Introducción: La peritonitis es una de las complicaciones más frecuentes y graves asociadas a la diálisis peritoneal (DP), siendo la primera causa de pérdida de catéter y de finalización de la técnica. La incidencia y etiología de cada episodio varía en función de cada región y evoluciona a lo largo del tiempo. Por esta razón, es de vital importancia conocer los factores de riesgo y pronósticos de peritonitis en cada momento. Métodos: Se realizó un estudio observacional de cohorte, multicéntrico, prospectivo, con un seguimiento máximo de 7 años (2003-2010) que incluyó 1177 pacientes, con 476 episodios de primera peritonitis (total: 1091 peritonitis). Resultados: Se presenta la descripción de las características del primer episodio de peritonitis en una serie amplia y actual. Los factores que se asociaron a un menor tiempo hasta la primera peritonitis en análisis multivariante fueron la comorbilidad cardiovascular previa (hazard ratio [HR] 1,25 [1,04-1,58]), la procedencia de hemodiálisis (HR 1,39 [1,10-1,76]) o trasplante renal previo (HR 1,38 [1,10-1,93]), iniciar DP con técnica manual (HR 1,39 [1,13-1,73]) y la edad de inicio > 70 años (HR 1,53 [1,23-1,90]). El primer episodio de peritonitis presenta una tasa de recidiva del 7,8 %, retirada de catéter del 11,7 % y una mortalidad en el primer mes tras el episodio del 1,3 %. La evolución de la peritonitis depende fundamentalmente del tipo de germen. Se estima un riesgo mayor para gramnegativos (odds ratio [OR] 5,31 [2,26-12,48]) y el agregado de peritonitis polimicrobianas, por hongos o por micobacterias (OR 38,24 [13,84-105,63]), comparados con la referencia de grampositivos. Conclusión: El desarrollo del primer episodio de peritonitis depende de las características del paciente al inicio de diálisis, la comorbilidad y la técnica utilizada. Los pacientes que presentan mayor riesgo deben recibir una atención especial en los procesos de entrenamiento y seguimiento.
Introduction: Peritonitis is one of the most common and severe complications associated with peritoneal dialysis (PD), constituting the primary cause of catheter loss and exit from the dialysis technique. The incidence and aetiology of peritonitis episodes vary based on geographical region, and change over time. For this reason, it is vital to maintain an updated understanding of the current risk factors and prognostic factors associated with peritonitis. Method: We performed an observational, multi-centre, prospective cohort study with a maximum follow-up period of 7 years (2003-2010), which included 1177 patients and a total of 476 first episodes of peritonitis (total: 1091 cases of peritonitis). Results: We describe the characteristics of the first episode of peritonitis from a large and current study sample. The factors associated with a shorter interval until the first episode of peritonitis as selected by the multivariate analysis included prior cardiovascular comorbidity (Hazard Ratio [HR]: 1.25 [1.04-1.58]), having previously received haemodialysis (HR: 1.39 [1.10-1.76]) or a kidney transplant (HR: 1.38 [1.10-1.93]), having started PD on a manual modality (HR: 1.39 [1.13-1.73]), and initial age >70 years (HR: 1.53 [1.23-1.90]). The first episode of peritonitis was associated with a 7.8% rate of recurrence, an 11.7% rate of catheter removal, and a mortality rate within one month of the episode of 1.3%. The progression of peritonitis infections depended on the type of causal microorganism. We calculated a greater risk for gram-negative bacterial infections (Odds Ratio [OR]: 5.31 [2.26-12.48]) and the aggregate group of infections caused by multiple microorganisms, fungal infections, and mycobacterial infections (OR: 38.24 [13.84-105.63]), as compared to gram-positive bacterial infections. Conclusion: The development of a first case of peritonitis depends on the characteristics of the patient starting dialysis, comorbidities present, and the technique used. Patients at a greater risk for peritonitis must receive special care during training and follow-up.
INTRODUCTION
Peritonitis is one of the most common and severe complications associated with peritoneal dialysis (PD), and is the primary cause of patients leaving this form of treatment.1 Peritonitis in patients on PD is associated with an estimated mortality rate of 1%-6%, according to different studies.2-4
An understanding of the prevalence and incidence of infectious complications, as well as the risk factors associated with them, can aid in establishing adequate preventative measures and treatment options. The risk factors associated with the appearance of peritonitis described in previous studies include: age, race, diabetes mellitus (DM), elevated body mass index, nasal carriage of Staphylococcus aureus, prior antibiotic treatment, and hypoalbuminuria.5,6
The incidence and characteristics of peritonitis cases vary by geographic region and also shift over time.7 This makes it especially important to continuously monitor the population, with periodical assessments that allow us to access an updated database in the context of predicting future patterns of peritonitis. Registries have reported a progressive decrease in the rates of peritonitis as improvements have been made to connection systems and strategies for training patients in proper use. However, most studies involving PD take into account peritonitis in general, and do not analyse the first episode as a singular entity with specific characteristics. This first episode determines hospitalisation rates, may delay transplantation, presents a hindrance to the use of PD free of infection, and can affect both the survival of the peritoneal membrane as a useful medium for dialysis and the survival of the patient.
