Antecedentes: El perfil clínico de los donantes fallecidos se está transformando velozmente hacia un incremento de donantes con criterios expandidos (DCE), por lo que el número de riñones descartados para trasplante está creciendo. Con la finalidad de optimizar el aprovechamiento de riñones de DCE que individualmente podrían aportar una masa renal insuficiente, se ha sugerido su utilización como TX doble o birrenal (TXB). Pacientes y métodos: En un estudio de casos y controles, se analiza la experiencia de un único hospital entre mayo de 2007 y marzo de 2011. Los criterios para decidir TX único o doble quedaron definidos en un protocolo en el que la puntuación de la biopsia era un factor importante, pero no exclusivo, ya que se tenía en cuenta también la edad, los antecedentes del donante, el tamaño de los riñones y el aclaramiento de creatinina. Durante este intervalo se han trasplantado 80 riñones de donantes mayores de 65 años. De ellos, 40 han sido como trasplantes únicos (TXS) y otros 40 como TXB. Resultados: La edad media de los donantes para TXS fue de 68,7 ± 3,0 años y la de los TXB de 74,2 ± 4,3 años (p < 0,001), con predominio de mujeres en TXB (75%) respecto al TXS (40%) (p < 0,001). No se apreciaron diferencias entre ambos grupos respecto a filtrado glomerular o proteinuria. Los riñones derivados para TXB presentaban mayor puntuación en la biopsia que los de TXS (2,95 ± 1,01 vs. 1,8 ± 1,04; p < 0,001). Los receptores de TXB fueron de mayor edad que los de TXS, no encontrando diferencias entre grupos respecto a isquemia fría, retraso de la función del injerto, complicaciones hemorrágicas o reintervenciones. Sin embargo, los receptores de TXB alcanzaron mejor aclaramiento de creatinina en los cortes de 1, 3, 6 y 12 meses, aunque sólo resultara estadísticamente significativo a los 6 meses (53,4 ± 19,5 ml/min vs. 44,5 ± 15,6 ml/min; p < 0,05). La trombosis de arteria renal se presentó en dos pacientes de TXS y en los dos riñones de un paciente de TXB. Otros dos pacientes de este último grupo perdieron un riñón cada uno por trombosis y necrosis del uréter, respectivamente, aunque se mantuvieron libres de diálisis con supervivencias del injerto del 90% a los tres años para ambos grupos. Tres pacientes fallecieron en el período estudiado (dos en el grupo TXS y uno en el TXB). Conclusiones: Esta experiencia preliminar indica que el TXB ofrece buenos resultados en cuanto a datos de supervivencia y función renal, a pesar de cirugías más complejas y características que probablemente no les hacía idóneos para TXS. La decisión de realizar TXB facilita la utilización de riñones de DCE y debería apoyarse en la combinación de criterios histológicos pretrasplante y las características clínicas de los donantes.
Introduction: In order to take full advantage of ECD kidneys, which may not provide sufficient renal mass if used individually, it has been suggested that such organs be used in dual or bilateral kidney transplantation (DTx). Patients and method: We analysed the experience in a single hospital between May 2007 and March 2011 in a case-control study. Criteria for determining whether to perform single or dual Tx were defined in a protocol in which the biopsy score was important, but not the only factor. Donor's age, medical history, kidney size and creatinine clearance were also considered. During this time period, 80 kidneys from donors over age 65 were transplanted. Single transplants (STx) accounted for 40 of the organs, and another 40 were used in DTx. Results: Mean donor age for STx was 68.7±3.0 years; for DTx, it was 74.2±4.3 years (P<.001), with more female donors for DTx (75%) than for STx (40%) (P<.001). There were no differences between groups with regard to glomerular filtration rate or proteinuria. Kidneys assigned to DTx received higher biopsy scores than those assigned to STx (2.95±1.01 vs 1.8±1.04; P<.001). DTx recipients were older than STx recipients. There were no differences between the groups regarding cold ischaemia time, delayed graft function, haemorrhagic complications or re-surgeries. However, DTx recipients achieved better creatinine clearance at 1, 3, 6 and 12 months, although the difference was only statistically significant at 6 months (53.4±19.5ml/min vs 44.5±15.6ml/min; P<.05). Renal artery thrombosis appeared in 2 STx patients and in both kidneys of 1 DTx patient. Another 2 patients in the DTx group each lost 1 kidney due to thrombosis and ureteral necrosis respectively, but were able to remain dialysis-free. Graft survival at 3 years was 90% for both groups. During the study period 3 patients died (2 in the STx group and 1 in the DTx group). Conclusions: Our preliminary experience indicates that DTx provides good results in terms of survival and renal function data, despite surgery being more complicated and the organs having characteristics that probably make them unsuitable for STx. The decision to perform DTx makes using ECD kidneys easier, and it should be based on a combination of pre-transplant histological criteria and the donor's clinical characteristics.
