In Nephrology, the use and integration of ultrasound as a diagnostic tool has been included in the activity of the speciality since the 1980s–1990s, mainly applied to the assessment of the urinary system and the evaluation of vascular access for dialysis.1–3
The scope of ultrasound in the speciality of Nephrology expanded rapidly, both as a diagnostic tool and in the performance of procedures. However, the acquisition of these competencies requires basic and advanced training models, suitably structured in centres with extensive experience and recognised for this purpose and, although it is already included in the training programme of the speciality, there is still a long way to go.4
Although it is already included in the training programme for the speciality, there is still a long way to go in the accreditation of centres and training programmes that allow students and teachers to be assessed and certified in the use of ultrasound. The aim of this article is to establish the basis for the creation of curricular programmes within the speciality of nephrology that include Point-of-care Ultrasonography (PoCUS) as a useful diagnostic tool.
PoCUS in Nephrology: an unmet medical needPoCUS is defined as a focused ultrasound scan performed by any physician at the patient's bedside, allowing immediate and correct clinical integration.5 Currently, PoCUS emerges as a useful tool for any nephrologist, with the aim of achieving an adequate correlation with the anamnesis and physical examination, using ultrasound as a tool to phenotype congestion (tissue and vascular), together with echocardioscopy (also known as FoCUS, from focused cardiac ultrasound).6,7 The ability of these parameters to perform dynamic scanning in decongestive therapy has potential implications for the treatment and understanding of the pathophysiology of congestive nephropathy, which remains an underdiagnosed entity at present.8–10
Today, the wide availability and relatively low cost of portable and ultra-portable ultrasound devices allow virtually any physician to perform PoCUS. Features such as artificial intelligence-assisted image acquisition and expert remote guidance further facilitate the spread of this new tool. In fact, PoCUS (insonation) has evolved to become the fifth pillar of the conventional physical exam11 helping to answer specific clinical questions such as "does this patient have a pericardial effusion", "is there congestion" and, if so, "is the congestion tissue, vascular or mixed". Some of the features of PoCUS are summarised in Table 1. However, the usefulness of PoCUS depends on proper image acquisition, accurate interpretation and clinical integration of the findings obtained.
Some characteristics of PoCUS.
| If you have oedema you clearly have congestion, there is no need for PoCUS. | False: Although the presence of oedema is a sign of tissue congestion, it does not indicate the presence of vascular congestion, which is useful in personalising treatment. |
| PoCUS NEVER replaces the assessment by Cardiology or Radiology. | True: PoCUS responds to specific questions at the patient's bedside, it is not intended to replace the regulated assessment by other specialties, which is complementary. |
| PoCUS is very easy, no formal training is required. | False: Ultrasound by its nature is operator dependent. An example is the assessment of vascular congestion where there are multiple limitations related to the patient, the ultrasound equipment and the operator. Regular training will allow correct identification and correlation of ultrasound findings with clinical data of the patient. |
| PoCUS can be carried out with ultra- portable or portable equipment. | True: The goal of PoCUS is to bring ultrasound to the patient's bedside, so easy-to-carry equipment is ideal. In addition, some manufacturers allow the use of artificial intelligence to better interpret the images or indicate the position of the transducer for better imaging and assessment. |
PoCUS: point-of-care ultrasonography.
Therefore, it is essential that physicians performing PoCUS receive adequate training to avoid unintended harm to patients due to misdiagnosis. The integration of PoCUS into the various levels of medical training is the key to ensuring standardised and uniform training. Evidence suggests that brief PoCUS training at the bedside improves the clinical diagnosis of medical students and young physicians compared to conventional physical examination alone. For example, after a 2-h training on echocardiography, Panoulas et al. reported that the use of PoCUS by medical students and residents substantially increased the sensitivity and specificity for the detection of left ventricular systolic dysfunction compared to physical examination (74.1% vs. 25.9% and 93.6% vs. 84.9%, respectively).12 Similarly, in another study, two half-day training sessions led by nephrologists increased the confidence of internal medicine residents in identifying common renal parenchymal abnormalities.13 However, long-term skill retention is only possible with well-structured longitudinal study programmes, as opposed to introductory courses.14 In contrast to short introductory courses where practical training takes place in simulation models or on healthy volunteers, long-term retention of skills is only possible with well-structured longitudinal study programmes. In real life, several patient- and equipment-related factors influence or limit image acquisition and clinical integration, leading to erroneous clinical decisions, especially by inexperienced users.15
Until a large number of well-trained nephrologists is reached, standardisation of PoCUS training will only be possible if professional societies collaborate and develop appropriate certification programmes for residents and nephrologists.
