first time and its relationship with the occurrence of events and cardiovascular mortality during follow-up.
MethodsWe included patients diagnosed with stage 5 CKD, who started haemodialysis or peritoneal dialysis for the first time between November 2003 and September 2007 in our hospital centre. Patients who started treatment in another centre or had undergone prior renal transplantation were excluded. The observational period ranged from the first day of dialysis to termination due to transplantation, death, patient transfer outside our health area of influence, or the end of the study 31 December 2012.
In the first month of dialysis, the following variables were assessed and included for analysis: demographic characteristics; anthropometric measurements; pulse pressure; history of hypertension and/or antihypertensive treatment (HTN); diabetes with indication of drug treatment at any time of follow-up; active smoking habit or cessation in the last 10 years; coronary artery disease documented by a history of myocardial infarction (MI) or compatible coronary angiographic test; ischaemic or haemorrhagic stroke, documented by a neurologist and/or imaging test report; atrial fibrillation (AF) in any of its forms documented in a prior medical record or by an ECG finding; and, analytical variables, such as haemoglobin, mineral metabolism (calcium, phosphorous, PTH), urea, creatinine, troponin I, albumin, C-reactive protein (CRP), cholesterol and fractions, triglycerides and glycosylated haemoglobin.
VC was studied with colour Doppler echocardiography by a single observer. It was defined as increased echo-refringence with a thickness > 1mm at the level of the mitral or aortic annulus or leaflet. Three grades were established according to the calcification area: mild, when there were only small, isolated areas; moderate, when there were multiple areas; and severe, when calcification was extensive and diffuse. It was analysed whether the calcification was limited to only one valve, mitral or aortic, or involved both.
The endpoint of our study was the occurrence of one or several of the following events in the course of follow-up: MI, stroke or death from cardiovascular causes (defined as death due to heart failure), pulmonary thromboembolism, sudden death, mesenteric ischaemia or peripheral arterial ischaemia.
Statistical AnalysisThe Student's t-test or the nonparametric Mann-Whitney test was used for the comparison of means. For the comparison of qualitative variables, the Pearson's Chi-square test was used. For the analysis of the association between VC and the risk factors that were present at the start of treatment, a logistic regression multivariate analysis was performed, and the odds ratio (OR) and 95% confidence interval were obtained. The predictive power of variables for the occurrence of the endpoint of our study was analysed through a Cox proportional-hazard regression analysis. The prognostic variable was the occurrence of the endpoint defined in the Methods section. Predictive variables were the presence of VC, and other variables with significant association in the univariate analysis or of special significance. The hazard ratio (HR) and 95% confidence interval were obtained.
Event-free survival was analysed with the Kaplan-Meier method, and the Mantel-Haenszel test (log-rank) was used to compare survival curves. For hypothesis contrast tests, a value of p < 0.05 was considered statistically significant. The analyses were carried out with the statistical package SPSS 15.0 for Windows.
ResultsFollowing the exclusion criteria, 48 patients were not included; another 29 patients were not included since they could not participate in the entire initial study. The total number of enrolled patients was 256. Mean age was 65.1 ± 15.9 years, median age was 69.9, and 146 patients (57%) were male. Nephropathies induced by renal failure included the following: glomerulonephritis 17.2%; interstitial nephropathies 15.2%; nephrosclerosis 15.6%; polycystic kidney disease 6.3%; other familial diseases 1.2%; systemic diseases 5.1%; diabetes 18.4%; unidentified diseases 18.8%; other 2.3%. Diabetes caused nephropathy or was a concomitant disease in 73 (28.5%) patients.
They study included 213 (83%) patients receiving haemodialysis and 43 (17%) patients in peritoneal dialysis, with a mean age of 66.8 ± 14.8 and 56.5 ± 18.5 years, respectively (p = 0.004). Patients were monitored for 42.1 ± 30 months (range: 0.23–109.4), with a follow-up of 898.1 patient-years.
Prevalence of Valvular CalcificationAt the beginning of the dialysis programme, valvular calcification (VC) was present in 128 patients, which accounts for a prevalence of 50%. The grades were: 90 mild (35.1%); 30 moderate (11.7%); and 8 severe (3.1%). Calcification was present in the mitral valve in 39 (15.2%) patients, the aortic valve in 20 (7.8%), and in both valves in 69 (27%) patients.
