Tramadol is recommended for treatment of moderate pain in patients with kidney disease1 and is regarded as a safe analgesic for patients with chronic kidney disease (CKD) since it lacks any direct nephrotoxic effects unlike the non-steroidal anti-inflammatory drugs (NSAID). However rare instance of acute kidney injury (AKI) due to granulomatous interstitial nephritis induced by tramadol has been reported.2 We report a case of AKI in a 30 years old man resulting from concomitant intake of tramadol and ondansetron which provoked serotonin syndrome, rhabdomyolysis and myoglobinuria.
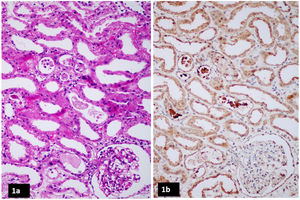
A 30 years old man was rushed to the emergency room after he had an episode of brief convulsion at his home. He was apparently healthy prior to this event and had no morbidities like diabetes mellitus or hypertension. However, he had chronic low back ache and insomnia for which he had ingested a combination of tramadol (50mg, thrice a day) and ondansetron (4mg twice a day) during the preceding 7 days. On admission to the hospital, he was irritable, disoriented and febrile (temperature 100°F). His pulse was 110/min, BP – 168/108mm Hg, respiratory rate was 22/min and his oxygen saturation while breathing ambient air was 97%. He had repeated episodes of generalized clonic jerks which occurred either spontaneously or were provoked by noise (startle). Pupils were normal in size and reacted to light normally. There was no focal neurological weakness; however, there was generalized muscular rigidity. Tendon reflexes were exaggerated and he had bilateral ankle clonus. Rest of the clinical examination was unremarkable. Computed tomography scan of brain was normal. The clinical course and lab reports are summarized in Table 1. After admission to the hospital, his urine output progressively declined and serum creatinine increased to 6.5mg/dl which necessitated initiation of hemodialysis. Serum creatinine phosphokinase (CPK) surged to 62500Unit/liter. Urine appeared dark brown and dipstick tested positive (3+) for blood while there were few RBCs in urine sediment. Kidney biopsy revealed acute tubular injury with intratubular cats which stained positive for myoglobin in immunohistochemistry (Fig. 1). There was no interstitial eosinophilic infiltration or granulomas. A diagnosis of serotonin syndrome induced by the combination of tramadol and ondansetron was made and patient was managed with cessation of offending drugs, hydration, benzodiazepine chlordiazepoxide, temporary dialysis and supportive care with which his sensorium improved and clonic jerks ceased. AKI was managed with intermittent hemodialysis with high flux membrane. He required three sessions of hemodialysis following which kidney function started to improve. He was dialysis independent by the ninth day of illness, discharged from the hospital on the twelfth day of illness when his serum creatinine was 2.1mg/dl. He eventually recovered completely from AKI.
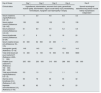
Clinical course and lab reports.