In this study, we sought to describe the characteristics and evolution of the first episode of peritonitis in patients on PD, as well as associated risk factors, in a population corresponding to a specific geographic area of Spain.
MATERIAL AND METHOD
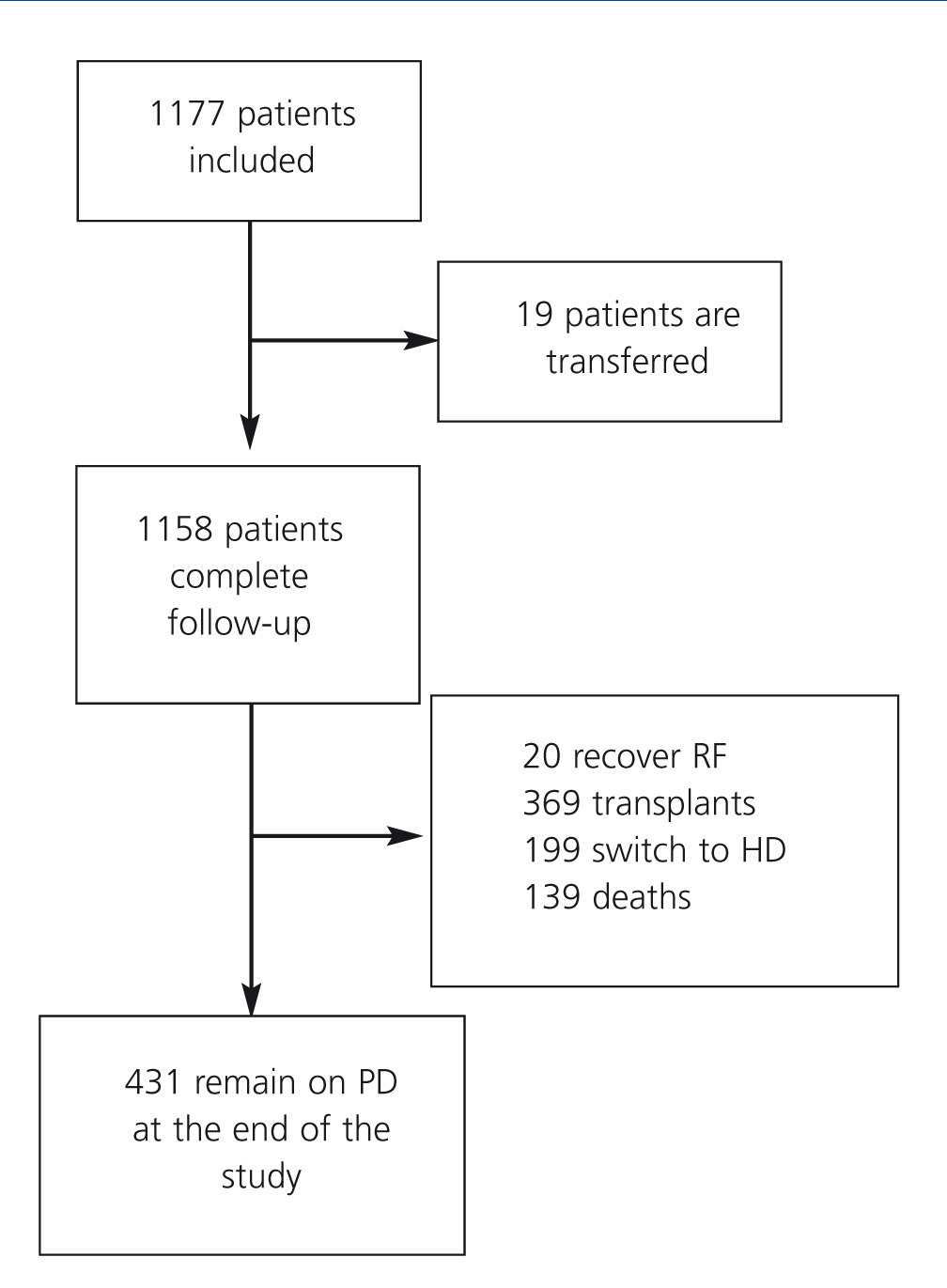
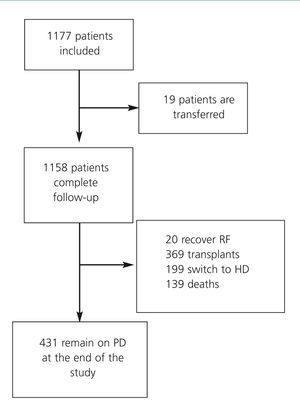
We performed an observational, multi-centre study among incident adult patients on PD (from January 2003 to January 2010) in the Peritoneal Dialysis Centre Group, composed of 22 public hospitals in central Spain, which is responsible for the treatment of 8.8 million inhabitants. In our country, PD is a treatment that is covered by the national health system, and so we have included all adult patients who started PD during this period, with an exhaustive follow-up regimen until the end of the study (Figure 1). All patients on continuous ambulatory peritoneal dialysis (CAPD) used double-bag systems, and patients on automated peritoneal dialysis (APD) used luer-lock connections to the cycler. We included baseline values for demographic parameters, aetiology of the chronic kidney disease, original treatment (haemodialysis [HD], transplant, or new treatment), free choice or required entry into PD, and comorbidities (Charlson index).8 Clinical events (peritonitis, hospitalisations, change in the renal replacement therapy [RRT] technique used, and deaths) were recorded at the moment they occurred. In addition, clinical and laboratory values were compiled twice per year as described previously.9 We considered cardiovascular comorbidities (CV) to be any major CV event prior to the start of PD: myocardial infarction, coronary revascularisation, major amputation due to peripheral ischaemia, initial status of heart failure with functional grade 3 or 4 on the NYHA (New York Heart Association) scale, or stroke.
