Fibrillary glomerulonephritis (FGN) is a rare entity defined by the finding of randomly arranged, unbranched fibrils between 15 and 25 nm in diameter in electron microscopy (EM).1 5 patterns have been defined in optical microscopy (OM) related to clinical presentation and prognosis.2–5 However, the greatest contribution to the diagnosis of this entity has been the discovery of the immunohistochemical marker DNAJB9, a marker with a sensitivity of 98% and a specificity of 99%.6,7 Furthermore, the use of the C4d marker, widely used in other kidney diseases,8 can contribute to the diagnosis.
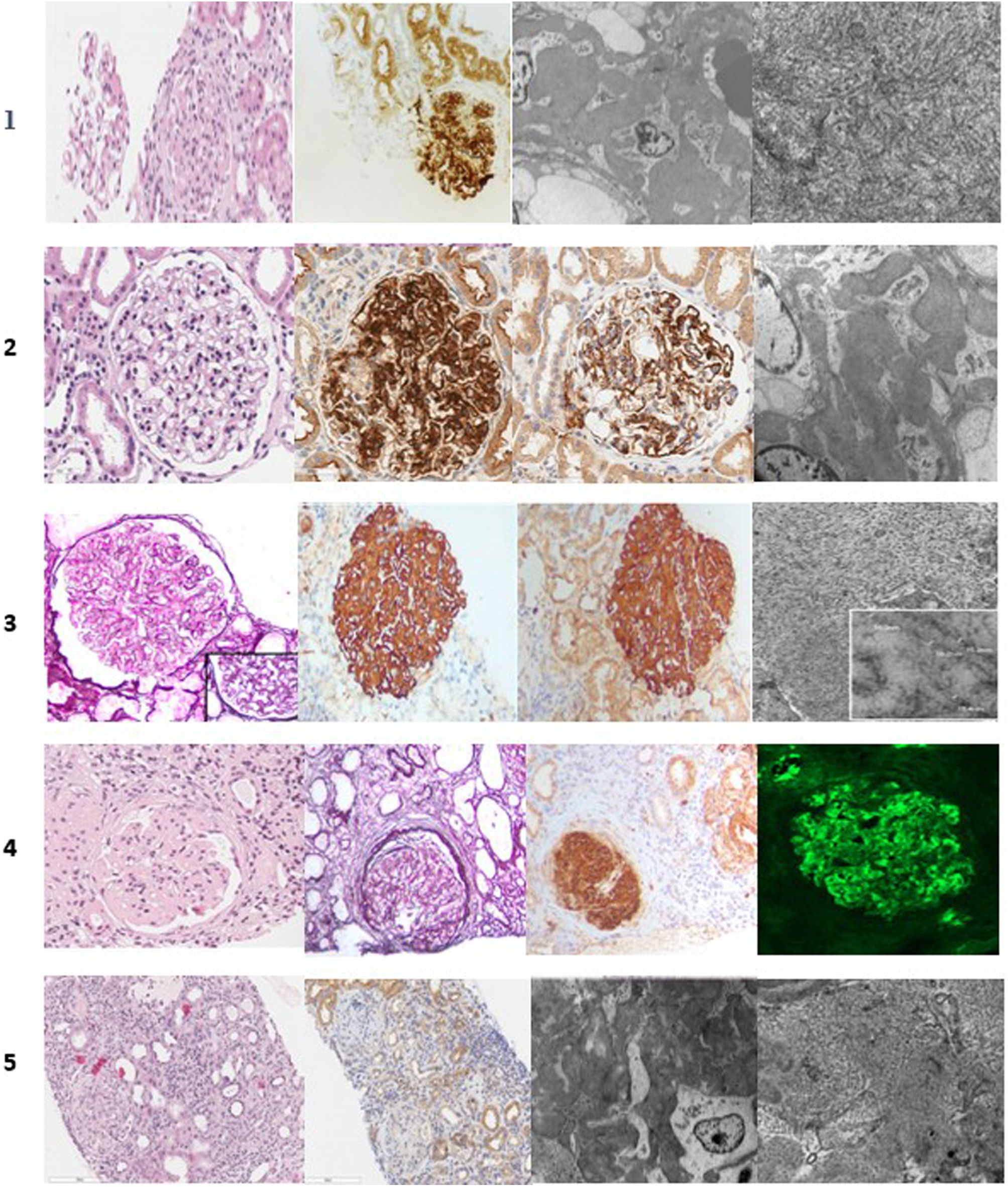
We present 5 cases of FGN with epidemiological, diagnostic and associative relevance (Table 1 and Fig. 1). The incidence of FGN is lower than 1%,1–4 but the incidence of our sample is higher, with 5 cases among 135 biopsies performed, providing an incidence of 3.7%. This could be justified by the recent discovery of the DNAJB9 marker as a diagnostic tool.
