Chronic kidney disease (CKD) is a growing health problem affecting between 10% and 15% of the Spanish population. The lack of updated projections of the evolution of the disease burden hinders the development of evidence-based health policies and interventions to optimise the management of the disease and prevent its progression. The aim of this study is to project the evolution of the clinical and economic burden of CKD in Spain between 2022 and 2027.
Materials and methodsInside CKD uses a validated microsimulation approach to project the burden of CKD. The projection is based on a virtual population according to Spanish demographics, literature, national data registries and clinical expert opinion. Costs associated with CKD management, renal replacement therapy (RRT), cardiovascular complications and arterial comorbidities were included.
ResultsIn Spain, an absolute increase in the prevalence of CKD of 1% (from 10.7% to 11.7%) is expected between 2022 and 2027, corresponding to an increase from 5.14 million to 5.68 million patients in 2027. However, only one third of CKD patients would be diagnosed. Of these diagnosed patients, 3.9% will require RRT in 2027, an increase of 14.7% from 2022. A total of 654,281 accumulated deaths are expected in patients with CKD diagnosed between 2022 and 2027. The economic burden of diagnosed CKD is expected to increase by 13.8% to 4.89 billion euros in 2027, representing 5.56% of total Spanish public health expenditure in 2027 (compared to 4.88% in 2022), of which 42.5% will be allocated to RRT (2.4% of public health expenditure).
ConclusionsThe Inside CKD project highlights the growing clinical, economic and social burden of CKD in Spain expected by 2027. Progression to more advanced stages with the need for RRT and associated complications represent a small proportion of the total CKD population, but contribute significantly to overall costs.
La enfermedad renal crónica (ERC) es un problema de salud creciente que afecta entre el 10–15% de la población española. La escasez de proyecciones actualizadas sobre la evolución de la carga de enfermedad obstaculiza el desarrollo de políticas e intervenciones sanitarias basadas en la evidencia para optimizar el manejo de la enfermedad y prevenir su progresión. El objetivo de este estudio es proyectar la evolución de la carga clínica y económica de la ERC en España entre 2022 y 2027.
Materiales y métodosInside CKD utiliza un enfoque de microsimulación validado para analizar la carga proyectada de la ERC, a partir de una población hipotética según la demografía española, bibliografía, registros de datos nacionales y opinión de expertos clínicos. Los costes incluidos fueron asociados a la gestión de la ERC, el tratamiento renal sustitutivo (TRS), las complicaciones cardiovasculares y las comorbilidades arteriales.
ResultadosEn España, se prevé un incremento absoluto en la prevalencia de ERC del 1% (del 10,7% a 11,7%) entre 2022 y 2027, equivalente a un aumento de 5,14 a 5,68 millones de pacientes en 2027, de los cuales solo un tercio serían diagnosticados. Se prevé un total de 654.281 muertes acumuladas en pacientes con ERC diagnosticada entre 2022 y 2027. El 3,9% de los pacientes diagnosticados requerirán TRS en 2027, un incremento del 14,7% respecto a 2022. La carga económica de la ERC diagnosticada se prevé que aumente un 13,8%, hasta los 4.890 millones de euros en 2027, lo que representaría un 5,56% del gasto sanitario público español total en 2027 (frente a 4,88% en 2022), de los cuales el 42,5% se destinará a TRS (2,4% del gasto sanitario público).
ConclusionesEl proyecto Inside CKD demuestra la creciente carga clínica, económica y social de la ERC en España prevista para el 2027. La progresión a los estadios más avanzados con necesidad de TRS y las complicaciones asociadas representan una pequeña parte de la población total con ERC, pero contribuyen de forma significativa a los costes totales.
