To assess SV in our RRT population in the period 1976–2012 as well as the influence of technique transference (TT).
Materials and methodsThe study included a retrospective cohort of 993 patients. Data were classified as transplant (Tx), change in technique, exitus or lost to follow-up. SV for TT was determined in patients with over 12 weeks of permanence.
ResultsThe mortality risk adjusted for age, sex, dialysis technique or diabetes mellitus (DM) showed that the estimated risk of death increased by 4.8% per year increase (HR=1.048; 95% CI: 1.04–1.06; p<.001) and was 44% higher in diabetics compared to non-diabetics (HR=1.44; 95% CI 1.16–1.76; p<.01). Regarding SV for TT, patients who initiated HD had a shorter survival than those who initiated PD and transferred to HD (p=.00563).
ConclusionIn our experience, SV in RRT is dependent on age and coexistence of DM. It would be beneficial to reinstate the concept of “comprehensive care”, in which RRT would start with PD and later transfer to HD.
La supervivencia (SV) comparada en terapia renal sustitutiva (TRS) es dependiente de la comorbilidad previa al inicio de TRS y no de la técnica dialítica.
ObjetivoValorar la SV en nuestra población de TRS habida en el periodo 1976–2012 y asimismo la influencia por la transferencia de técnica (TTc).
Material y métodosCohorte retrospectiva (n=993 pacientes). Los datos fueron “censurados” por trasplante (TX), cambio de técnica, defunción o pérdida para el seguimiento. La SV por TTc se realizó en pacientes con más de 12 semanas de permanencia.
ResultadosEl riesgo de mortalidad ajustado por edad, sexo, técnica dialítica o diabetes mellitus (DM) mostró que el riesgo estimado de morir aumenta un 4,8% por cada año aumentado (HR=1048, IC del 95%, 1,04–1,06, p<0,001) y este aumenta un 44% en los diabéticos con respecto a los no diabéticos (HR=1,44, IC del 95%, 1,16–1,76, p<0,01). En cuanto a la SV por TTc, los que inician HD presentan SV menor que los que inician DP y son transferidos a HD (p=0,00563).
ConclusiónEn nuestra experiencia, la SV en TRS es dependiente de la edad y la coexistencia de DM y sería conveniente retomar el concepto de “cuidados integrales” comenzado la TRS por DP y transferir a HD.
The survival of uraemic patients on haemodialysis (HD) and peritoneal dialysis (PD) was compared in several trials over recent years, resulting in extended controversy and dissimilar outcomes.1 The reasons accounting for this variability are complex, but are basically associated with the use of different study designs including non-homogeneous populations, different types of follow-up, the analysis of incident vs. prevalent population, and comorbidities prior to renal replacement therapy (RRT).1
A number of studies have shown that pre-RRT comorbidities are the most important factors predicting survival.2,3 Therefore, the dialysis modality may not have an independent effect on survival; furthermore, studies should be conducted on the incident patients.4
Since the beginning of the century it was suggested that both types of replacement therapy should be considered complementary for the “integral care” of the patient, an approach that may improve the survival in RRT.5 This is based on the idea that RRT should be started with PD and then switched to HD in case of complications or “lack of efficiency” of the technique.6,7
Based on these premises, our aim is to assess survival in both, HD vs. PD as well as survival resulting from the switch from PD to HD in patients from a retrospective cohort of 36-year of data collection.
Materials and methodsThe study includes a retrospective cohort of patients receiving RRT in our centre between 1976 and 2012. This registry includes data on demographics (age, sex, background disease) change of replacement therapy, transplants, deaths, or change of address. The original population were 1231 patients; but 223 were excluded because of incomplete data ondemographics; the final study sample was 993 patients.
Statistics: Gaussian variables and non-Gaussian variables will be presented as mean±SD and as medians, respectively. Variables were tested for normality using the Kolmogorov–Smirnov and Shapiro–Wilk tests. Qualitative variables will be expressed as frequencies and percentages.
Data were “censored” for transplants, loss or change of technique, or death.
The survival analysis by dialysis modality was performed from day 0 and was stratified by age, with the sample median as the cut-off value: 65 years of age, sex, and presence or absence of diabetes mellitus (DM).
Overall survival was estimated in the cohort and in strata defined by Kaplan–Meier. The relative risks of mortality for PD vs. HD were assessed by using a Cox regression analysis. Technique transference was analysed using Kaplan–Meier in patients who had completed over 12 weeks.
Differences were considered statistically significant at a p<0.05 in all analyses. Analyses were made by using the R free software (http://www.r-project.org).