Those patients who had valvular calcification were an average of 18 years older and were mostly women, diabetic patients, and had a history of cardiovascular events and diagnosis of atrial fibrillation. A higher proportion of patients included in the haemodialysis programme had valvular calcification. Creatinine, albumin and phosphorous levels were lower, while pulse pressure and body mass index were higher (Table 1). They also had greater left ventricular mass and left atrial dimension and greater diastolic dysfunction (Table 2). Frequency of HT and smoking habit, calcium levels, iPTH, anaemia or dyslipidemia, and systolic function assessed by echocardiography were not different from those observed in patients who did not have valvular calcification.
Characteristics of patients with VC at the start of dialysis.
| Without VC (n = 128) | With VC (n = 128) | p | |
|---|---|---|---|
| Age (years) | 56.2 ± 17 | 74 ± 9 | 0.000 |
| Sex: Female (%) | 47 (36.7) | 64 (50) | 0.032 |
| Technique: (Peritoneal | 30 (69.8) | 13 (10.2) | 0.004 |
| Dialysis) | |||
| Diabetes (%) | 26 (35.6) | 47 (64.4) | 0.004 |
| Coronary Artery Disease (%) | 6 (4.7) | 15 (11.7) | 0.040 |
| Ischaemic stroke (%) | 5 (3.9) | 14 (10.9) | 0.032 |
| AF (%) | 6 (4.7) | 25 (19.5) | 0.000 |
| BMI (kg/m2) | 26.7 ± 5.1 | 28.1 ± 5.2 | 0.043 |
| Systolic BP (mmHg) | 124.5 ± 22.4 | 133.6 ± 26.9 | 0.004 |
| Diastolic BP (mmHg) | 74.9 ± 12.9 | 71.2 ± 12.4 | 0.019 |
| Pulse pressure | 49.6 ± 18.7 | 62.4 ± 21.9 | 0.000 |
| Glucose (mg/dL) | 104.5 ± 39 | 121 ± 69 | 0.020 |
| Troponin I (ng/ml) | 0.03 ± 0.05 | 0.24 ± 1.07 | 0.030 |
| Creatinine (mg/dL) | 7.4 ± 2.3 | 5.9 ± 2.0 | 0.000 |
| Phosphorous (mg/dL) | 5.4 ± 1.8 | 4.8 ± 1.5 | 0.003 |
| Albumin (gr/dL) | 3.73 ± 0.51 | 3.38 ± 0.51 | 0.000 |
VC: Valvular Calcification; STR: Stroke; AF: Atrial Fibrillation
Echocardiographic parameters.
| Sin CV (n = 128) | Con CV (n = 128) | p | |
|---|---|---|---|
| LV mass/BS (gr/m2) | 156.2 ± 51.5 | 175.2 ± 52.3 | 0.005 |
| LVEF % | 65.5 ± 8.8 | 64.6 ± 6.9 | 0.460 |
| LA dimension (mm) | 39.55 ± 7.4 | 43.2 ± 7.5 | 0.000 |
| E/A ratio in mitral filling flow | 0.97 ± 0.45 | 0.79 ± 0.36 | 0.001 |
VC: Valvular Calcification; LV/BS: Left Ventricle/Body Surface; LVEF: Left Ventricular Ejection Fraction; LA: Left Atrium
In the multivariate logistic regression analysis, we included factors with statistical significance in the univariate analysis and other factors of potential involvement in the valvular calcification process: total cholesterol, HDL and LDL fractions, triglycerides, CRP, and left ventricular ejection fraction (LVEF). In this analysis, the factors independently related to the presence of VC were older age and lower albumin level (Table 3).
Occurrence of endpointDuring follow-up, 68 patients presented endpoint events of the study: MI, stroke, and/or death from cardiovascular causes. The distribution was as follows:
- •
Patients who died from cardiovascular causes: 50. Causes included: 8 MI; 7 stroke, of which 5 were haemorrhagic and 2 ischaemic, and 1 patient also had MI; 13 sudden death; 9 heart failure, cardiogenic shock or malignant arrhythmia; 8 mesenteric ischaemia; 2 pulmonary thromboembolism; 3 arterial ischaemia/lower limb amputation.
- •
Patients who had cardiovascular events: 18, of which 10 were MI, 7 were strokes, and 1 patient had MI and stroke. Twelve of these patients died in the follow-up due to non-cardiovascular causes, one received a renal transplant, and five were alive at the end of the study.
