Despite the increasing prevalence of end-stage renal disease, peritoneal dialysis (PD) is still offered to a minor subset of patients. One way to increment the utilization rates of this technique is the early start of PD after catheter placement, but there are several concerns related to this approach.
MethodsRetrospective analysis in a single-center; 52 patients, 34.6% of the patients started in the first 14 days after catheter placement (Urgent start Group – Group 1) and percentage started PD in a conventional mode (Non-urgent start Group – Group 2). Baseline data, short-term (90-day) clinical outcomes, mechanical complications and infectious episodes were compared among Groups.
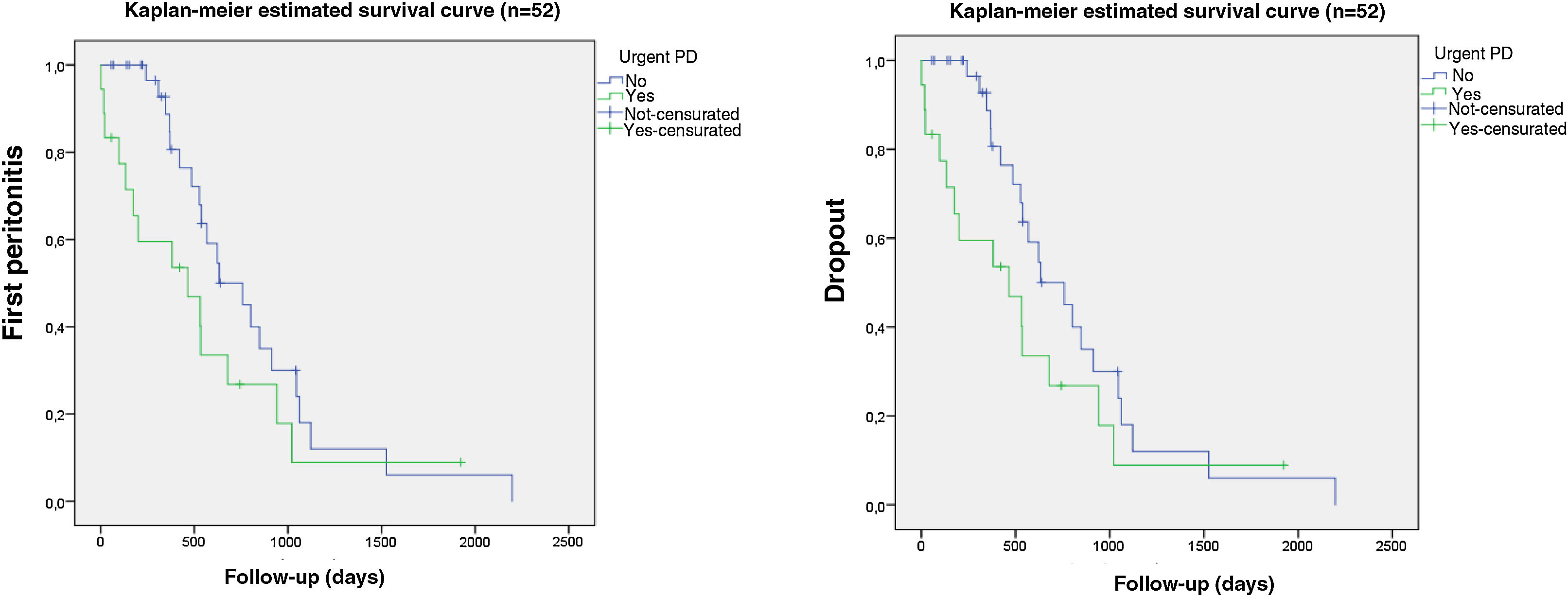
ResultsAt baseline, Group 1 had an higher Charlson Comobidity Index (CCI). Exchange volumes were significantly lower in Group 1, as expected. Short-term outcomes were equal except for iPTH and albumin, both lower in urgent-start Group (p<0.05). Episodes of leak, catheter dysfunction and rate of infections were similar among Groups (p>0.05). In Urgent-start Group we didn’t observed a higher risk for the first peritonitis episode (HR 0.68; 95% CI 0.24–1.99; p>0.05), higher dropout rate or risk to quit the technique (long rank test, p>0.05; HR 0.57; 95% CI 0.29–1.13; p>0.05).
ConclusionAccording to our observations, urgent-start PD seems to be a valid and safe alternative to urgent hemodialysis with central venous catheter and should be offered to patients without major contraindications.
A pesar de la creciente prevalencia de la enfermedad renal terminal, la diálisis peritoneal (DP) sigue ofreciéndose a un reducido subconjunto de pacientes. Una forma de incrementar las tasas de utilización de esta técnica es el inicio temprano de la DP después de la colocación del catéter, pero existen varias dudas respecto a esta estrategia.