ResultsA total of 993 patients were included in the cohort (Table 1). Elderly patients tended to be started with HD (p=0.0374) and the incidence of DM was higher in PD patients (p=0.000).
Descriptive analysis of the cohort and outcome.
| N | % | |
|---|---|---|
| Men | 634 | 63.85 |
| Women | 359 | 36.15 |
| No diabetes mellitus | 794 | 80.77 |
| Diabetes mellitus | 189 | 19.23 |
| HD | 685 | 68.98 |
| PD | 308 | 31.02 |
| HD (n=685) | PD (n=308) | p Value | |
|---|---|---|---|
| Age (M±SD) | 60.97±16.23 | 58.8±16.74 | 0.0374 |
| Gender (male) | 446 (65.11%) | 188 (61.04%) | 0.2168 |
| Diabetes (yes) | 99 (14.6%) | 90 (29.51%) | 0.0000 |
| Outcome | |||||
|---|---|---|---|---|---|
| HD, n=685 | PD, n=308 | ||||
| Death | 357 | 52.12% | Death | 131 | 42.53% |
| HD | 89 | 12.99% | PD | 29 | 9.42% |
| Tx | 188 | 27.44% | Tx | 83 | 26.95% |
| Switch to PD | 31 | 4.53% | Switch to HD | 60 | 19.48% |
| LFU | 20 | 2.92% | LFU | 5 | 1.62% |
HD, haemodialysis; LFU, lost to follow-up; PD, peritoneal dialysis; Tx, treatment.
The reason to cease the data collection were: a change in techniques: 91 (9.16%); death: 488 (49.14%); transplant: 271 (27.29%); loss to follow-up: 25 (2.52%); and continued PD: 29 (2.92%) and HD: 89 (8.96%).
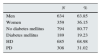
Survival was lower in patients who started with PD p<0.05 (Fig. 1a). Median survival time was 1815 days (4.97 years) in HD and 1255 days (3.44 years) in PD. Cumulative mortality was 52.12% in the HD group and 42.53% in the PD group (p<0.01).
The survival in consecutive incidents patients in HD (n=548) vs. PD (n=244) in less than 6 months favoured PD (p=0.0091) (Fig. 1b). The median survival time in patients starting HD and PD were was 138 days and 173 respectively. The cumulative mortality in HD patients was 55.95% and 31.67% in PD patients (p<0.01).
No differences in survival were found in patients followed for less than a year (HD, n=452 and PD, n=195) (p=0.1277), 5 years (HD, n=149 and PD, n=29) (p=0.4287), or 10 years (p=0.1057).
When corrected by age, the overall survival was slightly lower in the PD group. No difference in survival was found among patients older than 65 years (p=0.068). Median survival in HD and PD was 1340 days (3.67 years) and 926 days (2.53 years), respectively. Cumulative mortality in HD and PD was 69.04% and 70.23%, respectively (p=0.8034). No differences were observed in patients who were 65 years of age or younger (p=0.2249), although cumulative mortality was 37.02 in HD and 22.03 in PD (p<0.001).
In relation to gender, survival is higher for incident males in HD as compared to males starting on PD (p=0.0064). Median survival in HD was 1741 days (4.77 years) and 1112 days in PD (3.04 years), while cumulative mortality in HD was 50.9% and 43.62% in men from the PD group (p=0.0939). No significant differences were observed among women with the two types of treatment (p=0.5249); however the cumulative mortality was 54.39% and 40.83% in HD and PD patients, respectively (p<0.05).
Overall survival was superior in non-diabetic vs. diabetic patients (p<0.001). Median survival in HD was 1910 days (5.23 years) and 1465 days (4 years) in PD. Cumulative mortality was 50.09% in HD and 36.74% in PD (p<0.001). No significant differences were observed among incident diabetic patients based on dialysis technique (p=0.3606). Median time on HD was 1161 days (3.19 years) and 1000 days (2.74 years) in PD. Cumulative mortality in the HD and PD groups were 65.66% and 56.67% (p=0.2049) respectively. No differences were found in non-diabetic patients in HD vs. PD (p=0.1489).
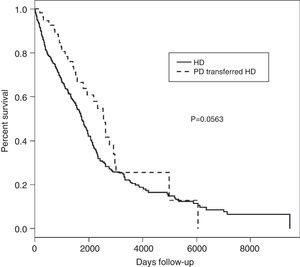
The mortality risk adjusted for age, gender, technique, and diabetes (Table 2) shows a 4.8% yearly increase in the estimated risk of death (HR=1.048, 95% CI, 1.04–1.06, p<0.001) and there is 44% increase in diabetic vs. non-diabetic patients (HR=1.44, 95% CI, 1.16–1.76, p<0.01). The analysis of the impact of changing technique (PD to HD) was conducted in 654 subjects who started with HD (who were not transferred) and 57 subjects who had started with PD and later there were switched to HD. Survival rates of incident patients in HD and PD who were switched to HD are shown in Fig. 2.
