Starting hemodialysis (HD) through an indwelling catheter (IDC) increases the risk of bacteremia, a risk that increases if it is maintained as a prevalent venous access (VA), and it is directly related to the morbimortality of the patient on HD.1,2 To reduce its incidence, clinical guidelines1,3,4 suggest a series of control measures, unified diagnostic criteria and common reference points. Thus, they define catheter-related bacteremia and establish as a control index the number of events per 1000 days of catheter use, and consider a rate of less than 1/1000 catheter days an excellent result.
The main route of entry for germs in an intravascular device with cuff is the intraluminal route5 and the most effective measure to control germs is aseptic management of the IDC,6 using different antimicrobial seals7 in case of high catheter-related bacteremia rates, but may not prevent associated complications. In 2015 we founded our unit and designed a protocol8 for aseptic IDC management implemented with the use of the Twister® Reverse Flow Device (TWR).9 This is a system designed to measure the flow of fistulas, but in catheters it allows us to reverse the flow ahead of monitor alarms without disconnecting the blood lines, which maintains the integrity of the connection, reducing the exposure of blood and/or connection systems to air or friction with non-sterile areas and therefore the risk of pathogens reaching the blood.
We conducted a 6-year retrospective review (2015–2021) of incident patients in HD carrying IDC, obtaining a total of 143 patients and 35 cases of catheter-related bacteremia that meet the diagnostic criteria defined by guidelines.1–3 The health district includes one hospital center and 2 centers under contract, so we compared the protocols for aseptic handling of the IDC, common to both contracted centers, and established the existing differences: use of TWR in hospital, a larger sterile drape in the hospital setting and higher nurse/patient ratio in the contracted center (4:1 vs. 5:1). We obtained and analyzed clinical histories from the JARA project, including age, sex, days on hemodialysis, days on incremental dialysis, days in the center, type of venous access, Charlson index, catheter days, clinical history and data on hospitalization for catheter-related bacteremia.
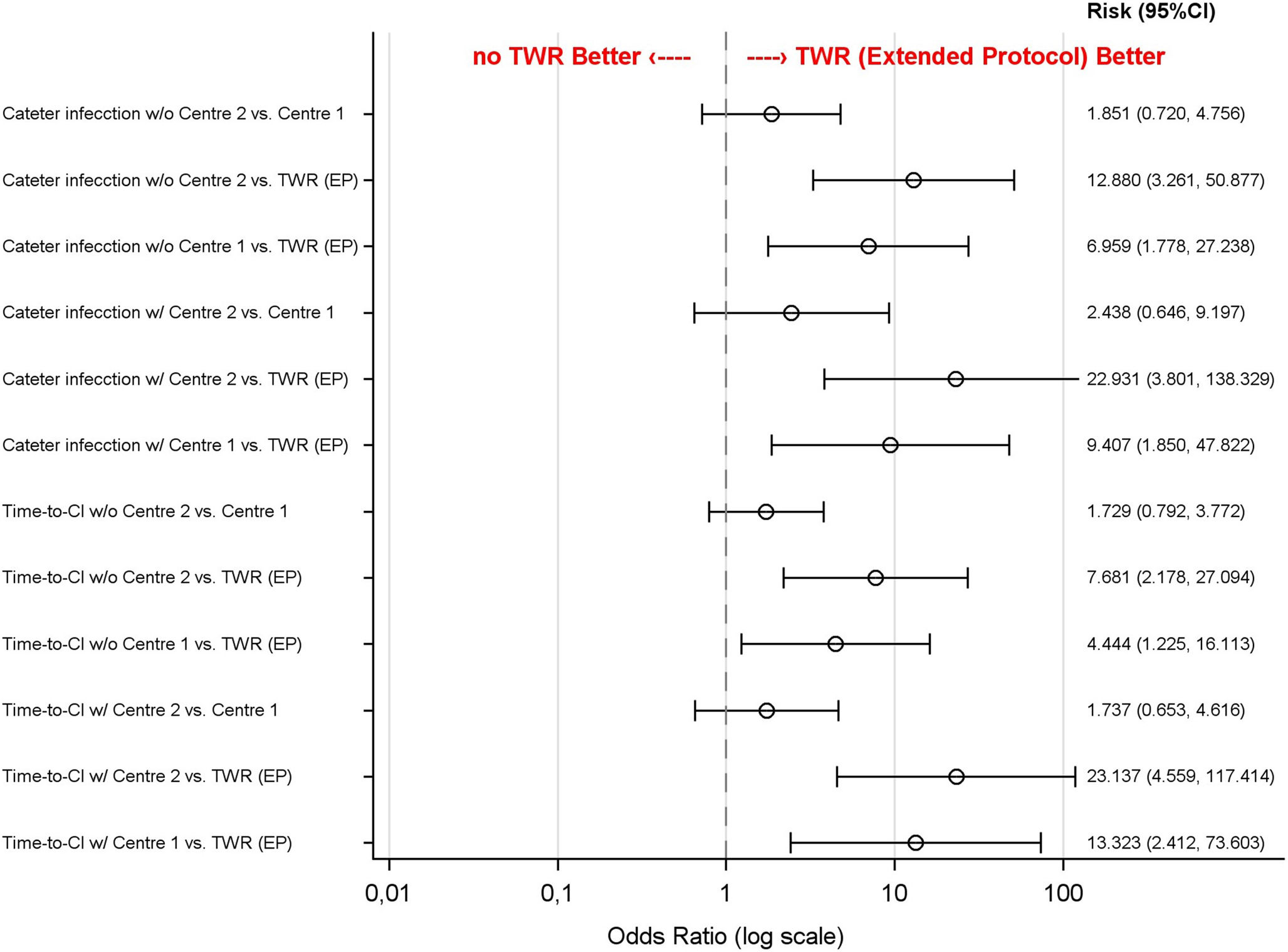