INTRODUCTION
Changes in the organ donor profile in Spain have resulted in a gradual increase in numbers of donors who are elderly, have co-morbidities1 and who die due to cerebral vascular accidents. These factors affect renal function and allograft survival in transplant recipients.2
Meanwhile, mean ages of kidney transplants (Tx) recipients have increased; today it would be quite uncommon for a patient on the Tx waiting list to be excluded based on age alone. This practice is supported by studies that show that for all age groups, including septuagenarians, kidney transplant recipients live longer than patients of similar ages who remain on the waiting list and never receive transplants.3,4 The current situation therefore includes growing numbers of both elderly recipients and elderly donors.
Unfortunately, given a scenario with numerous expanded criteria donors (ECD), a significant number of harvested kidneys are discarded in the end due to uncertainty about their being able to function acceptably as grafts. This is currently the leading cause of kidneys being declared unacceptable for transplantation, both in Spain and abroad. For example, according to the UNOS database for 2009, 2762 kidneys harvested in different transplant centres in the United States (19% of the total) were discarded, and this figure increases year after year.5 In our own region of Andalusia, according to Andalusian Transplant Coordination Authority data (currently unpublished), a total of 149 kidneys (32.1% of the total) were discarded in 2010. This figure is slightly higher than the mean in Spain.
Nevertheless, some of these organs may have been viable for transplants. The decision to discard them is taken based on an urgent evaluation following harvest which considers donor history, macroscopic appearance and results from a kidney biopsy, even though the biopsy findings may have poor predictive value beyond previously known information. Although scientific evidence is quite limited, biopsy results are being used to determine whether a kidney will be accepted for transplant or discarded.6
Several years ago, in order to optimise ECD kidney use, doctors suggested that these organs could be accepted as long as they were used in paired or dual kidney transplants (DTx). Medium- and long-term results from DTx procedures were published by OPTN/UNOS in the United States7 and by numerous authors.8-10 This led to a growing trend in ECD kidney use in hospitals that had previously discarded them for not meeting the quality standards established for single Tx. Experiences with DTx have also been reported by different Spanish hospitals, with acceptable results.11,12 However, despite the fact that DTx has proven itself useful, it is not widely performed in Spain; fewer than 30 DTx are performed yearly, well below the averages recorded in Europe13 and the United States.14
We must keep in mind that the goal is to match possibilities with needs by considering each recipient’s biological data (advanced age, lower rejection rate, shorter life expectancy, etc.). This encourages use of DTx as a valid option for transplanting pairs of certain types of kidneys in selected recipients.
Lastly, the aim of our study was to analyse results of DTx procedures performed in the Hospital Regional Universitario Carlos Haya, which has been the centre of reference for DTx in Andalusia since 2007.