A first episode of peritonitis was defined as the first case in which cloudy peritoneal fluid was observed, with a leukocyte count equal to or greater than 100 cells/mm3, and with >50% polymorphonuclear cells. For each episode of peritonitis, we also recorded the number of days elapsed until the leukocyte count fell below 100 cells/mm3. We also included information regarding concomitant infections of the exit site, placement and duration of the tube, and the final result of the episode (resolution, recurrence, catheter removal, or death). We considered deaths to be secondary to the peritonitis whenever this was expressly declared as the patient cause of death or when the patient died within 30 days of diagnosis of the episode. Hospitalisation was defined as a hospital stay >24 hours in duration, which excluded urgent treatment of peritonitis in the emergency department.
All data were compiled in an anonymous database, with no information stored regarding the commercial companies who supplied treatment materials for the patients. The design, management, and analysis of the database were all approved by an independent scientific committee and were monitored by a data manager who compiled and filtered the data twice a year. All patients signed an informed consent form for inclusion on the treatment regimen. All statistical analyses were performed using SPSS statistical software, version 11.0.
Results for numerical variables were expressed as mean and standard deviation (SD). Based on the type of variable to be compared, we used Student’s t-tests, ANOVA, or Χ2. We also performed a univariate logistic regression to calculate the odds ratio (OR) for each prognostic factor in the progression of the first episode of peritonitis, followed by a multivariate model that incorporated all variables that resulted in a P-value of <0.10, in addition to all clinically relevant variables. The final model chosen was that which was simplest and yielded the maximum R2 value. We used the Kaplan-Meier test (KM) and a Cox regression model to analyse the time interval until the first episode of peritonitis. These results were expressed as median estimated time until the first episode of peritonitis, and as hazard ratios (HR) for the Cox regression analysis, along with 95% confidence intervals. For the Cox regression model, we used a backwards step-wise procedure, in which we included all variables with clinical and/or statistical significance from the prior univariate analysis.
Sample processing and protocols used for peritonitis
