The history of home haemodialysis (HHD) is the history of haemodialysis (HD) itself. In the nineteen-fifties and the start of the nineteen-sixties, the artificial kidney technique successfully used for the first time at the end of World War II by Dr Kolff was perfected and with the advent of the autologous fistula reported by Cimino and Brescia, the first HD programmes could be created as treatment for advanced chronic kidney disease (CKD). Due to the unavailability of adequate hospital facilities and with the idea of treating as many patients as possible, these programmes brought HD to the home. As such, HHD saved many lives in this first stage, with the programmes led by Shaldon in London, Merill in Boston and Scribner in Seattle being notable. Subsequently, HHD continued to grow and reached its peak at the start of the nineteen-seventies at which point 40% of US patients used this method. From this period onwards, we have witnessed a progressive decline for different reasons, amongst which we must highlight the increase in the number and morbidity and mortality of patients, the development of peripheral HD units and changes in the financing policy. Furthermore, at the end of the nineteen-seventies and the beginning of the nineteen-eighties, peritoneal dialysis (PD) was developed, a new dialysis method that simplified the technique and also allowed it to be performed at home.
HHD began a gradual decline until the mid-nineteen-nineties, in which there was renewed interest due to the limitations observed in improving morbidity and mortality in kidney patients on conventional HD regimens of three sessions per week. New, more frequent and longer forms of HD had begun to be explored with the aim of avoiding long interdialysis periods, and in order to make this more sustainable from the financial point of view, it was brought to patients’ homes with more frequent dialysis being undertaken in hospital only when indicated by doctors in order to improve some comorbidities.
DEFINITION. CURRENT SITUATION
The term HHD includes the part of renal replacement therapy that refers to extracorporeal clearance carried out by the patients themselves in their own home. There are different regimens1, including:
- Short daily dialysis (2.5-3 hours, 5-6 days a week).
- Frequent nocturnal dialysis (6-8 hours, 5-6 days a week).
- Conventional regimens (4 hours, 3 times a week or on alternate days).
In Spain, the rate of HHD is currently low, accounting for only 0.3% of the total dialysis patients (although the real figure is unknown, since there are no records in this regard). By contrast, the prevalence of the technique has always been high in Australia and New Zealand (9.1% and 19% respectively of total dialysis) with there being a progressive increase in Northern European countries such as Denmark (5.7%), Finland (53%), the Netherlands (2.7%), Sweden (3.4%) and the United Kingdom (4%), where there are great efforts to develop it. Canada should also be highlighted, with a prevalence of 3.9% and from which there has been a large quantity of scientific publications, and the United States (1.3%), with high growth since 2002 due to changes in the Medicare financing policy2. Although the overall figures continue to be very low, recent growth has been very high and a greater development of the technique is expected over the coming years, with a progressive growth in the incidence and prevalence of patients2-4.
ADVANTAGES OF HOME DIALYSIS
The purpose of any renal replacement technique is to obtain the best morbidity and mortality rates with the best quality of life possible. HHD favours the prescription of more frequent HD, with the patient being administered an overall higher dose of dialysis with a lower cost than if this were to be carried out in a hospital, as well as avoiding unnecessary travel and long waiting times, with the inevitable benefits for their quality of life. Various studies have demonstrated many beneficial effects related to the increased frequency of HD, with the following being notable:
- Better control of uraemic toxins, with better tolerance in the sessions, eliminating the post-dialysis fatigue syndrome5-8.
- Better control of anaemia with a lower dose of erythropoiesis-stimulating agents5,6.
- Better control of mineral and bone disorders associated with CKD with a lower dose of chelating agents7-9.
- Better control of nutritional parameters10-13.
- Better control of blood pressure with a lower dose of antihypertensive drugs, facilitating the control of dry weight and maintenance of residual renal function5,8,14,15.
- Improvement in cardiological parameters such as a reduction of left ventricular hypertrophy5,8,14,15.
- Improved quality of life parameters11,16,17.
- Lower morbidity and mortality18-22.
- Reduced costs23-25.
In summary, increasing the frequency of HD makes it more physiological; and using it at the patients’ homes allows them to adjust their pathology to their own lifestyle, avoiding travel. Distance is a factor that facilitates home techniques, but large urban areas are also eligible for obtaining the clinical benefits of these techniques, and therefore the degree of urbanisation is not a barrier26-28. There is no doubt that the home dialysis techniques that enhance self-care offer additional advantages to patients. It has been noted that the two existing techniques, HD and PD are not competing with each other; on the contrary, they enhance one another and where there is more HHD there is more PD, and vice versa.