Clinical cases.
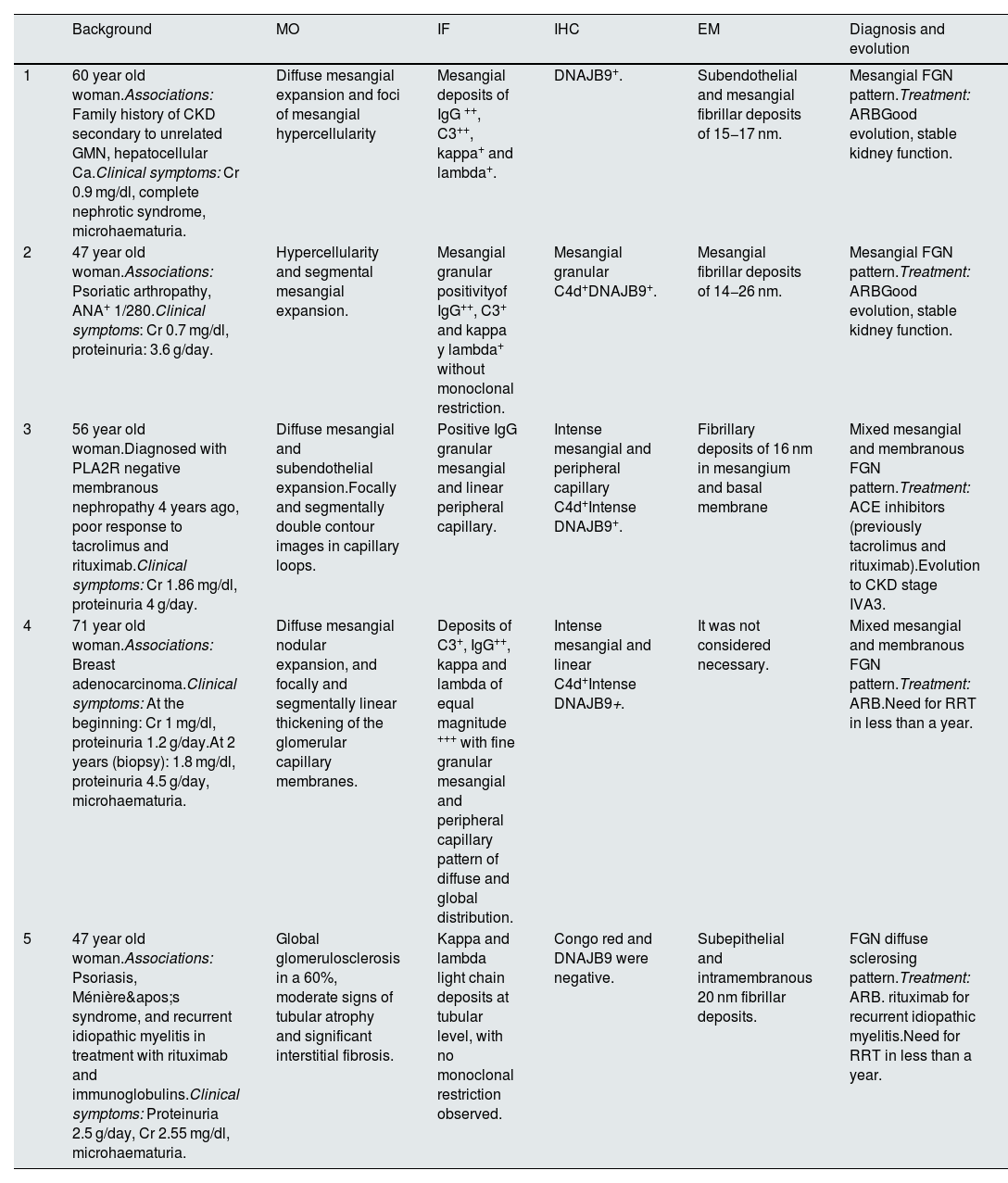
| Background | MO | IF | IHC | EM | Diagnosis and evolution | |
|---|---|---|---|---|---|---|
| 1 | 60 year old woman.Associations: Family history of CKD secondary to unrelated GMN, hepatocellular Ca.Clinical symptoms: Cr 0.9 mg/dl, complete nephrotic syndrome, microhaematuria. | Diffuse mesangial expansion and foci of mesangial hypercellularity | Mesangial deposits of IgG ++, C3++, kappa+ and lambda+. | DNAJB9+. | Subendothelial and mesangial fibrillar deposits of 15−17 nm. | Mesangial FGN pattern.Treatment: ARBGood evolution, stable kidney function. |
| 2 | 47 year old woman.Associations: Psoriatic arthropathy, ANA+ 1/280.Clinical symptoms: Cr 0.7 mg/dl, proteinuria: 3.6 g/day. | Hypercellularity and segmental mesangial expansion. | Mesangial granular positivityof IgG++, C3+ and kappa y lambda+ without monoclonal restriction. | Mesangial granular C4d+DNAJB9+. | Mesangial fibrillar deposits of 14−26 nm. | Mesangial FGN pattern.Treatment: ARBGood evolution, stable kidney function. |
| 3 | 56 year old woman.Diagnosed with PLA2R negative membranous nephropathy 4 years ago, poor response to tacrolimus and rituximab.Clinical symptoms: Cr 1.86 mg/dl, proteinuria 4 g/day. | Diffuse mesangial and subendothelial expansion.Focally and segmentally double contour images in capillary loops. | Positive IgG granular mesangial and linear peripheral capillary. | Intense mesangial and peripheral capillary C4d+Intense DNAJB9+. | Fibrillary deposits of 16 nm in mesangium and basal membrane | Mixed mesangial and membranous FGN pattern.Treatment: ACE inhibitors (previously tacrolimus and rituximab).Evolution to CKD stage IVA3. |