Chronic kidney disease (CKD) is one of the world's biggest public health problems and is estimated to affect 10–15% of the population in Spain.1,2 CKD is defined as the presence of abnormalities in kidney structure or function for at least three months, with implications for the patient's health.3 The main risk factors for CKD include advanced age,3 genetic predisposition4 and pre-existing comorbidities, such as diabetes mellitus, particularly type 2 (T2DM), obesity5,6 and arterial hypertension.7
In the early stages of the disease, subjects are often asymptomatic, which can lead to the silent progression of kidney damage and worse long-term health outcomes.8,9 The progression of CKD is associated with an increasing clinical burden and cardiovascular (CV) complications, such as cerebrovascular accident (CVA), myocardial infarction (MI) and heart failure (HF),10 which impact the quality of life of subjects and increase the all-cause mortality rate.11 In late-stage CKD, patients initiate renal replacement therapy (RRT), which further increases the overall burden of the disease and profoundly affects quality of life.12 The main types of RRT available are haemodialysis (HD), peritoneal dialysis (PD) and kidney transplant. Despite RRT, life expectancy may be shortened by up to 40 years compared to the population of the same age not dependent on RRT.13,14
CKD is associated with a high economic burden related to significant consumption of healthcare resources, especially in the more advanced stages due to the need for RRT. In 2016, it was estimated that subjects on RRT (approximately 57,000 people, representing only 0.1% of the Spanish population) consumed between 2% and 5% of the health budget in Spain.15 The high cost associated with CKD is due to complex factors, such as the diversity of its aetiology, accelerated biological ageing, increased comorbidities and the treatment. This intersectionality means that anticipating the resulting economic burden requires careful assumptions and interpretations.16
The evidence would seem to indicate that proactive interventions, such as screening17,18 and early treatment,19 can slow disease progression and decrease the clinical and economic burden, including the need for RRT. However, the scarcity of data on the prevalence and burden of CKD limits the knowledge and optimisation of management strategies, undermining opportunities for timely diagnosis and treatment.
Currently, evidence on global and national future projections of CKD prevalence and its clinical and economic impact is scant, owing to the scope of factors to be considered and the extensiveness of the research. Microsimulation modelling may provide an alternative approach, using different data sets to project the trajectory of the disease20 and allowing the creation of virtual, heterogeneous populations through which to model clinical outcomes. Quantifying the clinical and economic burden aims to generate evidence and knowledge that will enable policy makers to understand the situation and optimise CKD management strategies.
The aim of the Inside CKD programme is to analyse the prevalence and project the global burden of CKD by age, G (stage) category, comorbidity and complications in 31 countries, including Spain.21 The aim of this paper is to describe the clinical and economic burden of CKD in Spain between 2022 and 2027, as estimated in the Inside CKD study, to help health authorities establish preventive strategies focussed on reducing the future associated burden.
MethodsOverviewThe detailed methodology of the Inside CKD projection has been published already.21 This study presents the data used to characterise the model and the projection of the results of the analysis in Spain between 2022 and 2027. The model used by Inside CKD leverages demographic, epidemiological, clinical and economic data to project the burden of CKD onto a simulated virtual population generated from these data to describe the local situation and impact of the disease in 31 regions around the world.
Data enteredA virtual population of 20 million individuals representative of the Spanish population was generated, using local demographic data, published literature and expert clinical opinion. The sources of information for the different parameters included in the Spanish model along with a brief description are available in Appendix A additional material (Table S1).
For Spain, local demographic parameters were used to assign a profile to each virtual individual based on the following four modules: 1) population, which includes demographic data such as age, sex and comorbidities associated with CKD (T2DM and hypertension)22; 2) CKD stage (G1-G5) and use of RRT, assigned to each individual using the 2009 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) group equation,23 which considers the estimated glomerular filtration rate (eGFR) from serum creatinine without correction for race and albuminuria (category A1-A3) according to the albumin/creatinine ratio, obtained from regional databases and published literature1,2,24; 3) disease burden, which includes the prevalence of comorbidities (T2DM and hypertension), relative incidence of CV complications (CVA, MI and HF) and the probability of death from any cause25–33; and 4) health economics, which includes the costs associated with CKD diagnosed in categories G3a-G5, the costs of RRT (HD, PD and transplant incidence and maintenance) and the costs associated with CV complications.26,34–39
For those parameters in which local literature was not available, data from countries with similar environments and populations were used. Specifically, the proportion of subjects according to eGFR and albuminuria categories by age and sex was estimated from the data provided by Otero González et al.1 and Gorostidi et al.,2 respectively. However, as the data in the Spanish literature are aggregated, an algorithm was applied to fit them, by age groups required in the model, based on the results of the UK public health survey on eGFR levels by age.40 In addition, the cost of MI complications was used based on an approximation from an Italian study39 and relative risks of CV complications from the literature and the United States national data system.41,42
Progression in the microsimulationIndividuals progressed through the simulation in annual increments from 2022 to 2027. Increasing age during this period affects the risk of age-related complications and all-cause mortality, as well as the likelihood of a new CKD diagnosis or progression of existing disease. Consequently, the health status of each virtual person was updated annually until estimated death or the end point of the study.