Interesting examples would be the work carried out by the Spanish Society of Neurology (SEN), in collaboration and consensus with the Spanish Society of Cardiology (SEC), and the Spanish societies of Internal Medicine (SEMI) and Family and Community Medicine (semFYC) for the education, formaltraining and application of echocardioscopy in patients with cardiovascular pathology, such as the etiological study of stroke, among others.16 or the consensus document on ultrasound training published by the working group on Intensive Care Ultrasound of the Spanish Society of Anaesthesiology and Resuscitation (SEDAR), the Spanish Society of Internal Medicine (SEMI) and the Spanish Society of Emergency Medicine (SEMES) serve as an example for other specialties, such as Nephrology, which are new to incorporating this tool.17,18
Experience of the clinical ultrasound working group of the Spanish Society of Anaesthesia and Resuscitation (Sociedad Española de Anestesia y Reanimación)SEDAR formed in 2017 an ultrasound working group initially consisting of 11 anaesthesiologists. The criteria for membership of the working group were (1) formal accreditation in echocardiography by a scientific society with an established competency programme: European Association of Cardiovascular Imaging (EACVI/ EACTA) or National Board of Echocardiography (NBE) in the USA or Focused Intensive Care Echo (FICE) in the UK; (2) current involvement in education, teaching Intensive Care Echocardiography (ICCE) courses in the UK; and (3) specialists who routinely use echocardiography in their clinical practice. All of them had knowledge of echocardiography, most of them started their training in cardiology departments, completed a training stay and routinely used this diagnostic tool in intensive care units, i.e., "echocardiography enthusiasts".
The main objective of this group was to develop a Spanish consensus document on ultrasound techniques, classified as basic and advanced, used in the care of critically ill patients. The evidence and opinions published in international consensus documents from other scientific societies were used for this purpose. The areas of inclusion were echocardiography, pulmonary, vascular and abdominal ultrasound. In order to obtain additional qualification for the correct execution of a project of this magnitude, some members were included in training programmes led by radiology and vascular surgery.
Another objective was to consolidate a working group to provide practical training courses for both residents and specialists in critical care or emergency areas (anaesthesiologists, intensivists, emergency physicians, family physicians, nephrologists, internists).
To establish consensus, there were 2 rounds of voting by members, followed by a face-to-face meeting of the expert panel for consensus building if more than 50% of the votes were obtained for each point, delineating the competencies of image acquisition and the pathways for obtaining the diploma of accreditation in the use of basic echocardiography in Intensive Care and Emergency Medicine.18
The examples of other societies presented here could be useful as a reference for the generation of a consensus in education and training regarding the use of PoCUS in our speciality. These documents were produced with the collaboration of societies from different specialties and set methodological objectives and the minimum number of procedures required to obtain an endorsed training that could be included in the residency period.
Steps towards a consensus on the use of PoCUS in NephrologyIn 2014, the board of the Spanish Society of Nephrology (S.E.N.) approved the creation of the Diagnostic and Interventional Nephrology Group (NDI). The aim of this group, since its inception, has been to expand and disseminate this discipline, bringing together Spanish nephrologists with experience and interest in this area, grouping together various diagnostic and invasive procedures, with ultrasound as the cornerstone of this activity and including bedside ultrasound (PoCUS). The NDI group has carried out several initiatives, such as the assessment of the situation of diagnostic and interventional nephrology in the different nephrology departments in Spain through an extensive survey, the implementation of several specific courses, and the development of a series of training programmes.19 The group has carried out multiple specific courses, including a Master's Degree in NDI and formally published the first consensus document for ultrasound training in the speciality of Nephrology in 2020.20 This document emphasised the usefulness of multi-organ ultrasound including assessment of renal parenchymal alterations, arteriovenous fistula, procedural guidance for central venous catheter placement and volume assessment, mentioning also the introduction of echocardioscopy. This document includes a description of both basic and advanced techniques and highlights the official inclusion of the use of ultrasound in the Nephrology training programme, as well as the current development of the new speciality plan, in which the NDI group has actively participated and in which specific relevance will be given to diagnostic and interventional procedures, most of which are carried out with ultrasound. The NDI group of the S.E.N. is currently preparing a catalogue of NDI centres. Is drawing up a catalogue of teaching centres in the different variants of NDI, with a view to laying the foundations for the teaching accreditation process of the different services and areas involved.
