Aim: Peritonitis is one of the major comorbidities of peritoneal dialysis (PD) patients. The aim of this study was to concentrate on potential risk factors, including more recently studied ones among the classical ones for peritonitis, in PD patients. Materials and methods: We analysed 109 patients (F/M = 42/67) followed up at least for 3 months in a single centre, a tertiary referral hospital for 360.1 patient years. In the study which is designed as a retrospective cohort study, demographic characteristics, conditions for choosing PD, type of PD treatment, some chemical tests and peritonitis episodes were recorded from the files of the patients. Results: The rate of peritonitis was found to be 0.22 episode/patient year and 22 (20.18%) of the patients had more than one episode. Twenty seven (24.8%) of the patients were allocated to PD due to obligatory reasons. According to multiple regression analysis, the assosciated factors were found to be PD allocation type (obligatory versus voluntary) (p = 0.04; RR = 2.6), serum albumin level (p = 0.05; RR = 1.2), and anti-hepatitis C Virus Antibody positivity (p = 0.03; RR = 1.6). Frequency of female patients were significantly higher in the group who had multiple episodes (p = 0.01). Conclusion: Obligatory referral which can be an indication of loss of motivation for peritoneal dialysis procedures, is thought to be a strong risk factor for peritonitis in PD patients and should be further studied. Patients with multiple episodes had a higher frequency of obligatory referral as expected and additionally, they were higher in number of females when compared to the ones with single episode.
Objetivo: La peritonitis es una de las principales comorbilidades que presentan los pacientes en diálisis peritoneal (DP). El objetivo de este estudio es centrarnos en los posibles factores de riesgo, incluidos los de más reciente estudio entre los ya clásicos factores de la peritonitis en pacientes en DP. Materiales y métodos: Analizamos 109 pacientes (H/M = 67/42) sometidos a seguimiento durante al menos tres meses en un único centro, un hospital terciario con una tasa de 360,1 años-paciente. En este trabajo, concebido como un estudio de cohorte retrospectivo, se registraron las características demográficas, las condiciones que llevaron a la DP, tipo de DP, pruebas químicas y episodios de peritonitis. Esta información se extrajo de los historiales. Resultados: Se descubrió que la tasa de peritonitis era de 0,22 episodios/años-paciente y 22 (20,18%) pacientes habían padecido más de un episodio. Veintisiete (24,8%) de los pacientes recibían DP por obligación. Gracias al análisis de regresión múltiple, se descubrió que los factores relacionados eran el tipo de llegada al tratamiento (obligatoria frente a voluntaria) (p = 0,04; RR = 2,6), los niveles de albúmina sérica (p = 0,05; RR = 1,2), y la positividad para anticuerpos contra el virus de hepatitis C (p = 0,03; RR = 1,6). La frecuencia de pacientes mujeres era significativamente mayor en el grupo que había padecido múltiples episodios (p = 0,01). Conclusión: La remisión obligatoria, que puede ser un indicio de la falta de motivación por los procedimientos de DP, es un importante factor de riesgo de peritonitis en los pacientes en DP y merece ser objeto de estudio. Como era de esperar, los pacientes con múltiples episodios presentaron una mayor frecuencia de remisión obligatoria y además, el número de mujeres era mayor en comparación con el grupo que había padecido un único episodio.
INTRODUCTION
Peritonitis is one of the major comorbidities of peritoneal dialysis (PD) patients. Although the incidence of peritonitis has reduced in years with the introduction of new techniques, it still constitutes one of the major drop-outs from PD1-3. It is the leading cause of technical failure and main reason for switching therapy to haemodialysis (HD)4,5. The percentage of end-stage renal disease (ESRD) patients maintained on PD therapy is decreasing in some regions and centres (USRDS data and ANZDATA registry); complications from PD therapy mainly peritonitis, may be the reason for the decline.
There is variability in peritonitis rates by both region and program. Peritonitis rate also varies by individual patients within a program. Risk factors for the development of peritonitis in PD patients are widely studied. Low serum albumin at the begining of dialysis, immunosuppression and staphylococcal nasal carriage are some risk factors determined6,7. Some other controversial risks are age, diabetes and gender8,9. According to some studies, the introduction of automated peritoneal dialysis (APD), using a single connection each night, showed a reduction in the incidence of peritonitis episodes compared with continuous ambulatory peritoneal dialysis (CAPD), as a result of the decrease in the number of daily disconnections10,11. Obligatory referral which can be regarded as an indication of the reluctance of patients for PD is a potential factor studied recently12,13. This study concentrates on potential risk factors, more recently studied ones among the classical ones, for peritonitis in PD patients.
