La enfermedad renal crónica (ERC) representa uno de los principales problemas de salud pública debido a los altos costes sociales y económicos tanto por su elevada prevalencia como por la morbimortalidad cardiovascular asociada. Existen suficientes evidencias que demuestran que la implementación de modelos de prevención y de seguimiento mejora la evolución y frena la progresión de la ERC reduciendo los costes al mismo tiempo que mejora o se mantiene la calidad en la atención. Se requieren, por tanto, nuevos modelos que manejen de forma integral todos los niveles de la ERC. Aunque existen diferentes modelos de reembolso por parte de las aseguradoras o los gobiernos, tradicionalmente el pago por servicios ha sido el utilizado en los centros de diálisis concertados pagándose por sesiones de diálisis y unos requerimientos mínimos de calidad. Este modelo comporta el riesgo de favorecer la sobreutilización e inducción a la demanda. Sin embargo, cuando se acerca el estadio final de la ERC (inicio de la diálisis), el manejo integral mediante una tarifa comprensiva ofrece ventajas basadas en un principio de equidad, calidad y sostenibilidad. El reembolso se realiza a través de un pago único y completo de un paquete asistencial que cubre los servicios que se han definido previamente. La tarifa se estima con base en la utilización previa de recursos, sin tener en cuenta la prevalencia de la enfermedad. Un tercer modelo es la capitación. Esta ofrece a los proveedores una cantidad fija de dinero para proporcionar servicios a una determinada población durante un tiempo determinado teniendo en cuenta la prevalencia e independientemente del volumen de los servicios consumidos de forma individual. Para evitar la asignación incorrecta de los servicios y productos inducida por incentivos en contención de costes, se establecen requisitos mínimos de calidad de servicio. En nuestra opinión, el modelo de tarifa integral significa una tendencia hacia una mejor coordinación de los servicios concertados en la ERC estadio 5, siendo la financiación capitativa uno de los pilares para fomentar la integración de proveedores y la articulación entre niveles asistenciales.
Chronic kidney disease (CKD) is becoming a worldwide major public health problem that is rapidly approaching epidemic proportions due to its high prevalence, as well as the associated increase of cardiovascular morbidity and mortality in these patients. Early detection and prevention may have an impact on both slowing the progression of CKD and reducing cardiovascular morbidity and mortality. CKD prevention programmes can be more cost-efficient over time without negative impacts on quality of care. Until now, reimbursement in CKD has been segmented and usually focused on the end of the process (dialysis) when cost is higher, whereas new models focused on provider integration, while balancing quality and costs, are needed to respond to today’s challenges. Traditionally, “pay for services” has been used in state-assisted dialysis centres, but this model has the risk of inducing an increase in demand. Integrated management would respond to this challenge with comprehensive solutions that manage kidney disease at all levels of health care risk. It is based on a comprehensive model that typically includes several products and services, often including pharmacological treatments. The rate of reimbursement directly depends on the achievement of previously defined quality control parameters. The third model is based on a “capitation” model that consists of the provider receiving a set amount of resources per population for a particular time regardless of the volume of services provided. The complexity and the progressive nature of CKD along with the associated morbidity rates in these patients force us to consider a global approach rather than a sum of different services. In our opinion, the first method of reimbursement in CKD that should be considered is a bundle rate, and when this model has been consolidated, tending toward a global capitation model.
INTRODUCTION
Our health system is currently facing a crisis. This would appear unlikely when taking into account the extensive efforts made by health care professionals in many different aspects, such as genomic medicine, regenerative medicine, and evidence-based medicine. However, costs continue to rise rapidly, primarily due to demographic changes in the form of a progressively aging population and an increase in the prevalence of chronic diseases, while new technologies and treatments are constantly being developed and put into practice.
One of the circumstances that have provoked this change in the medical care has been the growing incidence of chronic diseases and their impacts. Currently, chronic diseases are responsible for 60% of the 58 million deaths per year worldwide, representing a significant economic cost to society.1 This means that approximately 80% of health care resources in developed nations are used for fulfilling the needs of patients with chronic diseases.2
In Spain, it has been more than two decades since experts foresaw coming issues within the National Health System, and a commission was established to evaluate these problems and elaborate possible solutions.3 The general objectives of this commission were4:
- A progressive introduction of the separation of funding and acquisition of health services (public), and of the functions of health care management and provision (public and private).