MétodosAnálisis retrospectivo en un único centro; 52 pacientes; en el 34,6% de los pacientes se inició en los 14 primeros días tras la colocación del catéter (grupo de inicio urgente [grupo 1]) y el resto comenzó la DP de forma convencional (grupo de inicio no urgente [grupo 2]). Se compararon los datos iniciales, los resultados clínicos a corto plazo (90 días), las complicaciones mecánicas y los episodios infecciosos entre los grupos.
ResultadosAl inicio del estudio, el grupo 1 tenía un índice de comorbilidad de Charlson (ICC) más alto. Los volúmenes de intercambio fueron significativamente menores en el grupo 1, como se esperaba. Los resultados a corto plazo fueron iguales, excepto para la hormona paratiroidea intacta (HPTi) y la albúmina, ambas inferiores en el grupo de inicio urgente (p<0,05). Los episodios de fuga y de disfunción del catéter, así como la tasa de infecciones, fueron similares entre los grupos (p>0,05). En el grupo de inicio urgente no se observó un mayor riesgo de sufrir el primer episodio de peritonitis (CRI: 0,68; IC del 95%: 0,24-1,99; p>0,05), ni una mayor tasa de abandono o riesgo de abandonar la técnica (prueba del orden logarítmico, p>0,05; CRI:0,57; IC del 95%: 0,29-1,13; p>0,05).
ConclusiónSegún nuestras observaciones, la DP de inicio urgente parece ser una alternativa válida y segura a la hemodiálisis urgente con catéter venoso central, y debería ofrecerse a los pacientes sin contraindicaciones importantes.
Among the renal replacement therapies (RRT), in the vast majority of industrialized countries, Peritoneal Dialysis (PD) is still underused. Compared to countries as Mexico or Taiwan, PD use in the United States of America is restricted to only 7% of patients with End-Stage Renal Disease (ESRD).1 According to the registry of the Portuguese Society of Nephrology, during the year 2018, only 8.7% of patients started PD; when considering patients treated by dialysis or with a functioning renal transplant in the same period, the numbers are even lower, about 3.8%.2 The reasons of PD underuse are well identified and are either patient or caregiver centered. Reimbursement policies favoring HD in most healthcare systems and the restraint to perform PD in private facilities are also important obstacles to the widespread of this modality. Despite the efforts made by countries as Portugal to promote the expansion of PD programs, like pre-dialysis education care, about 35% of patient who reach ESRD do not have any definite plan for this stage of the disease.1 This subset of patients poses a specific problem: the concern with the urgent access placement and initial PD prescription seem to justify the choice of HD through a central venous catheter as the first option, even though most of them would be considered suitable for PD.1,3–6 The purpose of our study was to demonstrate that the urgent PD start, defined as the use of catheter in the next 14 days of its placement to perform the technique, could be a safe option in patients without a dialysis plan or without the possibility to use a central venous catheter, due to central vein thrombosis or stenosis.
MethodsIn our study, we enrolled patients who started PD between October 2012 and March 2018 in a medium sized Nephrology Department in Portugal. Patients were divided in two Groups concerning the mode of starting PD: Urgent-Start PD (Group 1) and Non-urgent Start (Group 2). As stated before, urgent start PD refers to those patients without a dialysis plan care at the time of the beginning of technique, who choose PD as RRT modality and who start dialysis in the first 14 days after catheter implantation.
For each patient, we evaluated baseline demographic data, Charlson comorbidity index (CCI), etiology of ESRD, previous nephrology follow-up and mode of catheter placement (surgical or percutaneous). Early clinical outcomes (weekly Kt/V, daily ultrafiltration, hemoglobin, iron saturation, intact parathyroid hormone, phosphorus, calcium, and albumin) were evaluated 90 days after the beginning of PD program, as well as the prevalence of infectious [peritonitis, exit-site infections (ESI)] and mechanical complications (leaks, catheter malfunction). Patient and technique survival and causes for PD dropout were also evaluated. Baseline demographic data, short-term (90-day) clinical outcomes, infectious and mechanical complications, dropout causes were compared between Groups. p values were determined by using Chi-square test for comparing proportions and t-Student test for comparing means. A p<0.05 was considered statistically significant. Time to adverse events was examined with standard survival analysis methods, including Kaplan–Meier models and Cox regressions for multivariate analyses. Relative risk (with a 95% confidence interval) and hazard ratio (HR) were calculated.