Most studies that support the advantages of HHD are observational and there are currently no randomised prospective studies. As such, the National Institute of Diabetes and Digestive and Kidney Diseases developed the Frequent Hemodialysis Network, which is a follow-up study of Canadian and US patients over 12 months between March 2006 and May 2009, in which two patient groups were studied. In the first study, 245 patients treated with HD 3 times/week in the hospital (2.5-4 hours, with eKt/V greater than 1) were analysed versus 6 times/week in the hospital (1.5-2.75 hours); and in the second, 87 patients treated with HD 3 times/week in the hospital (2.5-4 hours, with eKt/V greater than 1) were studied versus nocturnal HD at home 6 times/week (6-8 hours). In the first section of the study, after 12 months of treatment, a reduction in the left ventricular mass 16.3±35.3g (p<.001) was observed, as well as an improved Physical Health Composite Score of 3.3±8.9 points (p=.004), better blood pressure control and better control of hyperphosphataemia in the daily HD group, in addition to the need for more interventions in vascular access in this group. The authors concluded that short daily HD is better than a conventional HD regimen8. In the second section of the study, after 12 months of treatment, the patients treated with nocturnal HD compared with HD three times per week did not show significant differences in the primary objectives that included death and reduction of the left ventricular mass, but they did show significant differences in the secondary objectives of blood pressure and hyperphosphataemia. In this instance, it was also necessary to increase the actions on vascular access in the nocturnal HD group. As such, the authors concluded that frequent nocturnal HD was not superior to the conventional regimen29. However, upon analysing this second section of the study, it was confirmed that only 33% of the statistical power was achieved since only 87 patients were randomised due to difficult recruitment, and as such, it was not easy to randomise nocturnal home against hospital (two radically different dialysis methods). Of these, only 78 completed the study, and therefore the statistical power was further reduced. There was also greater inequality in frequent nocturnal incident patients and 25% on the nocturnal regimen received fewer than 5 sessions of dialysis per week.
Given the problems in carrying out randomised studies, subsequent efforts have focussed on comparing large international cohorts. In this regard, the study by Nesrallah22 is notable, which compared French, Canadian and US patients during the period between 2000 and 2010 comparing data from the IQDR (International Quotidian Registry), which included 338 patients (treated 4.8 sessions/week, 7.4 hours/session) compared to 1388 patients of the DOPPS (Dialysis Outcomes and Practice Pattern Study) (treated 3 sessions/week, 3 hours/session). Mortality of 6.1% in the first group and 10.5% in the second group was observed (hazard ratio 0.55, confidence interval 0.34-0.87). The same working group, on this occasion led by Dr Suri30, compared 318 IQDR patients in the hospital (5.8 sessions/week, 15.7 hours/week) with 575 DOPPS patients in the hospital (3 sessions/week, 11.9 hours/week). In this case there was higher mortality in the daily HD group. However, the authors themselves indicate that, despite the efforts made to eliminate confounding factors, other factors as important as residual renal function, the severity of the comorbidity and blood pressure were not assessed. Furthermore, data related to vascular access (more prosthetic fistulae in the daily HD group) were lost and the reason for transfer to an intensive regimen was not analysed.
INDICATIONS AND CONTRAINDICATIONS FOR HOME HAEMODIALYSIS
HHD is a technique that may be used by very diverse age groups from young patients with an active working life who would be able to improve their time management, to older patients with major comorbidities, for whom this technique could allow them to stay at home in the final stage of their life. As such, the liberalisation of medical criteria maintains the good clinical results of HHD31, further improving the quality of life of patients32. With this aim, the American group Medical Education Institute has developed the MATCH-D selection criteria for HHD patients, which in its 2013 version presents three groups of selection criteria that allow patients to be categorised into three different recommendation statuses for the technique.