- Replacement of the concept of comprehensive health care for one based on the functions of health care authorities and functions based on services provided, with collaboration with the private sector.
- Increased flexibility among health care personnel, that is, a modification of the current regulatory framework that determines employee conditions (respecting worker’s rights).
- Approval of a new legal framework that would allow for certain hospitals and other health care institutions to become state-governed societies with financial and property autonomy subject to private law.
Only a few of these goals have been put into practice during the last two decades, and studies examining this issue have predicted that the current system will become unsustainable by the year 2015 if new models are not established and adopted.5
In this article, we sought to discuss the different models proposed for comprehensive health care for patients with chronic kidney disease (CKD) that attempt to establish a balance between quality of services provided and costs incurred.
CHRONIC KIDNEY DISEASE
CKD represents one of the main public health issues in modern society, both due to its high prevalence and the important associated cardiovascular morbidity and mortality rates, with all of the social and economic costs that this implies.
In 2008, the United States spent 23 billion dollars in the treatment of advanced CKD (ACKD), which represents 7.4% of that country’s health care budget, yet is applicable to only 1.1% of the population.6,7 In 2010, more than 48,000 individuals in our country were on renal replacement therapy (RRT), a statistic that has continued to grow during the last decade due to a progressively aging population and an increase in the prevalence of other chronic diseases, such as diabetes mellitus. The treatment of CKD (0.1% of the population) consumes 2.5% of the Spanish National Health System budget.8 This staggering value has generated widespread doubts about the long-term sustainability of RRT,8-10 as well as a proliferation of articles concerning the costs incurred by different modalities of dialysis.8,10-12 Our group carried out one study13 in patients on haemodialysis that resulted in a mean cost surpassing 40,000 Euros per patient per year.
However, we must keep in mind that CKD is a progressive and irreversible disease in which the patient passes through different phases, RRT constituting the final stage only reached by a small proportion of patients with CKD. However, a large percentage of patients do not reach the stage of RRT, primarily due to cardiovascular mortality.14
With this in mind, CKD represents an ideal scenario for the creation of an integrated health care management plan involving models for the comprehensive treatment of all stages of CKD in the at-risk population.
Such a plan has the potential to act upon different risk levels which are represented graphically in the following figures adapted from Theodore F. Hatch (Figure 1 and Figure 2).
Why is an integrated health care model necessary?
There are several different reasons why integrated health care management is particularly suited for the case of CKD: 1) multiple sources of comorbidity in this population require improved coordination of health care and specific plans for controlling diabetes and cardiovascular disease, 2) high rates of hospitalisation and mortality, which could be reduced with improved outpatient care and prevention-oriented medicine, 3) numerous health care techniques and processes have demonstrated improved clinical results for these patients, and 4) the disproportionately high health care costs for the relatively small population with CKD.15
Several different strategies have been proposed for reducing health care costs in these patients, but options are usually considered individually due to the impacts derived from social barriers,16-18 in addition to the fact that ACKD has traditionally been treated in a segmented and fragmented manner, particularly in end stages, when the risk of high usage of available health care resources is maximum. In order to face the current challenge presented to the provision of health care in our country, we must adopt a comprehensive approach that cares for patients of all three risk levels while achieving an appropriate balance between quality and costs.19 This process must also integrate the entire spectrum of health care provided to patients with kidney disease, ranging from prevention to the management of patients in late stages of disease development.20
Sufficient evidence already exists to demonstrate that the implementation of prevention and follow-up strategies achieves a slower progression of CKD and cost reduction,16,18,21,22 while the quality of health care provided is maintained or even improved. In order to achieve these positive changes, our efforts must be directed towards changing the management and treatment strategies applied to these pathologies.23
Palmer et al.24 demonstrated that a yearly screening programme applied in primary care for the early detection of nephropathies in hypertensive patients with type II diabetes mellitus, based on determining microalbuminuria rates using semiquantitative rapid strip tests, followed by early treatment with nephroprotective drugs (angiotensin receptor blockers) for patients diagnosed with nephropathies, yields improved long-term clinical results in exchange for a minimal initial economic cost.