PATIENTS AND METHODS
We analysed kidney donation and transplantation activity in the Malaga province between May 2007 and March 2011. During these 47 months, 333 donors were recorded by different hospitals within the Malaga province. Of these donors, 219 were younger than 65 (65.7%) and 114 older than 65 (34.2%). A total of 96 kidneys from the first group were not transplanted (53 due to macroscopic or microscopic defects; 28 due to prior disease; 15 due to lack of matched recipient). For the donors older than 65, 140 kidneys were discarded (63 due to prior disease and 77 due to macroscopic or microscopic lesions).
The inter-group analysis was designed as a case-control study. Cases were the 40 kidneys approved for DTx in 20 patients. Thirty-two kidneys were harvested in hospitals within the Malaga province, while 8 came from hospitals in other Andalusian provinces (Granada 4; Huelva 2; Córdoba 2). Controls consisted of single transplants (STx) performed in 40 patients in Hospital Carlos Haya during the same time period (2007-2011), where donors were older than 65 years with no other selection criteria.
The decision to accept or reject ECD grafts was made based on results from the pre-transplant biopsy. Biopsy samples, taken once the harvest team had finished the harvesting process, consisted of wedges of renal tissue measuring 10mm by 5mm by 5mm from a representative part of the renal parenchyma that were large enough to permit study of 25 or more glomeruli and two small-calibre arteries in each kidney. The study was carried out using cryostat sections stained with haematoxylin-eosin and methylene blue. The evaluation screened for four types of lesions: sclerotic glomeruli, myointimal hyperplasia, tubular atrophy, and interstitial fibrosis. Each lesion type was given a score between 0 and 3 points, ranging from no lesions to mild, moderate, or severe damage.15 All kidney biopsies were interpreted by the same 2 pathologists at Hospital Carlos Haya.
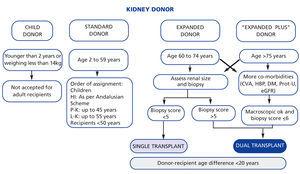
Criteria for deciding whether to perform single or dual TX were defined in a protocol in which the biopsy score was important, but not the only factor. Donor's age, medical history, kidney size and creatinine clearance were also considered. DTx recipients were informed about this option by the nephrologist on duty, and they signed the appropriate consent forms. Figure 1 shows the algorithm used in decision-making.
Dual kidney transplantation was performed through 2 independent incisions in each of the recipient’s iliac fossae. Cold ischaemia time was defined as the arithmetic mean of the time to unclamping for each of the two kidneys.
There were no differences in immunosuppressant regimens between the STx and DTx groups. The treatment basically consisted of induction with anti-CD25 antibodies (basiliximab), steroids, tacrolimus introduced on the 3rd or 4th post-operative day to maintain levels of 8-12ng/ml during the first 90 days, and mycophenolate mofetil. There were no differences in follow-up after admission to the Tx unit between single or dual kidney recipients.
Statistical analysis
Numerical data are expressed as percentages, mean ± standard deviation or median with interquartile ranges, as appropriate. Quantitative variables were compared using Student’s t-test or the Mann-Whitney U test if they did not follow a normal distribution, which was determined using the Shapiro-Wilk test. Either the chi-squared test or Fisher’s exact test were used for qualitative parameters, as appropriate. Graft survival rates in both groups were calculated using Kaplan-Meier curves and the log-rank test. Patients in the DTx group who maintained function in one of the two graft kidneys were considered dialysis-free for purposes of measuring graft survival. Values of P<.05 were considered statistically significant. Data analysis was performed using SPSS statistical software, version 15.0 (SPSS Inc, Chicago, IL).
RESULTS
During the study period, 396 cadaver-donor kidneys were transplanted in our hospital. Of these organs, 80 came from donors older than 65 years.
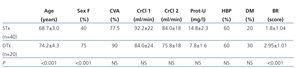
Table 1 summarises the main characteristics of the donors in each of the 2 study groups. Donors of kidneys that were transplanted as DTx were older and mainly female. There were no differences between the 2 study groups with regard to renal function, proteinuria, hypertension, diabetes, or cause of death. All kidneys were biopsied, and those with a score of more than 6 were ruled out for transplant. Mean biopsy scores for the STx group were 1.80±1.04 vs 2.95±1.01 for the DTx group (P<.001).
