Terminal-stage patients on peritoneal dialysis (PD) are often transferred to haemodialysis as they are unable to perform the dialysis technique themselves since their functional capacities are reduced. We present our experience with five patients on PD with a short-term life-threatening condition, whose treatment was shared by primary care units and who were treated with a PD modality adapted to their circumstances, which we call Palliative Peritoneal Dialysis.
Los pacientes en Diálisis peritoneal (DP) en situación terminal suelen ser transferidos a hemodiálisis ya que son incapaces de realizarse la técnica dialítica a consecuencia de que sus capacidades funcionales están disminuidas. Presentamos nuestra experiencia con 5 pacientes en DP con patología que amenazaba su vida a corto plazo, cuyo tratamiento fue compartido por las unidades de atención primaria y fueron mantenidos en una modalidad de DP adaptada a sus circunstancias a la que hemos denominado Diálisis Peritoneal Paliativa.
Terminal-stage patients on peritoneal dialysis (PD) whose pathology is life threatening in the short term have reduced functional capacities and serious difficulties in performing peritoneal exchanges or attending regular check-ups at the hospital. Under these circumstances, patients in the PD programme are often transferred to haemodialysis (HD). However, since they are conscious of their end-stage condition, some patients who had opted for PD to maintain their personal independence express their desire to die at home and remain on PD until the end. The current health care organisation in Spain does not offer this possibility. We present our experience with a home care programme for terminal patients on PD who are managed in collaboration with their primary care physician (PCP) and maintained on PD until their death.
Patients and methodsBetween May 1995 and December 2013, 307 patients with PD were treated by our Department, 5 of whom required palliative care due to an irreversible pathology with a short-term fatal prognosis. We analysed their data retrospectively from the PD Unit database. All the patients had expressed their desire to die at home, so it was necessary for them to remain on PD and not be transferred to HD. Making palliative care and PD compatible with the current functional structure of our Unit did not seem an easy task, although we wanted to meet all our patients’ wishes.
Therefore, we contacted their PCP to ask him/her to share in the patients’ follow-up and dialysis technique. A primary care (PC) nurse underwent a short training course (one to three days) in the PD Unit. This was necessary because, while three of the patients lived with family members who were familiar with the technique, two patients lived alone. Besides, as the nurse was going to be their closest contact, we believed it was convenient for him/her to learn the technique in order to inspire higher confidence in the patient and family members. We also trained a member of the ancillary staff of a public Long-Stay Unit (LSU) for chronic patients. This staff member trained the other members of the unit, where one patient was admitted until his death.
The primary care staff drew blood samples for lab tests at the patients’ homes, and the results were reported to us by phone along with clinical patient information. Blood tests included haemogram and basic blood chemistry. No urinalysis, Kt/V or PET measurements were ordered in any of the cases. The frequency of home visits and blood tests was established by the PCP and adjusted to the needs of the patient. In this manner, no patient came back to the hospital PD Unit for a periodical medical follow-up.
The pharmacological treatment was adjusted to the needs and situation of the patient. As a general rule, all drugs were discontinued except for erythropoietin and antihypertensive drugs. Medication for symptoms treatment (analgesia, sedatives, etc.) was left at the discretion of the PCP. The physician of the long-term unit played the same role. There was fluent and permanent telephone contact between the PD Unit, caregivers and primary care professionals until death. Below, we present the characteristics of the five patients that required palliative care in our PD Unit. In order to measure the degree of independence of the patients prior to requiring palliative care, we used the Barthel activities of daily living index.
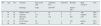
ResultsFour men and one woman were included in this programme. Mean age was 49 (range: 46 to 67) and the Charlson index was 11 ± 5.6 (range: 5 to 18). The underlying disease was: chronic glomerulonephritis (n = 2), radical nephrectomy due to bilateral renal carcinoma (n = 1), diabetic nephropathy (n = 1) and undetermined kidney disease (n = 1). Three patients were HIV positive. Two patients lived alone before reaching the end-stage condition. All were on manual PD technique and independent for activities of daily living (Barthel index 50, 75, 85, 60 and 65, respectively) and able to perform the dialysis technique themselves before experiencing the event that led to their admission to the palliative programme. Four patients were anuretic and the fifth patient had a diuresis of 200 mL/24 h. After 42.6 ± 27 months (range: 16 to 81) on PD, they developed the following nonreversible complications: two cachexia, one hepatic carcinoma with frequent hospital admissions due to encephalopathy, one metastatic squamous cell carcinoma, and one invasive bilateral renal carcinoma relapse. Four patients were treated with family-assisted PD at home until their death, and one patient was treated in a public LSU. The survival was 17 to 119 days, with a mean of 33 days. Only one patient was admitted to the Hospital for three days after initiating palliative care. Assisted PD was manual in all the cases. One or two exchanges per day were scheduled, and in specific cases a third exchange was performed when it was necessary to guarantee ultrafiltration. Four patients were managed with 2.27% glucose and only one patient received icodextrin in the long exchange. The characteristics of the patients are detailed in Table 1.