In addition to obtaining beneficial results for the cost-effectiveness of treatment of diabetic patients, these screening programmes should be applied to hypertensive and elderly patients as well.23,25,26
It is equally important to integrate the patients themselves into the process of managing the progression of their pathology with education and training. Wingard et al.17 observed how the application of a structured programme involving educational strategies for incident patients on haemodialysis, along with an exhaustive effort on the part of health care personnel during the first three months that the patient is on RRT in various specific areas of clinical care, such as control of anaemia, adequate dialysis dosage, nutrition, reduced catheter use, review of medicines prescribed, logistic support, and psychosocial evaluation with appropriate referral to social services, resulted in a significant improvement in rates of hospitalisation and reduced mortality.
Another point of emphasis is the advantages derived from early referral of these patients to a nephrologist. The majority of the results reported from early referrals to nephrologists are based on retrospective studies, with little evidence available based on prospective studies due to the possible ethical conflicts, and yet a systematic review found that inferior results were produced in terms of mortality and length of hospitalisation in patients who were referred to nephrology later in the progression of their disease.27 McLaughlin et al.28 evaluated the economic impacts of early referral (patient creatinine clearance rate = 20ml/min) as compared to late referral using a decision tree (Markov model), observing that early referral resulted in decreased costs, improved survival, a longer interval of life free of RRT, and reduced duration of hospitalisation.
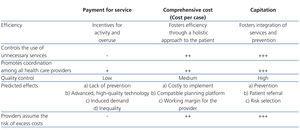
Several different reimbursement models for medical services are used by insurance providers and governments. Table 1 summarises the basic differences between them.
Payment for services is a variable method that assigns resources to the provider based on the amount of services or medical interventions provided. This method may generate incentives for increasing the number of interventions or services provided in order for the provider to receive a greater economic compensation, thus risking over-use of medical resources and over-induction of demand.29 To date, this has been the most common method applied in dialysis centres. Health care authorities pay the provider for the health care services provided, in this case based on the number of dialysis sessions, under minimal quality requirements.
However, in public hospitals, reimbursements generally form only part of the annual budget, which is primarily based on an analysis of budgets from previous years and that, although it can be adjusted based on indicators such as increased prices of goods and services, tends to remain fairly stable and does not allow for a reassignment of resources among different categories of health care services.
A capitation model, in contrast, offers providers a fixed quantity of economic resources based on the provision of services to a predetermined population during a fixed time period, regardless of the volume of services/goods consumed by individual patients. The definition of the different components related to treatment and quality requirements can vary widely.
The capitation model is based on three crucial elements:
This mechanism shifts the economic responsibility of controlling the provision of services within the system to the provider, thus facilitating improved efficiency throughout the fiscal period and fostering preventative measures, improved continuity of health care provided, and a lower consumption of available resources.30
Evidently, the capitation model can be considered as a cost-reducing strategy, thus maximising the profit-based feasibility of the provider business model, although it has the potential for negatively impacting the quality of health care provided. In order to avoid the inappropriate assignment of health care goods and services induced by this incentive, reimbursement models tend to define quality requirements and adopt one of the two following options: fines and punishments applied to institutions that do not comply with quality requirements, or a direct correlation of reimbursement quantities with treatment results.
As such, prospective capitation models strongly promote the following health care policy objectives31:
In the final stages of CKD, when RRT become necessary, integrated health care management based on a comprehensive fee system could offer major advantages based on three basic principles:
Principle of equality
The patient should be free to choose the modality of RRT preferred, within the context of a consensus between the patient and health care professionals (nephrologists, nursing staff, psychologists, and social workers). We have shown how the incorporation of a specific consultation for ACKD into our gamut of health services has contributed notably to facilitating freedom of choice for the patient, with a resulting increase in the rate of patients’ choosing home techniques both in the incident and prevalent population. In this context, the model facilitates state support not just of haemodialysis, but also of any home dialysis technique that the patient might choose.