PoCUS, understood as the early and agile performance of ultrasound diagnosis, often with ultra-portable or portable equipment, is part of the field of activity of NDI, and is currently in full expansion. Nephrologists' interest in PoCUS was stimulated by the publication of the Venous Excess Ultrasound Grading System (VExUS) by Beaubien-Souligny et al.21 a method to quantify systemic venous congestion by Doppler ultrasound. Since this study, several subsequent publications, in particular by nephrologists, have demonstrated its usefulness in multiple clinical contexts, such as hyponatraemia, cardiorenal syndrome, hepato-renal syndrome and patients on renal replacement therapy.7,10,22–27 Nephrologists consider ourselves experts in the management of complex fluid and electrolyte disorders and the ability to perform multi-organ PoCUS allows us to improve the diagnostic process at the bedside and provide better patient care, and therefore, we must also be experts in this discipline.
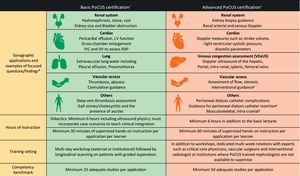
The growing popularity of PoCUS in nephrology and the increasing pressure on educational institutions to rapidly incorporate this skill into residency training has drawbacks due to the shortage of trained professionals, infrastructure, length of residency and lack of universally accepted clinical practice curricular elements. Current training programmes are heterogeneous without rigorous quality control. Like any other clinical skill, knowledge acquired in short courses decays in a short time without continued practice; therefore, ideally, longitudinal curricula should be developed that cover the entire length of a nephrology residency. New training programmes should build on existing curriculum models such as the Nephrology Partnership programme14 such as the Nephrology Partnership for Advancing Technology in Healthcare (NPATH) programme, which is a project led by the University of Bari that within the Erasmus + programme of the European Commission has created an international project comprising 8 reference centres in interventional nephrology, 2 reference societies, the European Renal Association (ERA) and the Vascular Access Society (VAS), a simulation company and an e-learning company, as well as online platforms such as Nephrology+, the Erasmus + programme of the European Commission, the European Renal Association (ERA) and the Vascular Access Society (VAS), a simulation company and an e-learning company.28 and online platforms such as NephroPOCUS.com, recognised by the American Society of Nephrology. These have a high didactic content and allow the development of a competency/quality assessment process at institutional level. In 2021, some of the authors founded the International Alliance for PoCUS in Nephrology (IAPN) with the aim of transforming physical examination in Nephrology through PoCUS through international and multidisciplinary collaboration. It is therefore essential that professional societies such as the S.E.N., through the specific groups of PoCUS in Nephrology. Through specific dedicated working groups, such as the NDI group, continue to advance this type of initiative and work to define the scope of competencies and develop standardized guidelines for the use of PoCUS in Nephrology, as well as official education and training to enable its formal expansion within the speciality. Fig. 1 includes our proposed curricular organisation model.
Proposed framework for standardized point of care ultrasound (PoCUS) certification in Nephrology. Sonographic applications are divided into basic and advanced depending on the complexity of image acquisition and interpretation.
LV, left ventricle; IVC, inferior vena cava; IJV, internal jugular vein; RAP, right atrial pressure; VExUS, venous excess ultrasound.
*Examples are not exhaustive.
#Optional applications depending on the local practice patterns.
+Both basic and advanced training require an evaluation of theoretical and practical knowledge.
The authors declare that they have not received funding for this article.
Conflict of interestThe authors declare that they have no conflict of interest.