To determine disease progression rates, eGFR slopes were generated by regression analysis from the DISCOVER CKD database, which includes retrospective and prospective data from CKD subjects in China, Italy, Japan, Sweden, the United Kingdom and the United States.43 These were individually assigned to each subject in the simulated population based on clinical characteristics, such as the presence of comorbidities and CV complications.
To determine the occurrence of CV events, relative risks of occurrence of CV complications were used based on CKD category and A1-A3 category for CVA,41 and by CKD category, A1–A3 category and age group (<65 and ≥65 years) for MI and HF.42
Estimation of economic burdenTo estimate the economic burden, the direct costs of CKD were taken into account; i.e., the costs derived from progression to the different health statuses and the succession of episodes for each virtual person. Costs associated with CKD diagnosed in categories G3a-G5,37,38 costs of RRT (HD, PD and transplant incidence and maintenance)35,36,38 and costs associated with CV complications26,34,39 were included. The costs of CKD in categories G1 and G2 were assumed to be zero due to the lack of diagnosis and the reduced need for CKD-associated treatment in these categories. Indirect costs, such as social benefits for incapacity for work and expenses for subjects and their families, were not included owing to inconsistencies in health data between different regions.
Results and sensitivity analysisClinical burden results included projected annual prevalence of CKD by G category (G1–G5), age, diagnostic status and comorbidities (T2DM, hypertension), as well as RRT by type (HD, PD and kidney transplant) and CV complications associated with CKD. Economic outcomes included projections of direct costs of CKD by G category, age, diagnostic status and comorbidity, of RRT by type and of CV complications in the population with diagnosed CKD. As a contextual reference measure for the results, the most recently published public health expenditure in Spain, estimated at 87.941 billion euros in 2021, was assumed.44
A sensitivity analysis of the number of subjects on RRT was carried out from the Spanish Registry of Kidney Patients, which has more recent data.13,24
Model validationA scientific steering committee made up of local clinical experts from each of the 31 regions, provided advice on the modelling approach, conceptualisation, clinical assumptions, parameter validation, addressing missing data, model calibrations and interpretation of results from a global and local perspective.24 The microsimulation was validated with five different types of verification: visual inspection, internal validation, external validation, predictive validation and cross-validation, to compare the results of the Inside CKD study with those of other models with previously published results.21
ResultsBaseline characteristics of the population studiedThe baseline characteristics of the population in Spain in 2022 are shown in Table 1. Spain is in line with other high-income regions in terms of epidemiological trends that may affect the prevalence of CKD. The prevalence of comorbidities such as diabetes (6.3%) and hypertension (19.2%) were lower than the average proportion in other high-income regions. However, the proportion of the Spanish population aged ≥65 years (20.1%) was slightly higher. Spain is expected to see an 11.5% increase in the population aged 65 or over by 2027.
Baseline characteristics of the study population.
| Value | |
|---|---|
| Sex, % | |
| Male | 51.03 |
| Female | 48.97 |
| Age, years, % | |
| 0−17 | 17.26 |
| 18−34 | 18.29 |
| 35−64 | 44.30 |
| ≥65 | 20.15 |
| CKD category, % | |
| G1 | 1.65 |
| G2 | 1.82 |
| G3a | 5.65 |
| G3b | 1.32 |
| G4 | 0.24 |
| G5 | 0.04 |
| CKD diagnosed, % | 3.39 |
| Comorbidities, % | |
| Diabetes | 6.3 |
| Hypertension | 19.2 |
| Coronary heart disease | 3.5 |
| History of cerebrovascular accident | 1.3 |
| Obesity | 23.8 |
| Smoker, % | 6.3 |
CKD: chronic kidney disease.
