Dear Editor,
The association of nephrotic syndrome that was presented with IgA nephropathy (IgA-N) and malignancy has been previously reported.
IgA –N was first described by Berger and Hinglais in 1968. It is now generally known to be the most common cause of primary glomerulonephritis worldwide and is characterized by mesangial proliferation and deposition of IgA.1 Malignancies that have been reported to be associated with IgA-N include Hodgkin’s disease,2 and non-Hodgkin lymphoma3 renal cell carcinoma,4 cancers of the lung,5 larynx and esophagus.6
We report a case of IgA-N presented with the recurrence of gastric adenocarcinoma in a 58 year-old patient.
CASE REPORT
A 58 year-old man admitted to our hospital in September 2010 with distension of the abdomen and involuntary loss of his %10 weight in the last three months. There were no abnormalities in urine examination on the first evaluation. Upper gastrointestinal endoscopy showed gastric mass and endoscopic biopsy revealed gastric adenocarcinoma. Since diagnosed with stage 3B gastric adenocarcinoma, the chemoradiotherapy (4 cycles of 5-fluorouracil and folinic acid with 50 Gy radiotherapy) was administered after the surgery. Complete remission was achieved and he has been considered for follow-up with three months interval without chemotherapy. He was admitted to our hospital with dyspnea and edema in January 2012. Hypoalbuminemia and 4 gram proteinuria was revelaed in laboratory examination. PET-CT scan was showed pleural effusion, bone metastasis and recurrence in mediastinal and abdominal lymph nodes. Then he was considered recurrence of the disease and reevaluated as stage 4 gastric adenocarcinoma. According to his performance status, chemotherapy was not considered and he was referred to our nephrology department for nephrotic syndrome. His blood pressure, temperature and pulse rate were normal. Physical examination revealed decreased breath sound over the right and left lower lung areas and severe edema in both lower extremities. Routine laboratory tests showed the following: serum levels of sodium 137mmol/L, potassium: 5.8mmol/L, calcium: 7.6mg/dL and phosphate: 2.9mg/dL. Blood urea nitrogen (BUN) 22mg/dL, serum creatinine 1.5mg/dL, serum albumin 1.4g/dL and hemoglobin 11.8g/dL. Liver function parameters were within their normal limits. Urinalysis showed urine red blood cells (RBC) counts were >100/high power field, and urinary protein excretion was 3.5g/day. Antinuclear antibody, anti-DNA, anti-streptolysin O, anti-neutrophil cytoplasmic antibody, anti-glomerular basement membrane antibody, anti-HBs, and anti-HCV were all negative. Complement factors C3 and C4 were within normal ranges. Serum and urine protein electrophoresis were negative for monoclonal gammopathy. The peripheral blood smear was normal with no schistocytes.
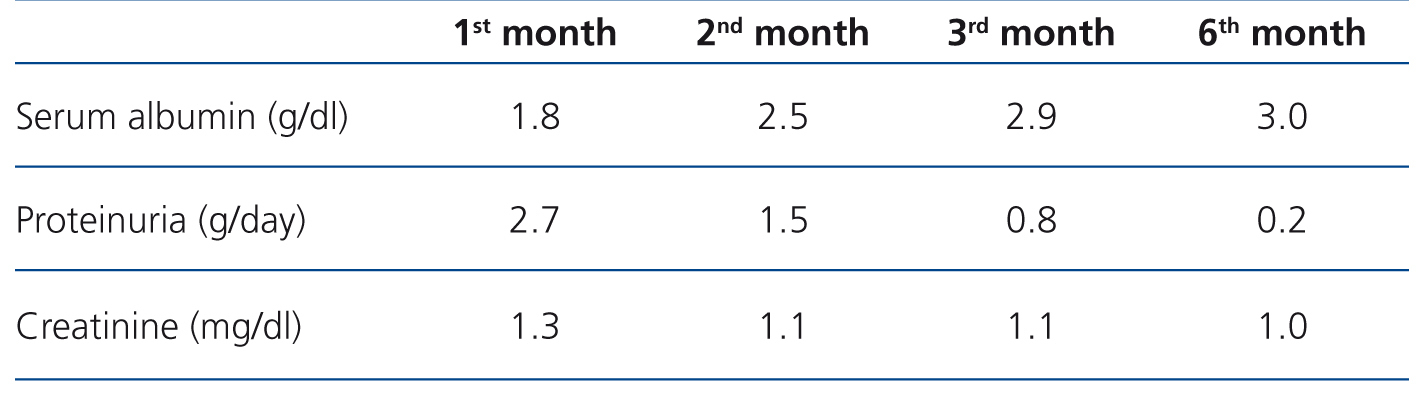
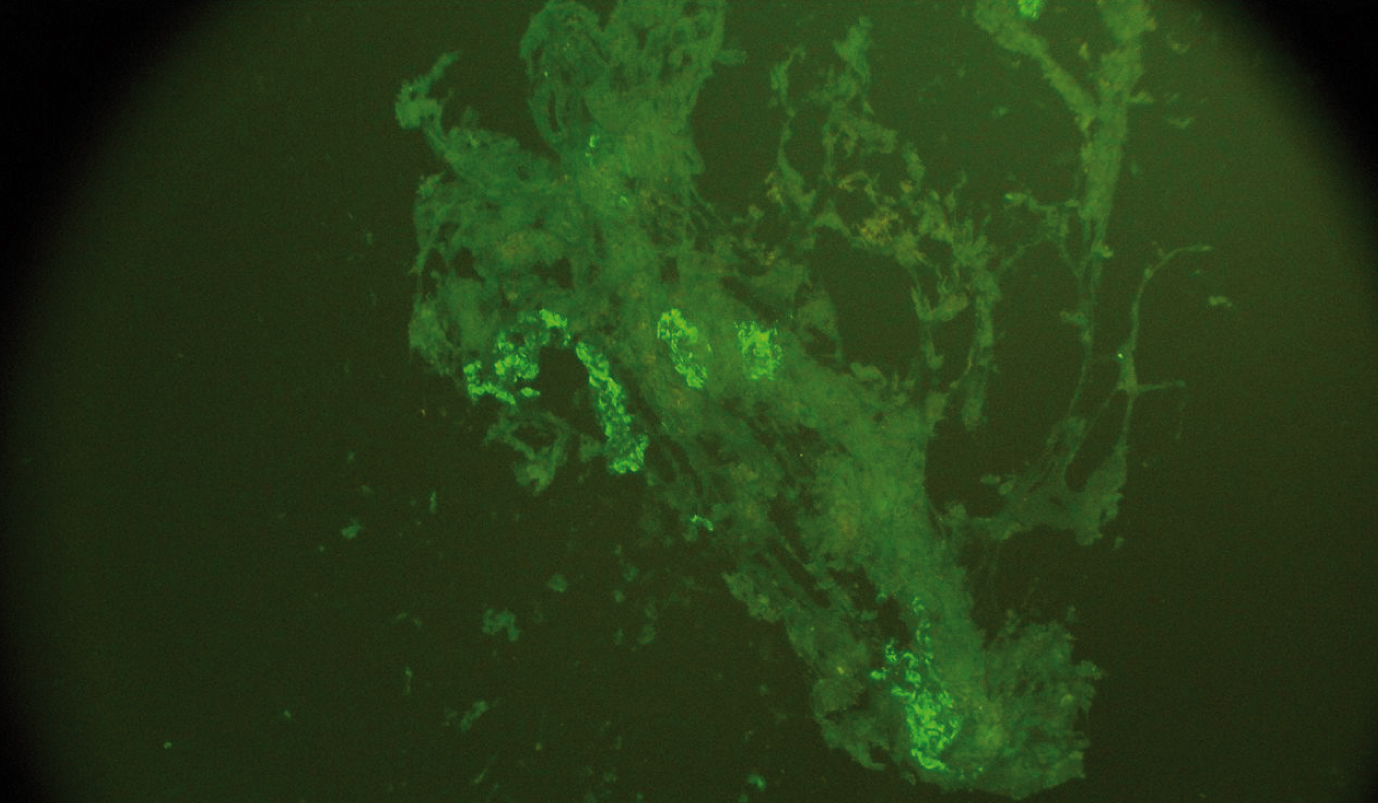