The 68 patients who experienced an endpoint event were older than the 188 patients who did not. Most were diabetic patients and patients with a history of AF, MI and/or stroke. In the echocardiographic test, they showed greater left ventricular mass and left atrial dilation with less left ventricular ejection fraction. Valvular calcification was more frequent in these patients (Table 4).
Patients who had the event (MI, stroke and/or death from cardiovascular causes).
| Patients with an event (n = 68) | Patients with no event (n = 188) | p | |
|---|---|---|---|
| Age (years) | 72,2 ± 9,8 | 62,5 ± 16,9 | 0.000 |
| Diabetes (%) | 41,2 | 23,9 | 0.007 |
| Prior coronary artery disease and/or stroke (%) | 30,9 | 9 | 0.000 |
| AF (%) | 17 (25) | 14 (7,4) | 0.000 |
| VC (%) | 51 (75) | 77 (41) | 0.000 |
| Creatinine (mg/dL) | 6,1 ± 1,8 | 6,9 ± 2,5 | 0.01 |
| Pulse Pressure | 60,5 ± 20,1 | 54,3 ± 21,5 | 0.034 |
| LV mass (g/m2) | 182,3 ± 61,4 | 159,5 ± 48 | 0.009 |
| LA (mm) | 43,4 ± 7,6 | 40,6 ± 7,5 | 0.011 |
| LVEF % | 61,9 ± 10,2 | 66,2 ± 8,6 | 0.001 |
AF: Atrial Fibrillation; VC: Valvular Calcification; LV: Left Ventricle; LA: Left Atrium; LVEF: Left Ventricular Ejection Fraction
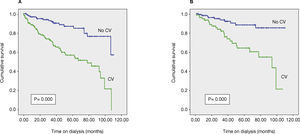
In the Kaplan-Meier analysis, the event-free survival was shorter in patients with valvular calcification. This difference was maintained when the analysis was performed in the 192 (75%) patients with no prior diagnosis of coronary artery disease, stroke or AF (Figure 1).
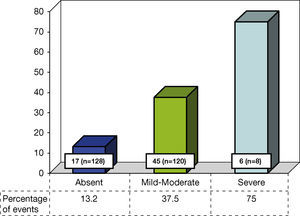
The occurrence of endpoint events increased according to the VC grade. In the absence of calcification, 13.2% of patients presented an event, 37% with mild or moderate grade and 75% of patients with severe grade (Figure 2).
In the Cox regression analysis, we included variables with statistical significance in the univariate analysis and others that were potentially associated with cardiovascular morbidity-mortality, such as sex, haemoglobin, phosphorous, CRP and dialysis technique. The factors independently associated with the occurrence of the endpoint of the study were the presence of VC at the start of dialysis, older age, and prior diagnoses of AF, coronary artery disease, and/or stroke (Table 5).
Predictive factors for event occurrence (MI, stroke and/or death from cardiovascular causes). Cox Regression Analysis.
| Hazard ratio | 95% CI | p | |
|---|---|---|---|
| Age | 1.028 | 1.002-1.055 | 0.037 |
| Valvular calcifications | 1.996 | 1.077-3.700 | 0.028 |
| Coronary artery disease and/ | 1.979 | 1.111-3.527 | 0.021 |
| or stroke | |||
| Atrial Fibrillation | 2.475 | 1.331-4.602 | 0.004 |
To assess whether VC severity increased the risk for endpoint events, the same analysis was performed for the calcification grades. For mild-moderate grade VC, the results were the following: HR 1.780 (95% CI 0.953–3.346, p = 0.07). Results for severe grade VC were: HR 4.517 (95% CI: 1.827– 11.809, p = 0.02).
DiscussionThe results of this study show that there is a high prevalence of VC in patients who start dialysis and that the presence of VC is associated with the occurrence of cardiovascular events and mortality in the course of follow-up. In the last decade, the scientific literature has shown that the frequency of VC (aortic, mitral, or both) in CKD is high. In the Framingham study, CKD (11% of patients with glomerular filtration rate < 40mL/min) increased the risk of mitral valve calcification by 60%, although not aortic calcification1. Another study did not find an association between glomerular filtration rate < 60mL/min and aortic valve calcification, but it did find an association with mitral valve calcification in diabetic patients only2. Most of the information about VC is from prevalent dialysis population studies, with a prevalence ranging from 30 to 70% of patients on both peritoneal dialysis2,3and haemodialysis4,5,11. However, studies of patients who initiate dialysis are less frequent. A recent published study of incident dialysis patients in Japan showed a VC prevalence of 57.7%, for an age slightly younger than that of our study15. In another publication, the prevalence of VC at the start of dialysis was 35.6% for patients 15 years younger than our patients16.
