Carbamazepine is used in the treatment of epilepsy, and also prescribed in neuralgic pain syndromes, and certain affective disorders. Carbamazepine intoxication with suicide attempt is a relatively common clinical problem that can result in coma, respiratory depression, arrhythmia, hemodynamic instability and death. The drug's relatively high molecular weight, elevated volume of distribution and intense protein-binding render it difficult to extracorporeal removal, but published experience with hemoperfusion or hemodialysis present variable results. We describe a case report involving carbamazepine intoxication who was successfully treated with charcoal hemoperfusion. With this treatment the half-life of carbamazepine was reduced with rapid lowering of carbamazepine levels and clinical improvement. Based on our experience in this patient and a review of previously reported cases, extended charcoal hemoperfusion should be considered for serious carbamazepine intoxication because free as well as bound drug fractions are eliminated via this technique.
La intoxicación aguda por carbamazepina en los intentos autolíticos es un problema clínico bastante común que puede dar lugar a coma, depresión respiratoria, arritmias, inestabilidad hemodinámica y muerte. El fármaco tiene un peso molecular relativamente elevado, un volumen de distribución moderadamente grande y una intensa fijación a las proteínas. En caso de sobredosis, estas características farmacocinéticas hacen su eliminación extracorpórea difícil, por lo que la experiencia publicada con hemoperfusión o hemodiálisis presenta resultados variables. Se presenta un caso de intoxicación aguda por carbamazepina que fue tratado exitosamente con medidas de soporte general y una sesión de hemoperfusión con carbón activado. Esta técnica produjo una extracción considerable del fármaco, mejorando rápidamente los signos clínicos de intoxicación. Basados en la experiencia con esta paciente y en la revisión de otros casos publicados, concluimos que en la intoxicación aguda por carbamazepina el tratamiento precoz con hemoperfusión prolongada debe considerarse de elección.
INTRODUCTION
Carbamazepine is used to treat epilepsy, neuropathic pain, certain affective disorders and as a migraine prophylactic drug. Carbamazepine poisoning, resulting from attempted suicide, is a relatively common clinical problem which can result in coma, hypoventilation, arrhythmias, haemodynamic instability and death.1,2 In the event of an overdose, the drug’s relatively high molecular weight, moderately large distribution volume and high protein-binding capacity makes it difficult to eliminate from the body. For that reason, published experiences using haemoperfusion or haemodialysis yielded highly variable results.3-16 We describe a patient with acute carbamazepine poisoning who was successfully treated with prolonged haemoperfusion. This case serves to illustrate that in cases of acute carbamazepine poisoning for which extracorporeal techniques are indicated, prolonged haemoperfusion with activated charcoal is effective for quickly lowering circulating substance levels.
CASE REPORT
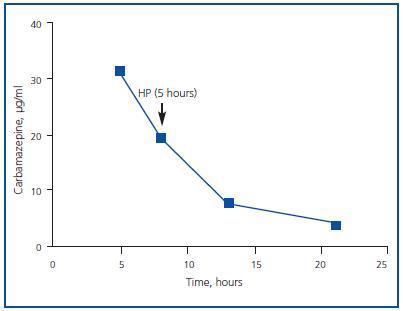
Female patient 27 years of age diagnosed with a personality disorder whose basic treatment consisted of 400 mg/day carbamazepine, 75mg/day venlafaxine, 5mg/day lorazepam and 15mg/day clorazepate dipotassium. The patient was admitted due to a suicide attempt with an undetermined amount of carbamazepine. The patient arrived at the emergency room approximately five hours after having ingested the drug. She was conscious with a Glasgow score of 7 and showed mydriatic pupils, mild drowsiness and disorientation. 1,500ml of isotonic saline solution and 1,500ml of 5% glucose solution were administered.Arterial pressure was 123/65mmHg, heart rate was 90 beats/min and diuresis progressed at 150-200ml/hour. Five hours after having ingested the drug and following several gastric lavages with activated charcoal, carbamazepine plasma levels were at 31.2µg/ml. Other laboratory data were as follows: haematocrit 37%, haemoglobin 13g/dl, leukocyte count 12,800/mm3, Platelet count 225,000/mm3, glucose 80mg/dl, urea 33mg/dl, creatinine 0.96mg/dl, Na 138mmol/l, K 3.6mmol/l, Cl 104mmol/l, bicarbonate 20.8mmol/l, total calcium 8.9mg/dl, total proteins 7.5g/dl, GOT 18IU/l, GPT 37IU/l, prothrombin activity 110%, INR 0.9. Normal ECG. The patient was moved to the Intensive Care Unit for monitoring, and three hours after having been admitted, began haemoperfusion treatment with a cartridge of activated charcoal (Adsorba 300 C, Gambro, Hechingen, Germany) with a blood flow rate of 180ml/min. The pre-haemoperfusion carbamazepine level was 19.5µg/ml. In the five hours during which haemoperfusion was performed and afterwards, the patient remained haemodynamically stable with a diuresis of 150ml/h. The post-haemoperfusion carbamazepine level was 7.8µg/ml, and eight hours later, it was 3.9µg/ml. The patient was discharged 24 hours later for follow-up by the Psychiatric Unit.