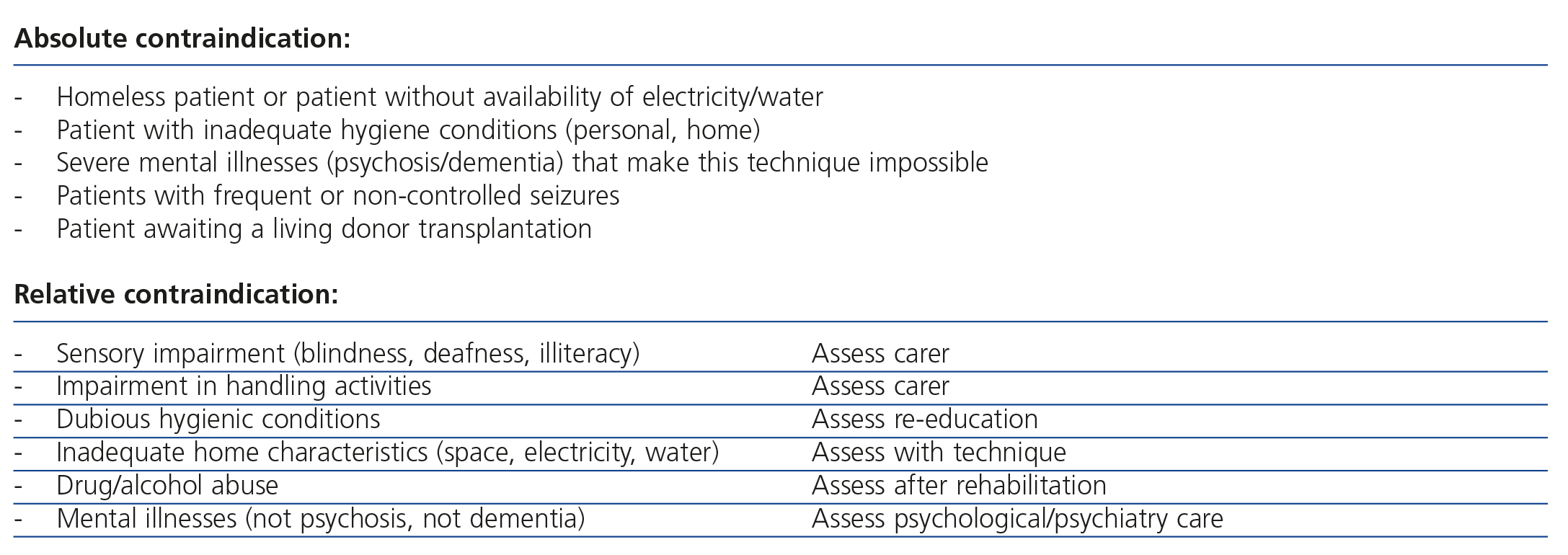
We consider that in HHD, liberal and objective criteria must be used to select patients, providing information to all those who are not absolutely contraindicated and attempting to assess the elimination of potential barriers in order to perform the technique, when these exist. Table 1 displays the absolute and relative contraindications that currently must be taken into account when considering whether a patient is a candidate or not for HHD.
Vascular access must have characteristics that make its objectives easy to achieve, i.e. obtaining sufficient flow for HD. A native fistula is preferable to a prosthetic fistula and the latter is preferable to a permanent catheter34. The presence of a temporary catheter would be a contraindication for this technique until permanent access is obtained. If it is impossible to cannulate the native fistula, this is not a contraindication for the technique. In this instance, if self-puncture is not possible, we should try to use techniques that facilitate it, such as the Buttonhole technique1. If this is not possible, we should assess the insertion of a permanent catheter, although in this case the patient must be made aware that the use of a central venous catheter increases the risk of infection and the associated morbidity and mortality35,36.
SPANISH SOCIETY OF NEPHROLOGY HOME HAEMODIALYSIS GROUP
It may be that in Spain, given the low current use of HHD, in which there are few patients per hospital and they are far from one another, attempts must be made to join efforts and experiences in order to increase its use. The final objective of the group is to increase this technique in our country, being convinced that it can be very beneficial for a certain group of patients. As such, we are considering a series of short- and medium-term objectives that may help to achieve the final objective. These would be the following:
- Knowing the real HHD situation in Spain by creating a patient registry.
- Knowing the barriers that impede its development and promoting its use.
- Carrying out multicentre studies in the field of HHD.
- Creating scientific documentation of interest on HHD (reviews, guidelines, etc.).
- Promoting knowledge and sharing with patients and healthcare professionals the benefits related to its use, in order that HHD may be a real therapeutic option.
- Contacting other international societies that have promoted the development of this technique.
In this regard, on 30 June 2014, the Governing Board of the Spanish Society of Nephrology (S.E.N.), approved the creation of the working group. We face many challenges ahead that we will attempt to address, since we consider that we cannot continue with a minimum incidence in the technique without offering this method of treatment to our patients. HHD is a good dialysis technique with great advantages for the patient, which allows it to be used daily at a reduced cost and which is being implemented in other countries in our setting on a large scale. Although in Spain the rate of use is low, we believe that this working group can change the panorama over the coming years. We invite all members of the S.E.N. who are interested in this technique to participate in this group by contributing their ideas and experience.
Conflicts of interest
The authors declare the following potential conflicts of interest.
They receive fees for lectures.
Table 1. Contraindications for home haemodialysis