Renal biopsy was performed and in total 14 glomeruli were obtained and evaluated. Light microscopy showed that one of the glomeruli had global sclerosis and other glomeruli had mesangial proliferation. Immunohistochemically, focal segmental mesangial IgA deposition was seen in three glomeruli (Figure 1). Steroid therapy with 1mg/kg/day metilprednisolone and losartan 50mg/daily were started and steroid dose was reduced gradually. After six months later, edema was completely regressed and serum albumin level was 3.0dL. Additionally, urinalysis showed only 1-2 RBC and proteinuria was 0.2g/day (Table 1).
DISCUSSION
Malignancy associated nephrotic syndrome has been described in the literature by Lee et al. reported that nephrotic syndrome occurring simultaneously with malignancy was 10 times higher than in the general population.7
Paraneoplastic syndrome may be suspected in the presence of the following criteria: (a) no evident etiology for the associated syndrome; (b) the diagnosis of the syndrome and cancer simultaneously; (c) clinical (and histological) remission after full remission achieved by chemotherapy or complete surgical removal of the tumor; (d) increases of associated symptoms with tumor recurrence.1
Different types of glomerulopathies, generally membranous glomerulonephritis have been associated with solid tumors.8 However paraneoplastic IgA-N has been reported rarely.
Primarily, IgA-N associations with cancer of the buccal cavity, the nasopharynx and the respiratory tract have been described. Mesangial IgA deposits have been found at autopsy in patients who died of a gastro-intestinal neoplasia without prior clinical evidence of nephropathy.9 Despite intensive investigation, the mechanism underlying glomerular IgA deposition in IgA nephropathy has not been clarified.10 There are two isotype subclasses of IgA: IgA1 and IgA2. Gastrointestinal and respiratory tracts plasma cells produce both IgA1 and IgA2; however plasma cells in the spleen, lymph nodes and bone marrow produce predominantly IgA1. Invasion of the intestinal mucosa by malignancy increases the circulating IgA level and therefore leads to the formation of mesangial deposits.10
In conclusion, paraneoplastic IgA nephropathy with nephrotic syndrome could be a clinical problem in patients with malignancies, besides the treatment chart has not been well-decumented yet. To the best of our knowledge, we report the first case of paraneoplastic IgA-N associated with recurrence of gastric adenocarcinoma. IgA-N should take into account in patients with malignancy and nephrotic syndrome even if primary disease was on remission and it could be a harbinger for the relapse of disease.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Change in serum albumin, creatinine and proteinuria levels after treatment at different times
Figure 1. Focal segmental mesangial IgA deposition in three glomeruli.