We treated all patients with antibiotic prophylaxis prior to placement of the peritoneal catheter. Patients were also tested for Staphylococcus aureus carriage, and those with positive results were given antibiotics. Peritoneal fluid samples were tested according to the recommendations by the International Society of Peritoneal Dialysis (ISPD).10,11 At three of the participating centres, patients were authorised to start empirical antibiotic therapy in an ambulatory context in the event of a strong suspicion of an episode of peritonitis, and instructed to reserve samples of the peritoneal fluid for testing. Empirical antibiotic therapy protocols were adjusted based on culture results, antibiotic resistance, and previous experience. The empirical treatment of choice was vancomycin and ceftazidime (or aminoglycoside) in 19 centres, cefazolin and aminoglycoside in two,10 and cefazolin and ceftazidime.11
Patient sample
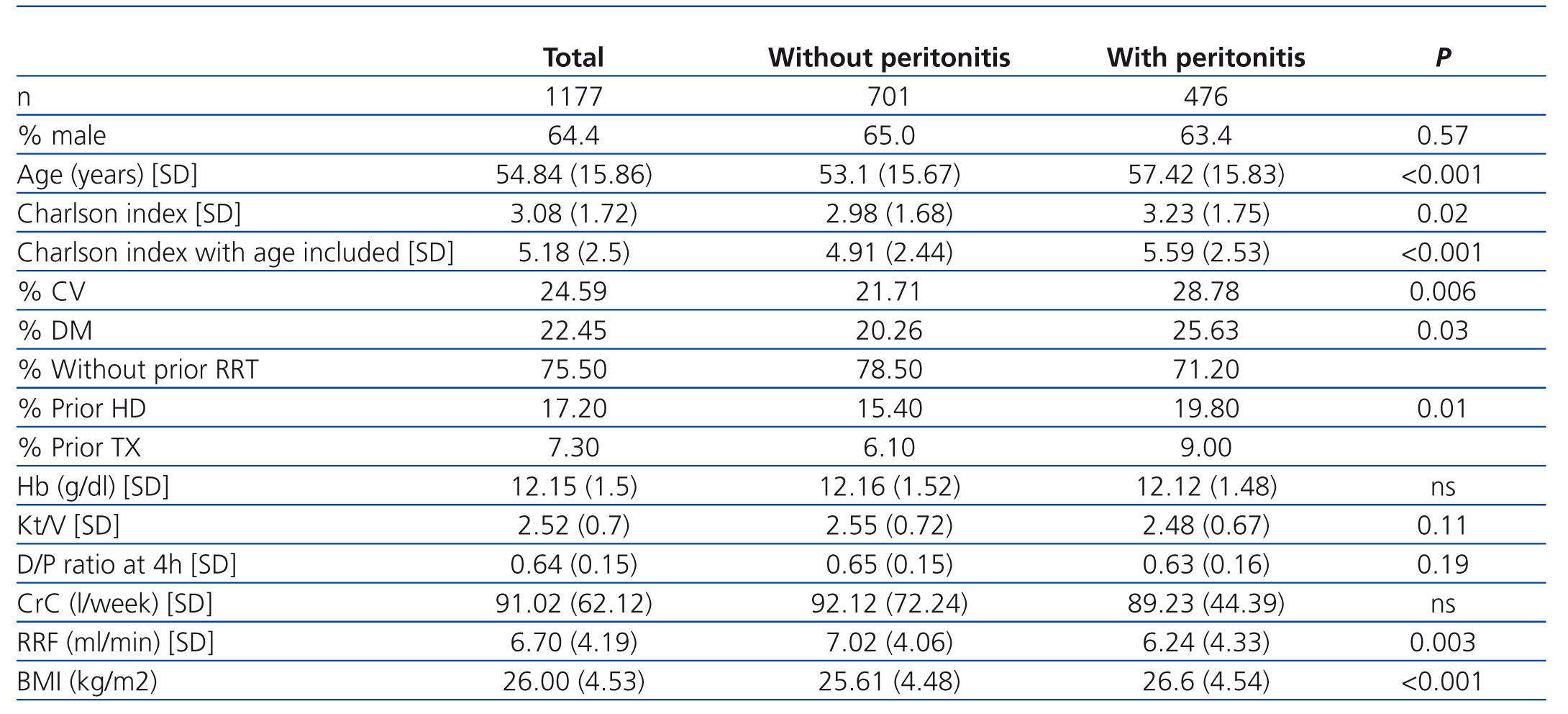
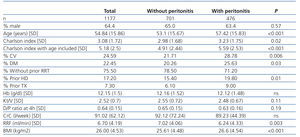
This analysis included a total of 1177 incident patients on PD treated between 2003 and 2010, of which 1158 completed the follow-up period. The most important characteristics of the patient sample are summarised in Table 1: mean age: 54.84 years (SD: 15.9), with a median of 56 years; 64.4% of the study population were males. At the start of PD, 22.5% were diabetic and 24.6% had suffered at least one CV event, with a mean age-adjusted Charlson index value of 5.18 (SD: 2.5).
As far as patient origin, 17.2% came from HD, 7.3% had received a kidney transplant (TX), and 75.5% were starting PD as their first experience on renal replacement therapy. In terms of the PD technique used initially, 812 patients started on manual techniques, constituting 69% of the total, and the remaining 31% started on automated techniques.
We examined the initial situation of the patients in our sample as a starting point for study values. Mean residual renal function (RRF) one month after starting PD was 6.7ml/min (SD: 4.2), with a mean Kt/V of 2.5 (SD: 0.7), and a mean creatinine clearance value of 91 litres/week (SD: 62.1). In addition, 80.1% of patients had a haemoglobin (Hb) value >11, and the mean initial Hb value was 12.2g/dl (SD: 1.5). Finally, 10.8% of patients had a dialysate/plasma creatinine ratio at 4 hours higher than 0.81 at the start of PD treatment, classifying them as high transporters.
At the end of the follow-up period, 431 patients continued on PD, 20 had recovered RRF, 369 had received kidney transplants, 199 switched to HD, and 139 died.
RESULTS
The total time of follow-up reached 1989.5 patient-years, with a mean follow-up time of 1.71 years/patient (range: 1 month – 6.9 years). Only 1.6% of patients were lost from follow-up. At the end of the follow-up period, 431 patients (36.6%) continued on PD. Figure 1 displays patient movements, with recovery of renal function, changes to the modality of RRT provided, or death.
A total of 1091 episodes of peritonitis were registered during the follow-up period, of which 476 corresponded to a first episode. As such, the rate of peritonitis was estimated at 0.55 episodes/year, with a 95% CI of 0.52-0.58; this is equivalent to one case of peritonitis every 22 months.