The estimate of prevalence for 2022 was obtained from data between 2004 and 2010 of subjects who meet the diagnostic criteria for CKD, according to the baseline characteristics of the population, including demographic characteristics (age and sex) and levels of eGFR and albuminuria by age (Appendix A, Tables S2 and S3 in additional materials) and estimating a Spanish population of 47.87 million inhabitants in 2022.22 In Spain, the total prevalence of CKD in categories G1–G5 is expected to increase from 5.14 million cases in 2022 to 5.68 million cases in 2027. This equates to an increase in prevalence from 10.7% in 2022 to 11.7% in 2027, representing an absolute increase of 1% in the total population in Spain and a relative increase of 9.3%.
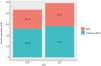
However, the number of CKD subjects without diagosis remains high and it is estimated that only 31.6% of subjects with CKD will be diagnosed in 2027. Specifically, it is expected that 1.80 million subjects with CKD will be diagnosed, while 3.88 million individuals with CKD will not be diagnosed (Fig. 1). The largest increase in prevalence is observed in subjects with CKD in category G3a, who will represent more than 500,000 additional subjects in 2027 (97% of the total growth).
Of the total number of subjects diagnosed with CKD, it is estimated that 3.9% (69,815/1,798,658) will require RRT in 2027, equating to an increase of 14.7% compared to cases in 2022. This increase is observed in all types of RRT and it is estimated that 49.3% of subjects would be on HD or PD (Fig. 2).
Projection of the prevalence of the number of people on RRT in Spain between 2022 and 2027.
The points in the figure reflect actual historical data from the Spanish Registry of Kidney Patients (REER). The bars show the growth projection for each type of RRT between 2022 and 2027.
RRT: renal replacement therapy.
In subjects with diagnosed CKD, the incidence of CV complications remains high throughout the period analysed, with a cumulative incidence of 183,464 new cases between 2022 and 2027, including 89,836 cases of HF, 46,745 of MI and 46,883 of CVA. All-cause mortality in these subjects also remains high throughout the period. A total of 654,281 cumulative deaths are expected in subjects with diagnosed CKD between 2022 and 2027.
The highest number of CV complications and deaths will occur in category 3a owing to the larger population size in this category, although the risk of CV complications and death increases as CKD progresses.
Economic burden of chronic kidney disease in SpainIn subjects with diagnosed CKD, the projected economic burden in Spain was estimated at 4.29 billion euros in 2022 and is expected to rise to 4.89 billion euros in 2027; an increase of 13.8%. This equates to 4.88% of the 2021 Spanish public health expenditure in 2022, and 5.56% in 2027.44 The annual healthcare cost of each eGFR G category and each type of RRT among subjects with diagnosed CKD is shown in Fig. 3. The greatest budgetary impact will be seen in the group of subjects with CKD who will not require RRT (2.811 billion euros in 2027), followed by subjects on HD (1.571 billion euros in 2027).
The cost associated with RRT was estimated at 40.1% of the total cost of CKD in 2022 and is expected to rise to 42.5% in 2027 (increase of 19.3%). Therefore, subjects on RRT represent a disproportionate economic burden for their volume, exceeding 2 billion euros (equivalent to 2.4% of Spanish public health expenditure in 2021) for the treatment of 3.9% of subjects diagnosed with CKD in 2027 (Fig. 4).
Sensitivity analysisCurrently, real data are available on subjects on RRT in Spain in 2021, in which 65,740 subjects with CKD required RRT and 35,777 had a functioning kidney graft,13,24 figures that the initial simulation did not expect to reach until 2026 (Fig. 2) and until after 2027, respectively. For this reason, the model was updated to project the number of subjects on RRT to increase to 75,745 cases in 2027. (+8.5% on the initial projection). This increase in subjects on RRT would result in a greater economic burden that will be 5.03 billion euros in 2027. The impact of this change will represent an increase of 3% in total annual healthcare costs and 8% in RRT, over the costs initially estimated.