In our study, older age and lower levels of albumin (an inflammatory and malnutrition marker) were independently associated with the presence of VC. Age is an important factor associated with VC3,6, along with inflammatory markers. In prevalent dialysis patients, an association was demonstrated between VC and inflammatory markers, such as β2 microglobulin, cytokines, CRP and others like fetuin A5,8,9,15.
In the baseline assessment, patients with VC had a higher incidence of history of cardiovascular events, AF and diabetes, along with higher blood pressure and pulse pressure as well as structural alterations such as left ventricular hypertrophy and greater diastolic dysfunction. In studies of patients with VC on dialysis, cardiovascular disease and structural cardiac alterations have not always been assessed. In prevalent patients, VC has been associated with coronary artery disease10, a history of cardiovascular events and left ventricular hypertrophy11, and carotid intima-media thickness13. In the Japanese study of events during dialysis, cardiovascular events and structural cardiac alterations were not analysed15. In another study, patients with prior coronary artery events were excluded16.
VC was not associated with alterations in bone-mineral metabolism, which is similar to other studies of incident dialysis patients6,15; some studies of prevalent patients have shown an association between VC and some biochemical alterations in calcium/phosphorous metabolism17,18. A possible explanation is the better phosphorous control in incident patients with residual renal function, which does not exclude the involvement of bone-mineral metabolism alterations in the genesis of VC. The pathogenesis of VC and vascular calcification is not clear, although they share mechanisms; in patients on dialysis, a correlation between VC and vascular calcification has been shown19. CKD involves alterations in calcium/phosphorous metabolism and bone remodelling, inflammation and imbalance between inducers and inhibitors of calcification. The final result is the phenotypical change of cells in valvular and vascular structures to osteoblasts20,21. Both in experimental studies22 and clinical studies23, an inverse correlation has been shown between vascular and valvular calcification with the loss of bone mineralization, and, in patients on dialysis, it has been shown that the presence of VC is associated with a greater progression of coronary calcification, measured by multi-slice CT16. In the ADVANCE study, patients treated with the calcimimetic cinacalcet showed less increase in the progression of aortic valve calcification, which indicates the involvement of mineral metabolism disorders in VC24.
Another matter is the importance of VC as a predictive factor for cardiovascular risk in patients on dialysis. In studies of prevalent haemodialysis patients, VC was a predictor variable for all-cause mortality4. In prevalent peritoneal dialysis patients, it was a predictor for cardiovascular mortality and mortality from any cause; this is similar to the risk posed by the history of atherosclerotic events, which establishes it as a cardiovascular disease marker3. In other studies, VC was not a predictor of mortality in the multivariate analysis adjusted for age and inflammatory markers16 or adjusted for prior cardiovascular events11. A study of asymptomatic prevalent dialysis patients (69% haemodialysis) at high risk for cardiovascular disease, segmental alterations in myocardial contractility and LVEF < 40% demonstrated an association between VC and the presence of inducible myocardial ischaemia; this suggests that VC may be a marker for silent myocardial ischaemia risk in this population25.
In this study, VC was a predictor variable for the occurrence of MI, stroke and/or death from cardiovascular causes. There were more severe VC events than mild-moderate events (Figure 2). In the multivariate analysis adjusted for all the included variables, the mild-moderate grade was observed at the limit of statistical significance as a predictor variable for endpoint events.
The availability of simple tools is important to assess cardiovascular risk. In studies conducted in our institution, the history of cardiovascular events recorded in medical records, data from exploratory tests and electrocardiograms were useful to predict cardiovascular risk in our population on dialysis26–29. Echocardiography is a safe, low-cost, widely available technique and a simple tool that adds value to the results of this study.
In summary, at the start of a dialysis programme, a high proportion of patients have VC. This fact doubles the risk of MI, stroke and/or death from cardiovascular causes during the course of dialysis. The magnitude of this risk is similar to that of cardiovascular disease or the presence of AF before the start of dialysis.