| Day of illness | Day 1 | Day 2 | Day 3 | Day 4 | Day 9 |
|---|---|---|---|---|---|
| Clinical status | Hyperthermia, disorientation, recurrent clonic jerks, generalized muscle rigidity, disorientation, oliguric acute kidney injury necessitating hemodialysis, myoglobin cast nephropathy in biopsy | Normal neurological statusRecovery phase of acute kidney injuryDialysis independent | |||
| Serum creatinine (mg/dl)(Reference: 0.6–1.2) | 1.1 | 2.0 | 4.6 | 6.5 | 3.2 |
| Serum sodium (mmol/L)(Reference: 135–145) | 138 | 130 | 132 | 131 | 139 |
| Serum potassium (mmol/L)(Reference: 3.5–5.0) | 6.1 | 6.9 | 5.5 | 5.2 | 4.8 |
| Serum bicarbonate (mmol/L)(Reference: 22–26) | 17 | 8 | 12 | 18 | 20 |
| Serum creatine kinase (U/L)(Reference: 55–170) | 33000 | 62500 | 40300 | a | 210 |
| Hemoglobin (gm/dl)(Reference: 13–16) | 14.6 | 14.0 | 13.8 | 13.8 | 14.0 |
| Total white blood cell count (cells/mm3)(Reference: 4000–11000) | 12400 | 14100 | 16500 | 13800 | 6800 |
| Platelet count (cells/mm3)(Reference: 150000–350000) | 205000 | 230000 | 310000 | 289000 | 186000 |
| Total serum bilirubin (mg/dl)(Reference: 0.5–1.0) | 0.9 | 1.0 | 1.0 | 1.1 | 1.0 |
| Alanine amino transferase (U/L)(Reference: 0–40) | 56 | 78 | 65 | 55 | 32 |
| Aspartate aminotransferase (U/L)(Reference: 0–40) | 65 | 82 | 76 | 43 | 25 |
Serotonin syndrome results from a heightened serotonin activity in the central and peripheral nervous system predominantly in the 5HT1A and 5HT2A receptors.3 Drugs which interfere with the metabolism and reuptake of serotonin increase the level of serotonin in the nervous system, thereby inducing the toxidrome. The list of drugs that could cause serotonin syndrome is exhaustive, however common agents include tramadol, meperidine, fentanyl, dextromethorphan, metoclopramide, ondansetron, granisetron, monoamine oxidase inhibitors like linezolid, serotonin reuptake inbitors like fluoxetine etc.4 Although any one drug on its own could provoke serotonin syndrome, a combination of two or more drugs has a greater propensity to induce the toxidrome. Our patient consumed a combination of tramadol and ondansetron which synergistically induced serotonin syndrome. Serotonin syndrome is characterized by a constellation of mental status changes (like agitation, anxiety, disorientation, excitement) autonomic dysfunction (like hyperthermia, tachycardia, tachypnea, arrhythmias) and neuromuscular abnormalities (like tremors, clonus, hyperreflexia and muscle rigidity).4 Neuroleptic malignant syndrome and malignant hyperthermia are close differentials for this toxidrome.
The diagnosis of serotonin syndrome is made clinically and relies upon the Hunter Serotonin Toxicity Criteria (HSTC).4 The HSTC requires consumption of a serotoninergic drug with at least one out of the following five requirements being met: (1) spontaneous clonus, (2)inducible clonus with agitation or diaphoresis, (3) ocular clonus with agitation or diaphoresis, (4) tremor and hyperreflexia, (5) hypertonia, hyperthermia>100.4°F and ocular or inducible clonus. This patient had altered mental status, hyperthermia, tachycardia, rigidity, spontaneous and inducible clonus in the background of ingestion of serotoninergic drugs viz. tramadol and ondansetron thereby satisfying the HSTC for serotonin syndrome. Repeated clonus and muscular rigidity culminated in rhabdomyolysis, myoglobinuria and AKI in this patient. Extreme form of serotonin syndrome is known to result in AKI by inducing rhabdomyolysis. Tramadol overdose producing seizure, high creatine kinase and AKI was reported by Afshari et al.5
Tramadol exerts its analgesic effect by two mechanisms – firstly by acting at the opioid receptor and secondly by preventing noradrenaline and serotonin reuptake in the nervous system.6 Thus, tramadol has a propensity to increase serotonin action in the nervous system and induce serotonin syndrome either when prescribed alone at high doses or in combination with other serotoninergic drugs. This potential of tramadol to induce serotonin syndrome and cause severe AKI either when used alone or in combination with other serotoninergic drugs must be kept in mind while prescribing the drug.
Previous presentation of this work as a whole or partNone.
Funding informationNone to disclose.
Conflict of interestNone.
We thank Dr. Anila Abraham, M.D., Consultant Pathologist, Renopath Lab, Chennai, India for providing renal histopathology images.