MATERIALS AND METHODS
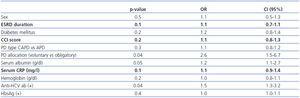
We analysed 109 PD patients (Female:Male = 42:67) followed up at least for 3 months in a centre, a tertiary referral hospital for 360.1 patient years. The mean time on renal replacement therapy and on PD of the patient population were 59.15 (± 43.52) months and 39.75 (± 29.32) months, respectively. Mean age of the patients was 43.4 ± 7.5 years. The most frequent aetiology underlying chronic kidney disease (CKD) was glomerulonephritis (39.4%). The underlying aetiology was diabetes mellitus in 17 (15.6%) of the patients. Twenty two (20.2%) of the patients were on APD treatment. In the study which is designed as a retrospective cohort study, demographic characteristics, conditions for choosing PD, type of PD treatment, some chemical tests and peritonitis episodes were recorded from the files of the patients (table 1). Peritonitis episodes recorded met the criteria of at least 2 of the following 3 conditions: 1) symptoms and signs of peritoneal inflammation; 2) peritoneal cell count exceeding 100 permicroL or polymorphonuclear cells >50% and/or 3) positive culture14. Multiple episodes of the same patient recorded excluding relapsing and recurrent peritonitis. Comorbidity index scores of the patients were calculated using the data from the files by using the Charlson Comorbidty Index (CCI) Score15. Nonparametric two-independent sample (Mann- Whitney U) test was used to determine the differences between different groups of patients such as diabetic patients versus non-diabetics, CAPD patients versus APD patients, patients with single episode versus patients with multiple episodes; and multiple regression analysis (for the analysis of time to first peritonitis episode) was used in order to determine the association between some factors and peritonitis episodes. Statistical significance was defined as p <0.05. All statistical analyses were performed using SPSS 13.0.
RESULTS
The rate of peritonitis in all PD patients was found to be 0.22 episode/patient year and 22 (20.18%) of the patients had more than one episode (excluding recurrent and relapsing peritonitis) through the whole follow up period. The peritonitis rate in diabetic PD patients was found to be 0.23 episode/patient year while in non-diabetics the rate was 0.22 episode/patient year (p >0.05). On the other hand, in CAPD patients solely, the rate was 0.22 episode/patient year whereas the one in APD patients was 0.21 episode/patient year (p >0.05).
Twenty seven (24.8%) of the patients were allocated to PD due to obligatory reasons that mainly were loss of arteriovenous access possibility or social problems in reaching the HD unit.
Table 1 shows some demographic properties, comorbidity status and laboratory tests of the patients. The patient population had a high frequency of anti- hepatitis C virus antibody (anti-HCV ab) positivity (26.6%).
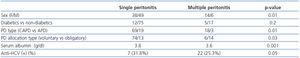
According to multiple regression analysis for the analysis of time to first peritonitis episode, the assosciated factors found were as follows; PD allocation type (p = 0.04; RR = 2.6), serum albumin level (p = 0.05; RR = 1.2), and Anti-HCV Ab positivity (p = 0.04; RR = 1.5). However, sex, diabetes, the type of PD treatment, duration of ESRD, mean haemoglobin level, mean C-reactive protein (CRP) level, Hepatitis B surface antigen (HBs Ag) positivity and mean CCI score were not found to be significantly associated with peritonitis (table 2).
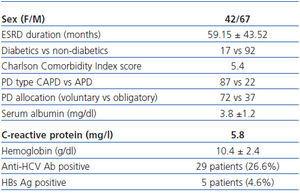
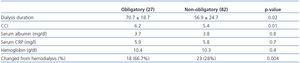
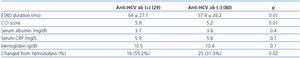
Table 3 shows the differences among patients according to PD allocation type. The different characteristics of patients with or without anti-HCV Ab are shown on table 4.
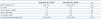
Twenty two patients (20.2%) had more than one episode during the follow-up period. Fourteen of these patients (64%) were females. When patients with single episodes were compared to those with multiple episodes, the percentage of female patients were significantly higher among those with multiple episodes (p = 0.01). Serum albumin level (p = 0.001), type of allocation to PD (p = 0.01) and type of PD treatment (p = 0.03) were also sigificantly different, however the number of diabetic patients was not higher in patients with multiple episodes than in patients with single episodes. The frequency of anti-HCV positivity was not significantly different in patients with multiple episodes when compared with patients with single episodes. The results of comparisons between patients with single and multiple peritonitis episodes can be seen in table 5.
At the end of the follow-up period, 93 (85.3%) patients were still on peritoneal dialysis, 4 (4.3%) patients were referred to hemodialysis, 4 (4.3%) patients died while 8 (8.6%) patients were transplanted.
DISCUSSION
Peritonitis episode rate can vary from region to region and from centre to centre within the same country16,17. The level of our centre was lower than those accepted by European Best Practice (1:24 months) and International Society of Peritoneal Dialysis (ISPD) (1:18 months) Guidelines18,19.
Peritonitis rate in diabetics, whether is higher or not compared to non-diabetics, most of the time, is a matter of debate in the literature6,20,21. But, mostly the finding is towards a higher but non significant difference in the rate of peritonitis in diabetics, same as our finding. Additionally in multivarite regression analysis, we could not show an association between diabetes and (table 2) peritonitis and morever there was no significant difference in terms of diabetes when patients with single and multiple peritonitis episodes were compared (table 5).