Those patients who never suffered an episode of peritonitis were on average younger than those who did (53.1 years [SD: 15.67] vs 57.42 years [SD: 15.00]; P<.001). These patients also started PD with a lower comorbidity index, a lower prevalence of DM (20.3% vs 25.6%; P=.03), and a lower rate of prior CV events (21.7% vs 28.8%; P=.006). Patients who suffered an episode of peritonitis were more likely to have received another type of RRT previously, whether HD or transplantation (Table 1).
Description and prognostic factors for the first episode of peritonitis
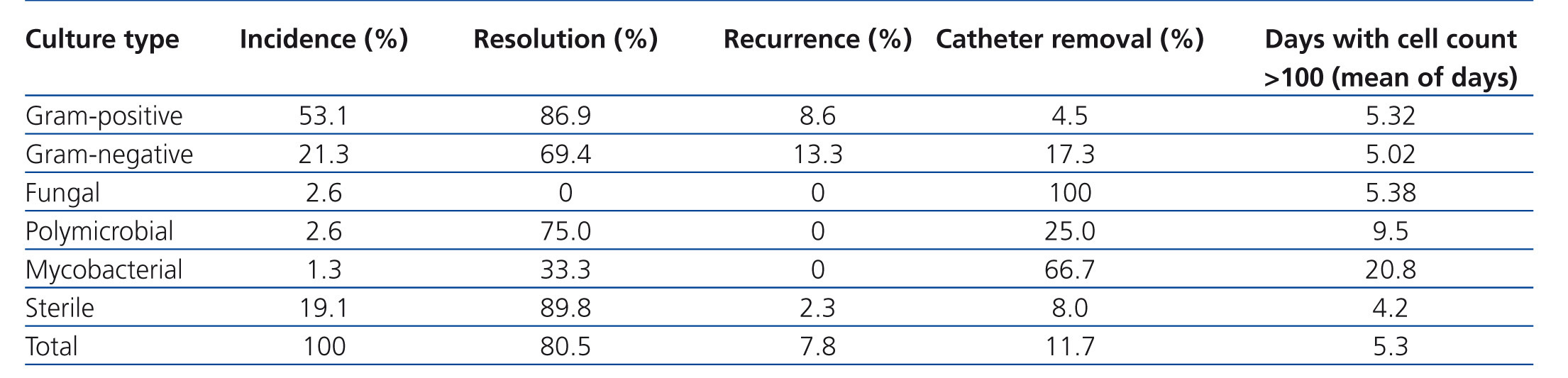
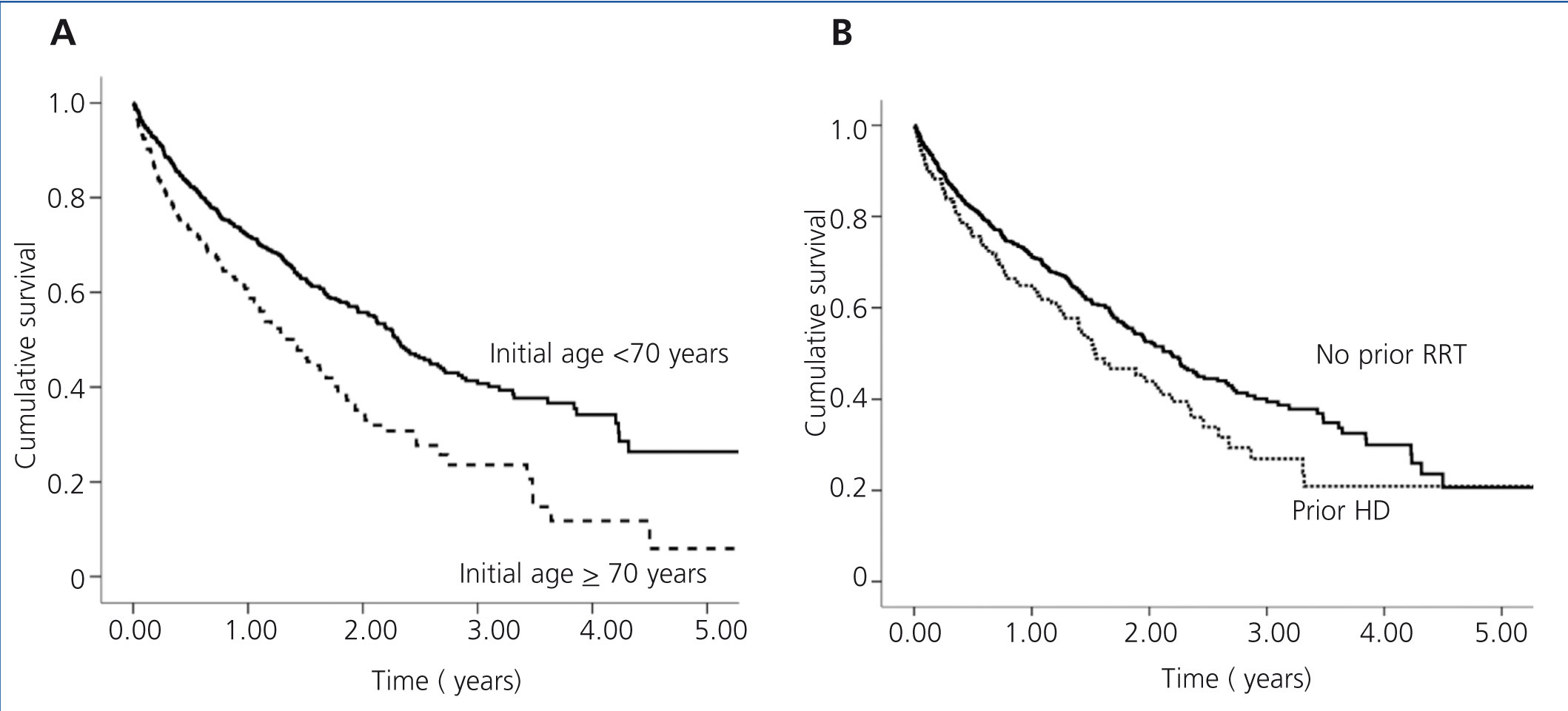
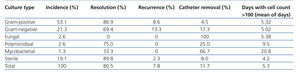
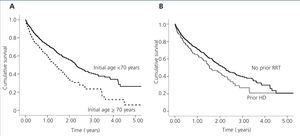
We recorded a total of 476 first episodes of peritonitis. The mean time elapsed until the first episode, as analysed using the KM test, was 2.1 years (1.87-2.32) (Figure 2). In these 476 first cases of peritonitis, the distribution of aetiological causes was similar to that observed for the global sample of peritonitis episodes (data not shown): 53.1% gram-positive bacteria, 21.3% gram-negative bacteria, 2.6% polymicrobial, 2.6% fungal, 1.3% mycobacterial, and 19.1% with a sterile culture.
The majority of cases of peritonitis progressed favourably towards resolution with no recurrence (80.5%). Negative results were considered to be catheter removal (11.7%) and recurrence (7.8%). No deaths were ascribed to peritonitis. However, 6 deaths were recorded within 30 days of the first episode of peritonitis. Hospitalisation was required in 37.6% of cases, with a mean hospital stay of 8.6 days per hospitalisation. Cell counts fell below 100/ml in a mean period of 5.29 days. Table 2 summarises the progression of cases of peritonitis based on the causative microorganism.
