To the Editor,
Diabetes mellitus (DM) is a common cause of kidney failure (KF), but this pathology is not the only aetiology in diabetic patients presenting with renal failure.
We present the case of a 62 year old man with a history of arterial hypertension (AHT), duodenal ulcer, acute myocardial infarction (AMI) and type 2 DM, diagnosed in 2007.
In February 2008, he was admitted to the internal medicine department with pyelonephritis with acute KF (MDRD 21 ml/min), which were interpreted in the context of the infection which was made worse by taking non-steroidal anti-inflammatory drugs (NSAIDs), and continued on discharge. In September 2008, he was referred to the nephrology department presenting with grade 4 KF (MDRD 13.83 ml/min), proteinuria of 5 g/24 h, and persistent microhematuria (negative urine cultures and negative cytology for malignancy). Of note in the rest of the analysis were: Negative ANA, ANCA, and Anti-GBM. Immunoglobulins, light chains, complements, and proteinogram were normal. Blood cultures for HCV, HBV, and HIV were negative. Abdominal ultrasound: kidneys of normal size with moderately cortical echogenicity with no evidence of dilation of the excretory tract. Normal ocular fundus.
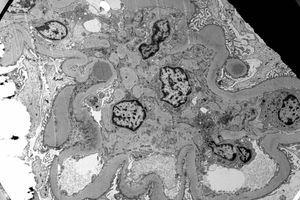
In view of the rapid evolution of the KF, without a clear aetiology being known, a kidney biopsy was performed which revealed 21 glomeruli, 6 of them sclerotic and the rest with glomerular mesangial expansion. A crescent formation was observed in one of these. Thickening of the tubular basal membrane and moderate interstitial inflammatory infiltrates was seen, with a predominance of plasma cells, polymorphonuclear neutrophils, and lymphocytes. Immunofluorescence was negative. An electronic microscope showed diffuse thickening of the glomerular basal membrane with the presence of subepithelial electron-dense deposits forming the typical humps (Figure 1).
This finding lead to a diagnosis of post-infectious glomerulonephritis (PIGN) complicating a nephropathy.
Figure 1. E.M: Postinfectious GN. Presence of subepithelial electron-dense deposits (humps)