Mean level of serum albumin of the patients, determined throughout the whole follow up period was found to be a significant factor associated with peritonitis according to regression analysis (p = 0.05, OR = 1.2). Hypoalbuminaemia relates with a chronic state of inflammation due to renal failure and dialysis but it can also be related to malnutrition and overhydration22. In our study we could not find an association between chronic systemic inflammation, determined by mean serum CRP levels, and rate of peritonitis. Accordingly, the association between hypoalbuminemia and peritonitis we showed, was probably indicating malnutrition to be the associated risk factor for peritonitis. Whatever the reason, it is certain that hypoalbuminaemia is a predisposing factor for peritonitis hence should be fought in PD patients in order to decrease peritonitis incidence23,24.
In a very recent study, obligatory referral to PD was found to be significantly related to higher mortality among PD patients12. In our study we found that obligatory referral is significantly related to higher peritonitis rates (p = 0.04, OR = 2.6). In another recent study, transferring from HD to PD was also found to be a risk factor for peritonitis13. Reasons of obligatory referral such as loss of AV access chance due to long years on HD may indicate more comorbid conditions in this group of patients which was shown in our study such that duration of ESRD, mean CCI score and percentage of patients changed from haemodialysis were significantly higher in patients obligatorily allocated to PD treatment (table 3). However, neither ESRD duration nor CCI score were found to be associated risk factors for peritonitis (table 2). Hence, it should be kept in mind that, lack of motivation of these patients in case of a mandatory referral can lead to problems like peritonitis and hence technical failure, due to reluctance and carelessness in carrying out the PD procedure. In order to understand better, the contribution of each reason for increased mortality, peritonitis and technical failure in these patients, we need to carry out further prospective studies.
We know APD is mainly driven by patient preference as it improves life style of patients. It has also been considered to have an advantage over CAPD in reducing the incidence of peritonitis which have been shown in some studies25-27 whereas in others no difference were found between the two different modalities of PD treatment13,28. In our study, the rate of peritonitis was lower in APD patients when compared to CAPD patients (0.21 episode/patient year vs 0.22 episode/patient year) but the difference was not significant. In multiple regression analysis, type of PD treatment was not found to be a risk factor for peritonitis. We believe, in addition to lesser contact with catheter due to the technic of APD, lower frequency of peritonitis among APD patients may partly be due to increased preference and hence motivation of the patients choosing APD. Following comparison between patients with single episodes with the ones with multiple episodes we found a significantly higher number of CAPD patients in multiple episodes group which may be at least partly due to higher motivation of APD patients. We believe a prospective trial considering motivation of the patients is needed for better understanding the difference in incidence of peritonitis between different types of PD treatments.
The prevalance and seroconversion rates of anti-HCV ab positivity are lower in PD than HD patients which is considered to be an advantage of PD over HD29,30. However, there is no data comparing HCV status to peritonitis in PD patients. In our study, multiple regression analysis reveals anti-HCV ab positivity to be a factor associated with episodes of peritonitis in PD patients (table 2). Patients with anti HCV positivity were on dialysis for a longer period, had a higher CCI score and were obliged to PD treatment more than anti-HCV negative patients (table 4). Probably this obligation was the real underlying associated factor for peritonitis in this group of patients.
The results of statistical analysis of mutiple episodes compared to single episodes showed that serum albumin is significantly lower for patients who had more than one isolated peritonitis episode when compared with patients who had multiple episodes during follow up period (p = 0.001). Patients who had multiple episodes were also allocated to PD mandatorily more frequently than the ones who had single episode (p = 0.01) supporting the findigs in multiple regression analysis. These two factors were consistent with associated risk factors for time to first peritonitis episode strenthening them to be risk factors for peritonitis episodes in PD patients. Morever, as mentioned above, APD patients were less in number in multiple episode group than CAPD patients which might be related to difference in motivation between two dialysis treatment types. Additionally, there were significantly more females among patients with multiple episodes compared to ones with single episode. In our study, sex was not a risk factor for developing peritonitis episodes (p = 0.5). However, female patients were found to have significantly more multiple episodesthan male patients. In several studies female gender is shown to be a risk factor for peritonitis13,31.
In conclusion, mean serum albumin levels in a PD patient is significantly associated with peritonitis and should be closely monitored during follow up. Obligatory referral which can be an indication of loss of motivation for peritoneal dialysis procedures is thought to be a strong risk factor for peritonitis in PD patients and should be further studied. Patients with multiple episodes were more hypoalbuminemic, had a higher frequency of mandatorry referral and they were mostly females when compared to patients with single episode during follow up.
Table 5. Comparison of peritoneal dialysis patients who had single attack with patients who had multiple attacks
Table 2. Multiple regression analysis for factors associated with peritonitis episodes
Table 1. Demographic data, comorbidity status and laboratory data (mean levels) of the patients
Table 3. Comparison of characteristics of patients according to type of allocation to PD
Table 4. Comparison of characteristics of patients according to anti-hepatitis C virus antibody status