| 4 | 71 year old woman.Associations: Breast adenocarcinoma.Clinical symptoms: At the beginning: Cr 1 mg/dl, proteinuria 1.2 g/day.At 2 years (biopsy): 1.8 mg/dl, proteinuria 4.5 g/day, microhaematuria. | Diffuse mesangial nodular expansion, and focally and segmentally linear thickening of the glomerular capillary membranes. | Deposits of C3+, IgG++, kappa and lambda of equal magnitude +++ with fine granular mesangial and peripheral capillary pattern of diffuse and global distribution. | Intense mesangial and linear C4d+Intense DNAJB9+. | It was not considered necessary. | Mixed mesangial and membranous FGN pattern.Treatment: ARB.Need for RRT in less than a year. |
| 5 | 47 year old woman.Associations: Psoriasis, Ménière's syndrome, and recurrent idiopathic myelitis in treatment with rituximab and immunoglobulins.Clinical symptoms: Proteinuria 2.5 g/day, Cr 2.55 mg/dl, microhaematuria. | Global glomerulosclerosis in a 60%, moderate signs of tubular atrophy and significant interstitial fibrosis. | Kappa and lambda light chain deposits at tubular level, with no monoclonal restriction observed. | Congo red and DNAJB9 were negative. | Subepithelial and intramembranous 20 nm fibrillar deposits. | FGN diffuse sclerosing pattern.Treatment: ARB. rituximab for recurrent idiopathic myelitis.Need for RRT in less than a year. |
ACE inhibitors: angiotensin-converting enzyme inhibitors; ARB: angiotensin II receptor antagonists; CKD: chronic kidney disease; EM: electron microscopy; FGN: fibrillar glomerulonephritis; GMN: glomerulonephritis; IF: immunofluorescence; IHC: immunohistochemistry; OM: optical microscopy; RRT: renal replacement therapy.