DiscussionInside CKD is the first programme designed to analyse the projected prevalence and current and future clinical and economic burden of CKD on a global scale,21 making it unprecedented in the scale of assessment and the wide variety of countries included in the analysis. This study presents the results on the prevalence and burden of CKD between 2022 and 2027 in Spain, which will facilitate the assessment of new strategies to meet local needs arising from the disease. The results indicate that the clinical and economic burden of CKD is expected to increase substantially in the coming years. This increase is mainly due to the contribution of the disproportionate cost of RRT and the projected increase in the prevalence of advanced stages of the disease (G3a-G5).
In the microsimulation, projections indicate that only one third of CKD subjects will be diagnosed, which will mean that a very high proportion of CKD subjects will not be diagnosed in 2027 (68%). Consequently, there is a need to update the strategy for tackling CKD developed by the Spanish Ministry of Health in 2015,45 with special emphasis on early diagnosis and prevention, as well as to update and implement, at the different regional health bodies, preventive interventions to help primary care providers identify and subsequently record CKD in its initial stages, all in line with the recommendations of the latest consensus documents for the detection and management of CKD published in Spain.9,46 In Inside CKD, the clinical and economic consequences of subjects with diagnosed CKD were projected, as this is the burden perspective that the National Health System will identify. However, the actual clinical and economic burden of CKD is logically much higher if the burden associated with undiagnosed CKD is also assessed.
In Spain, the proportion of people over 65 years of age is relatively high, and growing, as compared to other regions of the world, reflecting favourable socioeconomic conditions with better access to healthcare and innovation. However, as the population ages, it becomes more vulnerable to comorbidities and CKD-specific complications. In this analysis, the clinical burden is projected to increase substantially between 2022 and 2027, with a projection of more than 180,000 new CV complications and more than 650,000 deaths in subjects with diagnosed CKD. Furthermore, population ageing is likely to continue to drive an increase in the prevalence and burden of CKD, with important implications for healthcare resource allocation.47 The results consider that the economic burden of diagnosed CKD will continue to increase in the coming years, reaching 4.89 billion euros in 2027, and that a large part of this increase is due to the high economic burden of RRT. Specifically, it is estimated that 42.5% of the costs associated with CKD will be allocated to 3.9% of subjects diagnosed with CKD: those who will require RRT in 2027. In the sensitivity analysis, using the most up-to-date data from the Spanish Registry of Kidney Patients,13,24 the estimated economic burden of diagnosed CKD will be even greater and will reach 5.03 billion euros in 2027.
Given that it was not the objective of this study, the clinical consequences of different treatments were not included in the modelling of disease progression and subjects were considered to be treated with RAAS inhibitors. In recent years, several drugs have been approved for CKD owing to their broad benefits in slowing the progression of CKD and reducing related complications, including SGLT2 inhibitors.9 These drugs will play an important role in reducing the clinical and economic burden estimated in this paper.
The estimates in this article are in line with previous estimates of the economic burden of CKD in Spain. In 2010, Arrieta36 estimated that RRT accounted for between 2.5% and 3% of the Spanish public health spending budget and more than 4% of the budget for specialised care. In 2016, Ortiz et al.15 estimated that subjects on RRT consumed between 2% and 5% of the health budget in Spain. Furthermore, these results are in line with recent estimates from other countries, such as the United Kingdom, which has found that CKD represents a public health emergency and accounts for 3.2% of the budget of its national health service.48 The results of this paper are also in line with previous projections of the burden of CKD published in Europe. Projections of the clinical and economic burden of CKD in the UK between 2020 and 2025 indicated that the prevalence of CKD would increase by 1% (from 13% to 14%), with an increase in the total cost of the disease of 11.8% (from £12.51 billion to £13.99 billion).49,50 Subsequently, Mennini et al. published the projection of the burden of CKD in countries around the world between 2021 and 2026. In this study, it was projected that Spain would see a 14.9% increase in total costs of CKD, similar to that of neighbouring countries, such as Italy and the United Kingdom, with an increase of 10.8% and 16.4%, respectively.51
Given its increasing prevalence and its significant associated clinical and economic burden, CKD is undervalued in relation to other chronic diseases; so much so that, in different chronicity strategies, CKD is not included.52 This observation is reflected in the lack of early diagnosis and awareness of the disease, important factors for treatment adherence and effective provision of clinical care, which are currently low in CKD.53 However, work is being done on different initiatives promoted by scientific societies, patient associations and government agencies, with health administrations and primary care providers, to raise awareness of CKD and promote early diagnosis, which could improve diagnostic forecasts in the future.14,15,52
Simulating a complex disease, such as CKD, in a model introduces certain limitations. Firstly, it is necessary to group data from different sources to fill up the model, and the existing variability in the different studies and information registries carries a risk of bias in the accuracy of the results. To reduce uncertainty in cases where adequate local data were not available, data from a country with a similar healthcare system (UK and Italy) were selected using a study-specific algorithm and with the advice of a panel of experts. The collection of data for this analysis highlights the crucial need for additional nationwide epidemiological studies of CKD to better understand the current disease situation, especially in less advanced stages.