METHODS
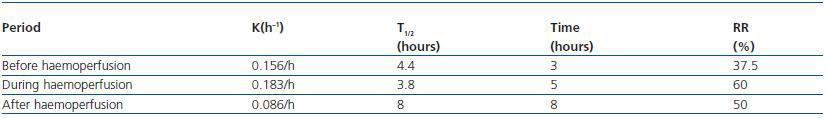
Carbamazepine plasma levels were determined using a fluorescence polarisation immunoassay (Abbott). The analysed samples were obtained at time of admission, pre- and post-haemoperfusion, and several hours after completing the treatment. The therapeutic range for carbamazepine is between 4 and 12µg/ml. To determine the specific pharmacokinetic parameters, we used carbamazepine plasma concentrations and employed standard equations to calculate the constant elimination rate (Kel) and the carbamazepine half-life (T1/2) before, during and after haemoperfusion: Kel (h-1) = 1/time * ln (C1/C2); T1/2 = 0,693/Kel, where “time” is the number of hours between carbamazepine concentrations C1 and C2. The reduction rate (RR) was calculated using the following formula: RR = 100 x (1-C2/C1).
DISCUSSION
Carbamazepine distribution and metabolism are complex processes. Carbamazepine has a molecular weight of 236 Daltons. After oral administration, it is absorbed slowly (70-95%), with a maximum plasma peak between 2 and 18 hours. It binds tightly to proteins (80-85%) and its distribution volume is 1-2L/kg; its elimination is fundamentally hepatic, through the P450 (CYP3A4) cytochrome system, and only 1-3% is eliminated by the kidney. The drug’s elimination half-life is between 12 and 20 hours, but an overdose can last as long as 55 hours.15
Carbamazepine poisoning can result in coma, hypoventilation, arrhythmias, haemodynamic instability and death. The mortality rate is as high as 13% of all cases.2 Keeping in mind the circulating level of carbamazepine, poisoning can be classified in four stages: potentially catastrophic relapse with levels < 11µg/ml, disorientation and ataxia at levels of 11-15µg/ml, combativeness and hallucinations at levels of 15-25µg/ml and convulsions and coma at levels > 25µg/ml.8
Treatment for carbamazepine overdose has drawn on diverse extracorporeal elimination techniques such as haemoperfusion, haemodialysis, a combination of both, continuous haemodiafiltration and even plasmapheresis.3-21
However, the most commonly used technique since the 1980s has been haemoperfusion with activated charcoal, which reduces circulating carbamazepine levels in some poisoned patients by 25-50% after 3-4 hours of treatment.6-8 In other cases treated with haemodialysis using highly permeable membranes, circulating carbamazepine levels decreased by 25-27% in 3 to 4 hours.10,11 In a recent case that was treated with haemodialysis over four hours, the carbamazepine level was reduced by more than 50%.9 In another study, the combined use of haemodialysis and haemoperfusion resulted in a plasma level reduction of 50%.14 One theory to explain haemodialysis’ paradoxical efficacy in eliminating the drug, despite its tight protein binding, suggests a high breakage rate of the drug’s union to proteins which would take place in countercurrent flows through the pores in the dialyser membrane.13 In a few cases in which plasmapheresis was performed, results were inconsistent.19-21 Continuous albumin dialysis is another treatment option that resulted in an elimination T1/2 of 4.5 hours.17 In turn, when haemoperfusion with activated charcoal and high-flux haemofiltration was used, the elimination T1/2 varied between four and eight hours. For all of these reasons, it is evident that studies of larger patient groups are needed in order to evaluate the efficacy of different extrarenal purification techniques. Other techniques such as MARS or Prometheus could also be useful.
According to the initial carbamazepine levels, our patient was in a severe state of intoxication. The elapsed time since the patient ingested the drug (about five hours) permitted elimination of a certain amount of it by gastric lavage, and probably also its adsorption to the activated charcoal administered through the nasogastric tube. With five hours of haemoperfusion, the carbamazepine plasma level dropped by 60% and over the next eight hours, using only forced diuresis, levels remained within the therapeutic range with no rebound effect (figure 1). The anticipated T1/2 of 20 hours was lowered to 3.8 hours during haemoperfusion treatment (table 1). In this patient, the carbamazepine T1/2 was much lower than in previously published cases for which toxicokinetic studies were carried out.6,7 Therefore in this case, haemoperfusion resulted in the extraction of a considerable amount of the circulating carbamazepine, which was probably due to its long duration; according to our estimates, the cartridge became saturated after seven hours.5 Following haemoperfusion, when only endogenous elimination (hepatic and renal) was being used, spontaneous clearance of carbamazepine resulted in an elimination T1/2 of eight hours. The only complication during hospital treatment was transitory thrombocytopenia, which resulted from the technique. The clinical profile was resolved in 24 hours.
In conclusion, in addition to the general support measures (which should include gastric lavage with activated charcoal and forced diuresis, both of which can eliminate an amount of free substance) early use of haemoperfusion is effective for rapidly lowering circulating carbamazepine levels in those cases of acute poisoning for which extracorporeal techniques are indicated.
Figure 1.
Table 1. Pharmacokinetics of carbamazepine before, during and after haemoperfusion