The time interval until the first episode of peritonitis was lower in patients coming from HD as compared to those with no previous experience on RRT (1.54 years [1.17-1.91] vs 2.18 years [1.92-2.44]; P=.016) or who had received a transplant (2.13 years [0.95-3.31]). Age groups were defined as older than or younger than 70 years of age. The rate of peritonitis was higher in patients older than 70 years (0.758 cases of peritonitis/year [0.676-0.847] vs 0.49 cases/year [0.456-0.526]; P=.001). In addition, 53.4% of patients older than 70 years of age suffered at least one episode of peritonitis, as compared to 37.5% of patients younger than 70 years (P<.001).
In terms of initial PD technique used, 43.9% of patients on CAPD developed peritonitis, as compared to 36.4% of patients who started on APD. Patients on APD were younger on average (50.1 years vs 57.0 years; P<.001) than patients on CAPD. However, the Charlson comorbidity index (without taking into account age) was similar between these two groups (3.07 vs 3.09; P>.05). Patients who started on APD had a greater rate of derivation from HD (22.4% vs 15.2%) or TX (12.5% vs 5.2%); P<.001. Patients on CAPD tended to suffer their first episode of peritonitis earlier in their treatment, with a median estimated time interval from the start of treatment of 1.86 years, as compared to 2.37 years for patients on automated PD (P=.001), with an estimated HR of 1.42 [1.16-1.75]. Once results were corrected for comorbidities, this effect persisted. Other clinically important factors, such as sex or presence of DM, did not reach statistical significance.
The Cox regression analysis of time until the first case of peritonitis included the following variables: age older than 70 years (HR: 1.53 [1.23-1.90]), prior history of a CV event (HR: 1.25 [1.04-1.58]), prior dialysis treatment modality (HR: 1.39 [1.10-1.76] for patients coming from HD, and HR: 1.38 [0.99-1.93] for patients coming from TX), and starting on a manual technique as opposed to a cycler (HR: 1.39 [1.13-1.73]).