A further limitation of CKD modelling lies in the variables included. CKD is a disease associated with various complications and comorbidities, such as T2DM or hypertension, and the distinction between the causes and consequences of the disease is blurred; hence, there is a risk of overestimating the clinical and economic burden of the disease. To avoid overestimations, hospitalisation costs, which could be counted twice with CV complications, were not included; nor were other non-CV complications, such as vascular and infectious processes, and it was conservatively assumed that the direct costs of CKD in categories G1 and G2 were zero. Due to the paucity of data in the literature, indirect costs such as social benefits for incapacity for work, expenses for subjects, their families and caregivers, and home adaptations for home treatment were not evaluated in the scope of the project despite the obvious major social impact of RRT, especially dialysis. The Inside CKD project also failed to take into account the potential impact of the COVID-19 pandemic on kidney health, as it began before the outbreak, or its impact on the reduction of healthcare resources available to the population. However, all this burden associated with CKD exists and will represent an additional hidden clinical and economic burden that has not been evaluated, which could be even greater than estimated in this paper.
Finally, the population on RRT between 2022 and 2027 is underestimated, since in 2021 the figure forecast for 2022 was exceeded, with 65,740 people on RRT, corresponding to the estimate for 2026.13,24 According to the most recent data from the RRT patient registry, the growth of transplant recipients in Spain will be greater than that forecast in the projection, owing to the efforts of the administrations and health services to increase transplantation. Furthermore, the clinical and economic consequences analysed arise only from the population with diagnosed CKD, equivalent to one third of the population with CKD. Hence, several of the limitations point to an underestimation of the real burden of the disease and its impact on the health budget.
ConclusionsBy way of conclusion, the Inside CKD project demonstrates the growing and relevant clinical and economic burden of CKD in Spain, despite several limitations that indicate that the disease burden and budgetary impact are an underestimate. As repeatedly claimed by a group of key stakeholders, including scientific societies, patient associations and government agencies,14,15,52 there is a need to implement health strategies and policies aimed at prevention, early diagnosis and proactive intervention to reduce progression to more advanced stages and related comorbidities, since people on RRT, who represent a very small proportion of the total CKD population, contribute disproportionately to the total costs. Implementing preventive strategies could slow disease progression and reduce the clinical and economic burden of the disease, while improving the quality of life of subjects.
FundingInside CKD is funded by AstraZeneca. Inside CKD is a microsimulation data-driven project, owing to which no drugs were supplied or funded. Statistical analyses were funded by AstraZeneca. PharmaLex received funding from AstraZeneca for the conduct of this study.
The research of AO and JFNG is funded by the Community of Madrid in Biomedicine P2022/BMD-7223, CIFRA_COR-CM; the Instituto de Salud Carlos III [Carlos III Health Institute] (ISCIII) RICORS programme to RICORS2040 (RD21/0005/0001), funded by the European Union – NextGenerationEU, Recovery and Resilience Facility (RRF) and European Regional Development Fund (ERDF). AO's research is also funded by PREVENTCKD Consortium Project ID: 101101220 Programme: EU4H DG/Agency: HADEA.
The authors would like to thank the Global Inside CKD team, comprising Salvatore Barone and Claudia Cabrera from AstraZeneca, and Laura Webber and Lise Retat from Health Lumen, for the design and execution of the Inside CKD modelling.