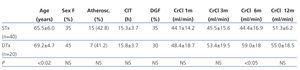
Table 2 lists the most relevant characteristics of recipients in the 2 study groups. Mean age was higher in the DTx group. There were no differences with regard to moderate-to-severe atherosclerosis, which was present in 15 (42.8%) STx recipients and in 7 (41.2%) DTx recipients. Cold ischaemia times were similar for both groups, as were the percentages of grafts with delayed function. Creatinine clearance (CrCl) estimated by the MDRD method (Modification of Diet in Renal Disease Study Group) was slightly higher in the DTx group than in the STx group, but this difference was only statistically significant 6 months after Tx (P<.05).
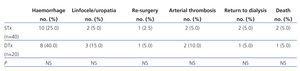
Most complications occurred immediately after transplantation. Table 3 shows the main complications in both groups. There were 2 cases of vascular thrombosis in the STx group that resulted in nephrectomy and return to dialysis. In the DTx group, 1 kidney was lost due to ureteral necrosis and the patient maintained a Cr level of 2.9mg/dl with a CrCl rate of 20ml/min. Additionally, 2 patients experienced arterial thrombosis, which was bilateral in one case and unilateral in the other. The latter case remained dialysis-free with serum creatinine levels at 1.9mg/dl and a CrCl rate of 36ml/min.
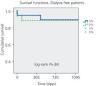
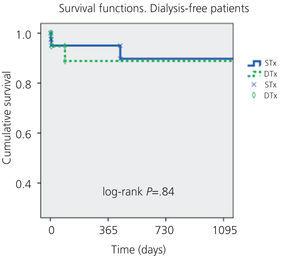
Figure 2 shows overall survival rates for kidney graft in each of the study groups (not death-censored). The median follow-up period was 410 days for the STx group and 284 days for the DTx group; the dialysis-free graft survival rate was 90% at 3 years (P=NS).
One patient with DTx died in the third month due to bilateral pneumonia. Two patients in the STx group died due to sepsis and neoplasia at 14 and 44 months, respectively.
DISCUSSION
Although DTx make up a small percentage of the total cadaver-donor transplants performed in our hospital (5.6%), they present yet another option for optimising the use of kidneys from donors older than 65 years, as shown by our study.
The question of what to measure in expanded criteria donors, and how to measure it, remains controversial. An ideal method would be objective, reproducible and more reliable in identifying high-risk donors, kidneys that are acceptable or unacceptable for Tx, and kidneys that would provide reduced renal function as grafts.16 Using intuition in addition to transplantation records and data from large cohorts, we can point out certain donor characteristics that are associated with poorer functional stages and lower graft survival rates.17,18 Several nomograms have been proposed for evaluating ECD, generally defined as donors 60 years of age or older or donors aged 50-60 with at least two of the following conditions: history of high blood pressure, cerebral vascular accident as cause of death and serum creatinine levels higher than 1.5mg/dl.2 The KDRI (Kidney Donor Risk Index) was introduced in 2009; this index includes conditions in both the donor and the recipient which can lead to allograft failure or significant dysfunction.19 Its webpage lets us calculate the risk of delayed graft function according to variables present in the donor and in the recipient.20
Some groups consider that measuring kidney function using estimated glomerular filtration rate formulas is sufficient for accepting kidneys as long as harvesting reveals no major macroscopic abnormalities.21,22 Others, however, feel that strict acceptability testing is necessary for kidneys from elderly donors, and that histological studies of the graft should always be completed prior to transplantation. Although some authors feel that the percentage of glomerulosclerosis may be a sufficient measure,23 other studies24 and consensus documents support individualised, precise measurements of the abnormalities present in different kidney structures (glomeruli, interstitium and blood vessels) prior to Tx.25