Histology of clinical cases. Case 1: haematoxylin-eosin (H & E), DNAJB9, electron microscopy (EM). Case 2: H&E, DNAJB9, C4d, EM. Case 3: methenamine silver staining, C4d, DNAJB9, EM. Case 4: H&E, methenamine silver staining, DNAJB9 and IgG immunofluorescence. Case 5: H&E, DNAJB9 negative, EM.
Clinically, it usually begins in the fifth or sixth decade of life, with a predominance in Caucasian women, as occurred in our cases. There is a broad clinical spectrum, with the most common being the association of deterioration in renal function, proteinuria and microhematuria.1 In our series, 3 of the 5 patients had altered renal function at the onset, all had proteinuria, 4 of them were in the nephrotic range, and 3 had microhematuria.
Its association with the hepatitis C virus, dysproteinemias, autoimmune diseases, diabetes mellitus and malignancy has been described.2–4 In our series, 2 patients presented tumour disease (breast adenocarcinoma and hepatocellular carcinoma) and one patient presented ANA+, without correlating with autoimmune disease. There is also a case with diagnosed recurrent myelitis, classified as idiopathic, and a case with a family history of unknown glomerulopathy. The literature describes some cases of familial association of FGN, such as the paper published in 2015 by Ying T et al., in which two Australian families were diagnosed with FGN with an autosomal dominant inheritance pattern.9
In the BM, we found 2 cases of isolated mesangial pattern, 2 cases with a combination of mesangial and membranous pattern and one case with diffuse sclerosing pattern. Similar to the literature,1–4 the 2 patients with a mesangial pattern presented better outcomes. Two patients had a mixed mesangial and membranous pattern, which, although in isolation, have been correlated with a better prognosis. The association of patterns could explain the worse evolution, especially for case number 4. Finally, the patient with a sclerosing pattern diffuse presented poor evolution.
The recent discovery of DNJAB9 as a diagnostic tool,6,7 with a sensitivity of 98% and a specificity >99%, has meant an important advance in histological diagnosis. It may even avoid performing ultrastructural studies in patients with positive DNJAB9. In our series, 4 of the patients were DNAJB9 positive, avoiding the use of EM in one of the cases. For the last case, with DNAJB9, negative Congo red ruled out the possibility of advanced amyloidosis, and the advanced optical microscopy pattern ruled out the possibility of incipient amyloidosis. Finally, electron microscopy confirmed the diagnosis, this being the gold standard examination.
Although DNAJB9 is a highly specific tool, it is not routinely performed in all renal biopsies, so there must be a prior histopathological suspicion to request it. The use of markers such as C4d, widely used in other kidney diseases, was key for the differential diagnosis in case 4, previously diagnosed with membranous nephropathy, since upon observing that in addition to the classic pattern of membranous deposits, there was also mesangial deposits, which led to considering other diagnoses, requesting DNAJB9 and EM, and thus confirming the diagnosis.
No optimal therapy for fibrillary glomerulonephritis has been established to date.1 In addition to conservative medical therapy for the treatment of proteinuria, some immunosuppressants have been tested: steroids, mycophenolate, rituximab or cyclophosphamide. However, the results are not very encouraging, and it is rituximab that has shown an apparent benefit.10 In our series, all patients were conservatively treated after diagnostic confirmation. Additionally, 2 patients received treatment with rituximab, one due to a previous diagnosis of membranous nephropathy and another case for recurrent myelopathy. Both presented poor evolution.
In conclusion, FGN is a rare clinical entity, but it is probably underdiagnosed. The appearance of new diagnostic tools, such as the DNAJB9 marker, may lead to higher numbers of diagnoses in the coming years. The prognosis is related to the histological pattern observed, and currently, there are limited therapeutic options. Therefore, new studies are required to improve the treatment and management of the disease.