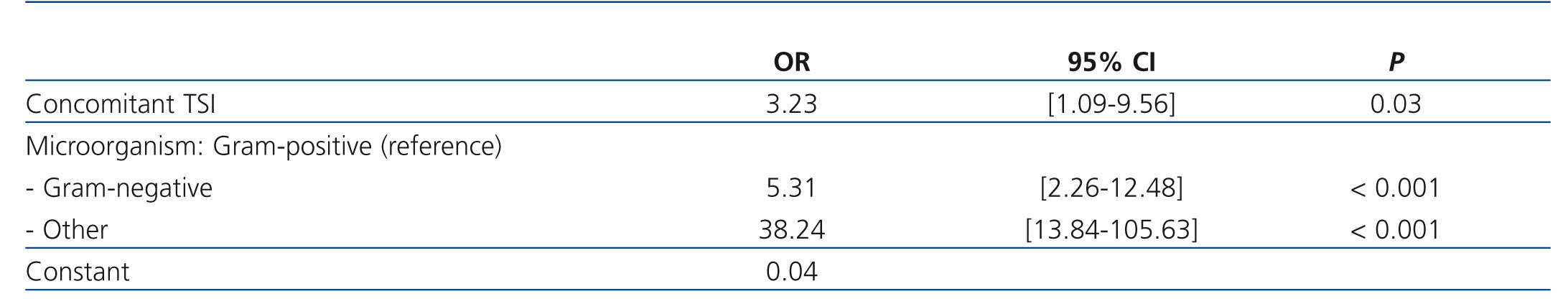
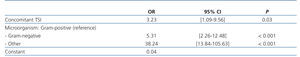
The model yielded type of causative microorganism and exit site infection as prognostic factors for negative results of the first episode of peritonitis (catheter removal or death) (Table 3). We used a logistic regression model with an R2 value of 30%, in which no significant changes were observed when correcting for comorbidity using the Charlson index. As such, this could be a valid model regardless of comorbidities present, making the type of causal microorganism the primary factor in determining patient evolution. In this manner, a peritoneal fluid culture resulting positive for gram-negative bacteria induces a greater risk for poor evolution than gram-positive bacteria (OR: 5.31 [2.26-12.48]), whereas episodes of peritonitis caused by multiple microbes, mycobacteria, or fungal infections present an OR of 38.24 [13.84-105.63], when compared to the reference value of gram-positive bacteria. Other factors such as the need for hospitalisation and time to hospitalisation were not included in the analysis due to a lack of independence.
DISCUSSION
Our study provides recent data regarding the incidence, characteristics, and prognostic factors for a first episode of peritoneal infections, as well as an estimation of the time elapsed until this first episode. Peritonitis remains the most important complication in PD. The global rate of peritonitis in our study sample was fairly stable over time, approximately 0.55 cases of peritonitis/patient-year, which is similar to rates published in other studies.12,13 We also observed that patients older than 70 years of age, those with associated comorbidities, and those who received previous treatment with HD or a TX are more susceptible to suffer the first episode of peritonitis at an earlier time.
An improved understanding of the characteristics associated with the development of this first episode of peritonitis allows for establishing prevention measures and delaying its appearance as long as possible. This first episode affects the survival of the peritoneal membrane as a medium for dialysis as well as the survival of the patient.14 The importance of prolonging the period of treatment until this first episode of peritonitis lies in the possibility of transferring a patient from PD to a TX without ever having suffered an infection. This is especially relevant in our group of patients, since the primary cause of exit from PD is transplantation, with higher success rates than those published in other studies, at a mean 1.74 years [1.55-1.92] from the start of treatment.15,16 In addition, peritonitis is a temporary contraindication for TX, thus prolonging the wait time until a TX would be feasible. As such, our objective must be providing high-quality PD without infection until a transplant is made available.
Another negative effect of peritonitis is hospitalisation, which goes directly against the primary advantage of PD, the availability of home-based treatment, and imposes personal repercussions on the patient and extra costs for the health system. Despite similar results presented in studies by other authors,17 we believe that the rate of hospitalisations due to peritonitis is high. This could be justified by the indications for hospitalisation being based more on organisational criteria than clinical severity, since patients often seek hospital treatment during hours when the PD unit personnel are not present. Results in terms of short hospital stays and positive clinical evolution would support this hypothesis. This is a controversial issue since guidelines clearly establish diagnostic criteria and preferential choices for antibiotic treatments, but do not establish when the patient should be hospitalised. A clear definition of these hospitalisation criteria would help optimise health resources and reduce morbidity rates and health costs related to PD.18
The distribution of microorganisms causing episodes of peritonitis was similar to that described recently by other authors,19 with a reduced rate of gram-positive infections as compared to historical values.20 This could be due to improvements in the double bag system used by patients in our study.21 We did not observe a difference in types of infections produced in first or subsequent episodes of peritonitis. The rate of sterile culture results in our study was higher than in other studies,22 although still well within target ranges. This could be due to improper sample processing, early extraction (when cell counts are still quite low), or chemical peritonitis.