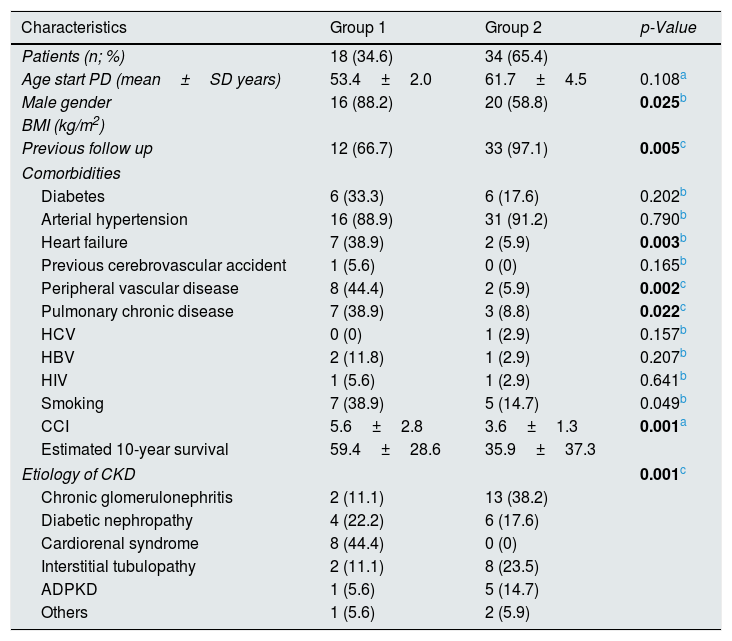
ResultsA total of 52 patients were included in the study, 34.6% (Número de doentes) in Group 1 and 65.4% (Número de doentes) in Group 2. We observed male predominance in Group 1, but no statistical differences in age or body mass index. Group 1 also presented a higher prevalence of chronic pulmonary obstructive and cardiovascular diseases (but not diabetes) and higher CCI, with an estimated 10-year mortality of 59.4%. As expected, patients on Group 2 had more frequently a previous Nephrology follow-up. ESRD etiology was also correlated with urgent start of PD, with 44.4% of the patients in Group 1 beginning dialysis because of cardiorenal syndrome. Patients’ characteristics are summarized in Table 1. Percutaneous technique was the main form of catheter implantation in both Groups. The average time until catheter use was, in Group 1, 4.94±1.21days, with 38.9% inducing dialysis in the first 24h due to severe uremic symptoms and/or volume overload. No significant difference was reported in the first PD prescription between Groups, except for the lower dwell volumes in the urgent start patients. Biochemical and hematological parameters related to CKD complications (anemia, mineral bone disease and nutrition), either at baseline or 90 days after technique beginning were similar among Groups, with the exception of the parathyroid hormone and albumin levels (lower in Group 1 (p<0.05) in both moments. Adequacy parameters (weekly KtV, creatinine clearance and ultrafiltration volume) were also evaluated 90 days after beginning and the results were similar (p>0.05). Despite of the higher rates of leak (18.8 vs 8.8%) and catheter dysfunction (33.3 vs 24.2%) in Group 1, the risk was not statistically higher (p>0.05). Regarding infectious complications, 29 episodes of exit-site infection (ESI) and 33 of peritonitis were recorded, mainly due to Staphylococcus aureus (31.0%) and Staphylococcus epidermis (13.8%); however its occurrence was also similar between the Groups (p>0.05). Despite of the earlier occurrence of first peritonitis in Group 1 (478 vs 831 days), this time difference was not statistically significant (p>0.05) and, according to the Kaplan–Meier analysis, these patients did not have worse free-time to first peritonitis episode(long rank test, p>0.05, Fig. 1A). In multivariate Cox regression model, Group 2 was associated with 32% reduction in risk of first peritonitis episode compared with Group 1 (HR 0.68; 95% CI 0.24–1.99; p=0.487). Regarding to technique survival, Group 2 presented a lower rate (61.8% versus 77.1%), and a reduction in dropout risk of 43%; however this difference was not statistically significant (HR 0.57; 95% CI 0.29–1.13; p 0.105).