–.
| Pat. | Age | Sex | Terminal | Days of life until | Admission days | Icodextrin | Residual | Main Caregiver | Year |
|---|---|---|---|---|---|---|---|---|---|
| Pathology | death | after PCP | diuresis (mL) | ||||||
| 1 | 67 | H | Kidney Cancer | 5 | 20 | 0 | 0 | wife | 2001 |
| 2 | 49 | M | Cachexia | 115 | 39 | 0 | 0 | daughter | 2007 |
| 3 | 53 | H | Metastatic Cancer | 40 | 119 | 0 | 200 | LSU | 2010 |
| 4 | 48 | H | Liver Cancer | 40 | 33 | 3 | 100 | parents | 2011 |
| 5 | 46 | H | Cachexia | 113 | 17 | 0 | 0 | aunt | 2013 |
Palliative Care Units (PCU), which have traditionally focused on patients with terminal-stage cancer, have had to widen their field of action in recent years due to the increasing demand for assistance and palliative support by patients with chronic, progressive non-cancer pathologies.1–3
At the beginning of the 21st century, palliative care extended to include other pathologies, such as chronic kidney disease, with the intention of humanising and easing the transition to death, not only for patients but also for their family members4,5. Thus, in recent years there has been a growing interest within the nephrology community to offer palliative care to patients with chronic kidney disease. This is either because they are not eligible for dialysis and would therefore start conservative treatment, or because discontinuation of dialysis treatment is considered the best option. In this regard, there are several excellent publications where the need for multidisciplinary palliative care units for renal patients was justified and the grounds were set forth, not only in Spain but also worldwide6–8.
But, what if the patient is eligible for palliative care and does not want to discontinue dialysis? The decision to discontinue dialysis raises concerns. It is perceived as suicide in up to 12% of patients9, and it may even be considered euthanasia from a family standpoint. This dilemma is partially solved through the new “palliative dialysis” concept10, which basically involves continuing dialysis treatment but replacing the usual targets of dialysis efficiency (Kt/V, dry weight, PTH levels, etc.) with asymptomatic patient targets. Thus, palliative dialysis consists in individualising the dialysis prescription for each patient, focusing on ultrafiltration rather than on the clearance of uraemic solutes. The palliative dialysis mentioned in the literature is, in fact, palliative HD, and patients on PD who may require palliative care would be transferred to HD when they are not independent enough to make exchanges themselves.
Moreover, what if patients on PD who require palliative care do not want to change their dialysis technique? That is to say, if patients have chosen home dialysis and express the explicit desire to continue said treatment when facing the end of life, should we keep them on PD or transfer them to HD? This is the situation of our patients. The first time we faced this event was in 2001. As mentioned above, our patient had a highly invasive bilateral renal carcinoma recurrence with a poor short-term prognosis. The patient had the support of family members who were trained in the technique, but he needed an individualised treatment, at home if possible, for the tumour-related symptoms. Given this circumstance and wishing to respect this request, we opted to contact the patient's PCP. After explaining the situation, we asked the physician to share in the responsibility of monitoring the patient and dialysis technique with us. This request was immediately accepted. Our nursing staff gave the visiting nurse a short training session on the PD technique. This patient died 20 days later, without requiring office visits or hospital admission. We have repeated the experience four more times. In each case, both the patients and families have personally manifested their satisfaction to us, while we ourselves have also felt satisfied. We must highlight that patient No. 3 was admitted to a publicly-funded LSU and treated with PD until the moment of death 119 days later. In this case, a member of the LSU ancillary staff was trained at our PD Unit and was later able to teach the LSU staff.
Since 1990, the Community of Madrid has progressively implemented a health care resource directed at providing palliative care services for both Specialised Care and Primary Care. Family members of treated patients and the participating staff themselves have shown a high rate of satisfaction with this high-quality care11. In 1991 and 1992, Health Areas 4 and 11 initiated specific programmes directed towards terminal patients that were based on the collaboration between Primary and Specialized Care in order to ensure continuous care. In addition, six home care support teams12 were created in 1999, under the management of Primary Care, in order to collaborate with and support PCP when treating immobilised terminal-stage patients. Subsequently, Act 16/2003 (from May 28th) on the Cohesion and Quality of the National Health Care Service specifically included palliative care for terminal patients, both in Primary Care and Specialised Care services. The health area of Ramón y Cajal Hospital and Gregorio Marañón Hospital was a pioneer in the implementation of specialised and continuous care programmes for terminal patients based on the collaboration and coordination between Primary Care and Specialised Care. These programmes are aimed at any and all patients at a terminal stage, including renal patients. In its 2004 report, the ESAD (Equipo de Soporte de Atención Domiciliaria [Home Care Support Team]) of the Community of Madrid assisted 24 terminal nephrology patients, as detailed in its report11.
Assisted peritoneal dialysis, performed by either qualified staff or a family member, is a good solution for patients on PD at a terminal stage without the need to transfer them to HD13. The traditional model of assisted PD is based on using a cycler at night with a dry day, which makes the dialysis technique compatible with the daily life of the caregiver and avoids overburdening him/her. This modality was not applied in our patients since all of them received manual PD treatment and there was no training with cyclers. What we propose for terminal patients on PD is, in fact, Palliative Peritoneal Dialysis, which we define as PD therapy that, on the one hand, can keep the patient free of symptoms such as dyspnoea and, on the other hand, makes the patient feel cared for (dialysed) until the end, without overwhelming the main caregiver.
In our experience, this has been possible through manual peritoneal dialysis with 1 or 2 glucose exchanges every 24hours. In patients in whom blood volume control is a priority, a long icodextrin day exchange combined with a glucose night exchange could be the recommended pattern.
To summarise, PD may be continued until the end of life of patients at a terminal stage, without transferring them to HD and without overburdening the caregiver. In our experience, the support of primary care professionals was essential to provide these patients with proper, individualised treatment and to comply with the Patient Autonomy Law14. Selfless support provided by the primary care staff allowed patients to continue PD treatment and to receive home care without the need to be transferred to HD, thus respecting their desire to die at home. Assisted Palliative PD is well accepted by family members and does not involve a severe burden during the short survival of said patients. Decision-making in patients with an end-stage condition must be shared, while taking into consideration the patient's clinical situation, prognosis, quality of life and desires. In cases where PD discontinuation may increase the anxiety and distress of the patient and family, we believe that palliative peritoneal dialysis is a good solution.