Of the 143 included patients, 63 received therapy at the Hospital Virgen del Puerto, 40 at hemodialysis center 1 and 40 at hemodialysis center 2. Of the total catheter-related bacteremia cases, 3 took place in the hospital unit and 32 in the peripheral units, which means a catheter-related bacteremia rate of 0.17 versus 0.83 per 1000 catheter days in favor of the TWR protocol. The statistical analysis revealed a significant difference (p < 0.001) in terms of the need for hospitalization and days of admission for catheter-related bacteremia (normalized to 1000 catheter days) with results favoring the TWR protocol (0.04 vs. 0.33 and 0.23 vs. 3.40 days of admission/1000 days of IDC). In the linear regression, adjusted for the covariates analyzed (Fig. 1), we observed that the TWR protocol is a protective factor against catheter-related bacteremia. Furthermore, it is more effective in delaying catheter-related bacteremia while maintaining the IDC free of infection for longer, differences that are not found in the regression when comparing both centers that do not use the TWR (Fig. 2).
Linear regression analysis. Effect of TWR on the presence of catheter-related bacteremia and catheter infection-free time.
w/o: without covariates; w/: with covariates; TWR (EP): TWR (extended protocol); Time-to-CI: time to catheter infection. Risk of binary event as catheter infection is shown with the odds ratio and confidence interval risk of time to event as time-to-catheter infection is shown with the hazard ratio and confidence interval.
In 2022 the Spanish Ministry of Health published the estimated cost of bacteremia episodes at 7186.2; with an average admission of 10.2 days which means a daily cost of 697.7;.10 If applied to the calculated days of admission, the average cost per catheter-related bacteremia per 1000 catheter days is 821.09 ; vs. 5,992.08 ;, in favor of the use of TWR. But we must also add the cost/session for the application of TWR; 10.30 ;/session, i.e. an expense of 4063.56 ;/1000 days in the hospital center and zero in the contracted centers. Therefore, the total cost to be compared would be the sum of applying TWR and the average cost derived from admission by catheter-related bacteremia, final cost 4,884.6 ; vs. 5,992.08 ; in favor of TWR. We calculated a lower cost per infection, which represents a final difference of 19.5% in favor of the TWR protocol.
In conclusion, the use of TWR systems appears to be a useful and cost-effective tool for reducing and delaying episodes of catheter-related bacteremia in our units while awaiting a definitive arteriovenous fistula. Despite the weaknesses of the study, the non-randomization and inter-individual variability in the application of the protocol, we found that there is no significant difference in the rate of catheter-related bacteremia among centers that do not use TWR. It is necessary to design studies to increase the evidence base for this type of data.