Patients starting on HD have a lower survival rate than patients who initiated PD and then switched to HD (p=0.0563). The median survival time of patients starting with HD was 1742 days (4.77 years) and 2566 days (7.02 years) in patients starting with PD who switched to HD.
Cumulative mortality was 54.59% in HD patients and 50.85% (r=0.5808, p>0.05) in PD patients who were switched to HD.
The analysis of survival in incident patients who were followed for at least 5 years between HD and PD who were switched was not significant (p=0.1767), and neither was the cumulative mortality (p=0.7096>0.05). However, significant differences were observed in patients followed for 10, 15, and 20 years.
Patients starting with HD had a worse 10-year survival (p<0.01) as compared to patients starting with PD who were switched to HD. The median survival time in HD was 1621 days (4.44 years) and 2533 days (6.93 years) in patients starting with PD who were later switched to HD.
Cumulative mortality in HD patients was 303/506 (53.53%) and 28/55 (50.91%) (p=0.7096) in patients who started with PD and switched to HD.
The 15-year survival is also worse in HD patients compared to patients who started with PD and switched to HD (p<0.05). The median survival time in patients starting with HD was 1714 days (4.69 years) and 2566 days (7.02 years) in patients who started with PD and switched to HD. Cumulative mortality in HD patients was 314/587 (53.49%) and 19/56 (51.79%) in patients who started with PD and switched to HD (p=0.8068).
Significant differences were still present at 20 years (p<0.005). The median survival in patients starting on HD was 1727 days (4.73 years) and 2566 days (7.02 years) in patients who started with PD and were switched to HD. Cumulative mortality in the HD group was 320/595 (53.78%) and 30/57 (52.63%) in patients who started with PD and were switched to HD (p=0.8679).
DiscussionAs a result of the methods used, survival studies on RRT posed major challenges, complications, and diverse interpretations. As first explained in the Ross et al. meta-analysis,3 the most important factor having an effect on survival is previous history of comorbidities, while dialysis technique has no independent and differentiated effect. Under these circumstances, the strategy of the statistical analysis should have a major effect in the final outcome. By means of a refined description, Perez Fontan et al.2 address problems arising in this type of analysis, essentially including: statistical methods used, and external and internal validity of studies. In our case, just as in any other study, the statistical methods used1 were the univariate analysis of actuarial survival and Kaplan–Meier, and the Cox multivariate analysis. Even though the latter has certain limitations, including assumed linearity (the effect of RRT may not be consistent over time) and the consideration of a single terminal event. As far as limitations resulting from internal validity, cardiovascular and non-cardiovascular comorbidity of patients is not available, and of course, allocation of treatment modality is not at random. A comparison of the baseline characteristics of the sample (Table 1) revealed that the PD population was younger (p=0.03749) and the prevalence of DM was higher (p=0.0000), and our results are consistent with other studies,2,4,8,9 where survival is influenced by age and DM, and this effect is sustained following the adjustment for comorbidities.2
Survival was higher in PD that HD at 6 months, just as in other observations,4 but no significant differences were seen at 5 and 10 years, as described.9–11 This outcome is certainly influenced by technical improvements both in PD and HD, early remission in patients in the end-stage chronic renal disease (ESCRD) consultation and free choice of therapy.1,8,9
The change from PD to HD results in a higher survival rate5 and in our case survival was higher in PD patients who were transferred to HD as compared to those who remained in HD, thereby strengthening the notion of “integrated care” in RRT. RRT should be started with PD and then switched to HD once completed or in case of loss of residual renal function.5–7
The study had two basic limitations. The first limitation is that it is a retrospective and that the patient allocation is not at random, and the second limitation is that no data were collected on comorbidity, except for age and concurrent DM, or variables including dialysis dosing, HD or PD modality, residual renal function or arteriovenous fistula or catheter. Nonetheless, an analysis of a database including information from a 32-year follow-up proves that survival in RRT is higher when patients start with PD and are later switched to HD, and that mortality risk is 2.6-fold higher in patients older than 65 years and is increased by 50% in patients with diabetes mellitus.
Conflicts of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Otero González A, Iglesias Forneiro A, Camba Caride MJ, Pérez Melón C, Borrajo Prol MP, Novoa Fernández E, et al. Supervivencia en hemodiálisis vs. diálisis peritoneal y por transferencia de técnica. Experiencia en Ourense 1976–2012. Nefrología. 2015;35:562–566.