The nephrologist in charge of the patient will be responsible for giving advice regarding the optimal technique for each particular situation, taking into account both clinical and social factors. In this manner, the patient is free to choose between manual and automated peritoneal dialysis, or from any one of the various haemodialysis options available (low-flux, high-flux, haemodiafiltration, etc.), accompanied by a signed informed consent form. It is common for this effort to be made in hospital care, but this is not always the case for state-assisted patients in real-life situations.
In 2004,32 in the Region of Murcia, reimbursement for using special techniques was granted for the first time (on-line haemodiafiltration and frequent haemodialysis) in state-assisted patients (as many as 20% of all patients). Other autonomous communities followed suit, generating enormous differences in treatments provided between the different geographic regions of Spain.
The new model guarantees the eligibility of all possible treatment options in 100% of cases, both in terms of the type of technique applied and the frequency and number of sessions, thus eliminating any differences between hospital dialysis and dialysis in state-assisted centres in terms of equal access.
Principle of quality
The Cartagena model33 incorporates several novel aspects in terms of traditional dialysis regimens, such as the participation of public nephrologists in state-supported health care and the creation of an oversight committee that will evaluate compliance with each of the established protocols on a trimester basis. This committee is composed of representatives from the Murcia health department, the hospital, the contractor, and the patient association (Association for the Assistance of Renal Patients).
The group of quality indicators includes two components with major impact on vascular access points, one of the biggest issues in modern nephrology. Recently, major differences (52.7%-82.6%) were reported among the different autonomous communities in terms of the percentage of state-assisted patients with an autologous fistula.34 In the current treatment model, the contractor has committed to ensuring that more than 80% of patients on haemodialysis have an autologous or heterologous fistula at any given moment.
In this same manner, a commitment has been made to ensure that 95% of all patients should have a definitive access point within a maximum deadline of 15 days.
Principle of sustainability
The new model35 utilises a fixed cost per patient for each modality of dialysis, with no hidden fees or other surprises for the individual who pays for the health care services, incorporating financial penalties in the case of non-compliance with quality indicators, especially in cases of the greatest economic impact, which can lead to a cessation of the state-assisted health care agreement in the case of recurrent or particularly severe non-compliance.
The final goal is a responsible health care system throughout the entire process, introducing the concept of economic responsibility in the management of all contractors involved. In this manner, compliance with the previously mentioned quality indicators regarding vascular access points would reduce the number of patients who start RRT with a temporary catheter, as well as the global number of catheters placed, with substantial impacts in terms of reducing indirect costs and morbidity/mortality rates.36,37 In health care partnerships in which the contractor assumes the responsibility of the vascular access point, the recommendation should be made, based on national and international guidelines, that the patient be referred by the hospital in stage 4 CKD (glomerular filtration rate: 20-30ml/min) in order to ensure sufficient time for establishing and maturing the vascular access (4-6 months prior to inclusion in a haemodialysis programme in the case of an autologous arteriovenous fistula, and 4-6 weeks for prosthetic fistulas).38
The combination of all of these elements of equality, quality, and sustainability define the Cartagena model of integrated health care, under the concept shared with De Francisco9 that efficiency cannot be prioritised at the expense of quality in the health care provided.
To conclude, we need imaginative responses for dealing with the double threat facing the public health care system in the form of the economic crisis and increasing prevalence of chronic diseases that consume large quantities of health care resources. We should search for strategies for early detection and prevention of CKD, as well as secondary prevention measures for progression towards advanced chronic kidney disease, since both processes would have considerable economic impacts on the budget available for health care. In this article, we have reviewed some of the public-private collaboration models that can be applied to the situation of CKD and RRT, which in our opinion do not contradict with, but rather provide an opportunity for collaboration with other initiatives for improving the quality of health care services provided, such as clinical management models that demand efficiency among health care professionals. In the first stage of implementation, the integrated Cartagena model of reimbursements could signify a tendency towards improved coordination among health care partnerships responsible for treating stage 5 CKD. After this process yields an appropriate framework for improved collaboration, the capitation financial model could come to constitute an optimal regulatory pillar for the development of integrated services from health care providers and coordination between the various levels of the health care system.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Differences between the different models of reimbursement for medical services
Figure 1. Level of severity/degree of costs
Figure 2. Level of severity/type of intervention/degree of costs