Baseline characteristics of the patients included in the present study.
| Characteristics | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| Patients (n; %) | 18 (34.6) | 34 (65.4) | |
| Age start PD (mean±SD years) | 53.4±2.0 | 61.7±4.5 | 0.108a |
| Male gender | 16 (88.2) | 20 (58.8) | 0.025b |
| BMI (kg/m2) | |||
| Previous follow up | 12 (66.7) | 33 (97.1) | 0.005c |
| Comorbidities | |||
| Diabetes | 6 (33.3) | 6 (17.6) | 0.202b |
| Arterial hypertension | 16 (88.9) | 31 (91.2) | 0.790b |
| Heart failure | 7 (38.9) | 2 (5.9) | 0.003b |
| Previous cerebrovascular accident | 1 (5.6) | 0 (0) | 0.165b |
| Peripheral vascular disease | 8 (44.4) | 2 (5.9) | 0.002c |
| Pulmonary chronic disease | 7 (38.9) | 3 (8.8) | 0.022c |
| HCV | 0 (0) | 1 (2.9) | 0.157b |
| HBV | 2 (11.8) | 1 (2.9) | 0.207b |
| HIV | 1 (5.6) | 1 (2.9) | 0.641b |
| Smoking | 7 (38.9) | 5 (14.7) | 0.049b |
| CCI | 5.6±2.8 | 3.6±1.3 | 0.001a |
| Estimated 10-year survival | 59.4±28.6 | 35.9±37.3 | |
| Etiology of CKD | 0.001c | ||
| Chronic glomerulonephritis | 2 (11.1) | 13 (38.2) | |
| Diabetic nephropathy | 4 (22.2) | 6 (17.6) | |
| Cardiorenal syndrome | 8 (44.4) | 0 (0) | |
| Interstitial tubulopathy | 2 (11.1) | 8 (23.5) | |
| ADPKD | 1 (5.6) | 5 (14.7) | |
| Others | 1 (5.6) | 2 (5.9) | |
ADPKD, autossomal dominant polycystic kidney disease; CCI, Charlson comorbidity index; cm- centimeters; kg, kilograms; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; SD, standard deviation.
For a long time, the concerns related with mechanical and infectious complications have justified the non-use of PD as the first option to patients that need urgent RRT but the question that remain is: are those risks truly higher when compared to conventional dialysis outcomes? The advantages of a period around 2–4 weeks between the catheter placement and the initiation of PD are well known and are mainly related to allow proper peritoneal healing.7–11 Unfortunately, in some cases, patient survival depends on urgent initiation of dialysis and a subset of patients seldom presents with unstable clinical features that also affects dialysis (HD and DP) and patient's outcomes. In our study, urgent start patients were more likely to be referred late, which implied PD initiation often without hemodynamic stabilization and/or under uremic syndrome. Despite the clinical condition, no statistical difference was observed in PD modality or catheter placement, being the modified Seldinger technique the main option due the shorter time admission and smaller complexity of the procedure.12 Biochemical laboratorial values were similar in both groups, with the exception of serum albumin and intact parathyroid hormone levels, probably related to the lack of adequate follow-up and worse overall clinical condition. Regardless higher initial exchange volumes in the conventional group, this difference had no impact on the adequacy parameters, including daily UF. As expected, mechanical complications occurred earlier in Group 1, but the prevalence and risk were comparable. These adverse effects could easily be minimized with measures as laparoscopic catheter insertion, purse-string suture, PD in supine position as well as the use of smaller exchange volumes, which explain the lower volumes prescribed in Group 1.7,9,13,14 It is also well known that infections are also an important cause of lower efficacy and technique survival. In our cohort, despite the occurrence of earlier events in the urgent-start Group, there was no significant difference in the incidence between both groups. It is important to properly monitor and educate these patients, who do not have a timely placed peritoneal access, to minimize the difference in the risk of infectious complications compard to patients with a standard pre-dialysis educational care. We must not forget that several factors that are not directly related to the early start of the technique (age, CCI or cardiovascular comorbidities, acute illness with the need of hospital admission) may have an important impact on morbidity/mortality and influence the outcomes in all the modalities of urgent dialysis, PD and HD.14–20
Our study has its limitations: it is a single-center non-randomized study with a relatively small sample size, with no control Group, which makes it difficult to interpreted and generalize our results to other centers. However, we described a very diverse population that represents the reality of ESRD patients; that is why we find that these results may be able to confirm the safety and the positive outcomes of urgent PD in patients with severe conditions, that require immediate dialysis, mainly the ones who traditionally would start urgent HD with a temporary central venous catheter.
ConclusionUrgent-start PD could be a safe alternative to HD with a temporary central venous catheter, with similar technique survival to conventional-start PD patients. Despite of the apparently higher risk of complications, the equivalent rates of early and late infectious, as well as the marginally higher rates of mechanical complications, should not discourage the use in patients who do not have major contraindications to PD. In fact, the rates of infectious and mechanical complications associated to HD transcutaneous vascular access (like bacteremia, central venous stenosis or vascular thrombosis) are responsible for the lower longevity and success of the technique, as well as, for the higher morbidity and mortality. For all those reasons, urgent-start PD seems to be valid alternative in patients requiring urgent RRT.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNo conflict of interest.