Unfortunately, urgent biopsies that are evaluated based on emergency criteria entail some drawbacks. Some of these weaknesses have to do with the methodology; use of quick cryostat sections and less staining does not enable perfect visualisation of abnormalities involving vascular damage, especially hyaline arteriopathy (usually underestimated) and the degree of glomerulosclerosis (usually overestimated).26 Our hospital opted for a pathology study with quick cryosection and haematoxylin-eosin and methylene blue staining; biopsies were evaluated by the same 2 pathologists. Reading quick-section biopsies has its limitations and does not allow for evaluation of hyaline arteriopathy, our hospital decided to continue using the technique after reading a preliminary analysis of 180 ECD kidney biopsies (currently unpublished). In this study, retrospective evaluation of biopsies from kidneys accepted for Tx based on frozen section biopsies resulted in scores of 3 (which would have ruled out transplant use) in 1.1% due to glomerulosclerosis and 5.6% due to hyaline arteriopathy. This obviously allowed us to continue using the simplified method, which provides reports in less time. The Spanish Society of Nephrology25 recently issued a consensus statement on assessing histological damage in order to decide whether or not a kidney is viable after a certain score threshold.
At the same time, we decided to begin DTx procedures using ECD grafts that could theoretically be discarded due to the histological score being too high (>6). This was in line with Spanish National Transplant Organisation and Andalusian Transplant Coordination Authority directives. This step called for specific selection criteria for the recipients of such grafts: older than 60, absence of cytotoxic antibodies, first-time grafts and no human leukocyte antigen (HLA) match required.
Our team made the technical decision to perform separate implants, placing 1 kidney in each of the iliac fossae using 2 independent approaches. This was considered to lower the risk of complications regarding ureteral integrity and preserving the arterial flow to the lower limbs in patients with differing degrees of atherosclerosis. Other alternatives, such as placing both kidneys in the same iliac fossa so as to preserve the other one for future Tx procedures, have been shown to be useful.28
We understand that despite having defined protocols and algorithms, it is sometimes difficult to accept or discard a pair of ECD kidneys that exceed the normal expanded criteria score29; we might refer to such organs as “expanded plus”. In these cases, the biopsy score constitutes an objective evaluation and it helps the on-duty nephrologist make the final decision by offering a certain guarantee of good results, at least for the short- and medium-term. The fact that survival rates and renal function data were similar in both of our study groups supports this hypothesis. In any case, we must remember that important factors such as experience and intuition, supported by the donor's clinical and analytical data, are also involved in the evaluation process.10
Lastly, some might argue that some of the kidneys used in DTx could have been transplanted separately, thereby benefiting two different patients on chronic dialysis. Little is known about this matter; there have been no studies specifically designed to determine the precise threshold of viability for STx or to determine when organs should be used in DTx or be discarded. The 2 patients in the DTx group who remain dialysis-free with 1 functioning kidney have slightly higher serum creatinine levels than those in the STx group, and this coincides with data from other studies.12
In conclusion, this preliminary study suggests that DTx offers good results as shown by survival rate and renal function data, despite surgeries being more complex. Decisions to perform DTx in experienced Tx centres should be based on the combination of pre-Tx histological criteria and the donors' clinical characteristics.
Acknowledgements
The authors would like to thank all of the kidney coordination, harvest and transplant teams in Andalusia, as well as the Andalusian Transplant Coordination Authority. This study was financed in part by the Andalusian Regional Ministry of Health (PI-0499/2009) and by the Spanish Ministry of Science and Innovation (Instituto de Salud Carlos III, FIS PI10/01020).
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Donor characteristics analysed for both patient groups
Table 2. Recipient characteristics and kidney transplant outcomes
Table 3. Post-operative complications in transplant patients
Figure 1. Algorithm for the decision to choose single or dual kidney transplantation according to the type of kidney donor
Figure 2. Survival of STx and DTx grafts