The relationship between patient age and risk of peritonitis is the subject of some debate.5,6,23 In our study, we considered “elderly” patients those over 70 years of age, based on commonly used standards in geriatrics studies. These patients in our study had a shorter initial time period until the first infection, which is in contrast to the results reported in another article concerning first episodes of peritonitis.13,16 Our finding was also reported by other authors,24 who estimated that the risk of peritonitis increased by 26% for every 10-year increase in patient age.6 This finding could be explained by decreased dexterity and vision, which can be a hindrance to proper aseptic technique in elderly patients, in addition to a lower rate of automated PD technique use in these individuals.
The peritonitis rate was greater in patients who started dialysis on manual PD as compared to those who started on automated PD. This pattern is observed in most studies,25,26 although not all,27 and is attributed to the increased risk associated with a greater number of connections used in manual techniques. Ours was not a randomised study, and technique choice may have been associated with other confounding factors, such as assigning manual techniques to elderly patients as a standard practice, which would subtract from the relevance of this finding.
Patients who have transferred from HD have a shorter time interval until suffering a first episode of peritonitis, which could contribute to the inferior evolution of these patients observed in previous studies.28 This increase in risk of peritonitis could be due to decreased motivation on the part of the patient when switched from HD to PD due to clinical indications as opposed to free choice, along with a sub-optimal training in PD techniques when this change is mandatory. One could also argue that these patients would tend to have greater comorbidity, and yet this effect persisted even after correcting for Charlson comorbidity index values in the model (age and comorbidity). As such, it is very important that the patient be allowed to freely choose the dialysis technique to be applied whenever possible, with increased support from the medical team and added measures to care for patients who are forced to switch to PD due to clinical reasons.
Several studies have observed a higher rate of peritonitis in women, above all those caused by gram-negative bacilli derived from vaginal contamination.6 In our patient cohort, we did not observe any differences in rates of peritonitis between sexes, or even in the number of episodes or proportion of causal microorganisms. The role of DM in the incidence of peritonitis is another source of controversy,5,16 and we did not identify this condition as a risk factor for the first episode of peritonitis, although we should point out that the prevalence of DM in our sample was lower than that reported in other studies.7,16,29 In our experience, CV comorbidity is associated with previous RRT, older age, and DM.28 With this in mind, the introduction of one of the two types of comorbidity (CV or DM) in a multivariate model would negate the need for the other. We selected the model incorporating CV as opposed to DM because of the greater statistical weight produced.
In our study, the first episode of peritonitis resulted in negative results in 20% of cases, requiring catheter removal or leading to recurrence or death. Predictive factors for catheter removal included type of causative microorganism and concomitant infection of the tube site.17,18,30 Mortality rates at the end of the follow-up period were low, and no deaths were reported as a result of peritonitis, although 6 patients did die within the first month following the first episode of peritonitis. This could be due to early catheter removal in the event of poor evolution of the episode of peritonitis, giving priority to protecting the patient over maintaining the dialysis technique. In effect, many patients whose catheters are removed switch definitively to HD, whether due to failure of the peritoneal membrane or the negative experience associated with this complication, which would affect long-term survival of the patient on PD.
We must also mention the limitations inherent to our study. Firstly, the observational design only allows for establishing correlations, not causality. In addition, the lack of a unified empirical treatment protocol for catheter removal hinders any attempt at a global analysis. Despite the recommendations by the ISPD for avoiding antibiotic resistance,10,11 13 of the participating centres used vancomycin as an empirical treatment to cover gram-positive bacterial infections. This strategy is not necessarily condemnable, and may depend on ecological factors and a high prevalence of bacterial resistance within each hospital, or even strategic decisions in the context of methods of administration.
Peritonitis continues to be the most important complication of PD, despite recent technological advancements. Our analysis provides updated information on a large sample of patients, which represent a specific geographic area, allowing us to present information on their characteristics, with the goal of improving prophylactic and treatment goals and monitoring changes over time.
CONCLUSIONS
Our study describes: the incidence, characteristics, and prognostic factors of first episodes of peritonitis in a large, representative, homogeneous, and contemporary sample of patients on PD. The early identification of patients at high risk for developing peritonitis (such as those transferring from HD) will help assign prevention measures, provide proper patient training in dialysis methods, and facilitate early treatments in order to delay the onset of peritoneal infections and minimise their impacts on patient survival and maintenance on PD.
Conflicts of interest
This project was co-financed by Baxter (2003-2013), Amgen (2005-2013), and Fresenius (2007-2013) through the Madrid-based Nefrología-SOMANE Foundation. The authors have no contractual obligations, nor do they serve on any advising committees, for PD companies in Spain.
Table 1. Baseline characteristics comparing patients who have suffered at least one episode of peritonitis during the monitoring period with those who have not
Table 2. Description of first cases of peritonitis according to causative microorganism
Table 3. Negative prognostic factors for peritonitis (event: catheter removal; multivariate logistic regression analysis)
Figure 1. Flow rates in study patients
Figure 2. Survival analysis until the first episode of peritonitis comparing patients who started peritoneal dialysis prior to the age of 70 years with those who started peritoneal dialysis after an age of 70 years (A) and based on prior treatment provided)