Chronic kidney disease represents an important health problem, due to its high incidence and prevalence, as well as its significant morbidity and mortality and socioeconomic cost.
Aimscompare the effectiveness and economic consequences of outsourcing versus hospital dialysis.
MethodA scoping review, for which different databases were consulted, using controlled and free terms. Those articles that compared concerted versus in hospital dialysis in terms of effectiveness were included. Likewise, those publications that compared, in the Spanish field, the cost between both modes of service provision and the public price rates of the different Autonomous Communities were included.
Results11 articles were included in this review: 8 on comparison of effectiveness, all of them in the USA, and 3 on costs. A higher rate of hospitalization was observed in subsidized centers, but no differences in mortality were observed. Additionally, greater competition among providers was associated with lower hospitalization rates. The cost studies reviewed show that hospital hemodialysis is more expensive than in subsidized centers, due to the structural costs. The data of the public rates of the different Autonomous Communities show a wide heterogeneity in the payment of the concerts.
Conclusionsthe coexistence in Spain of public and subsidized centers, the variability in the provision and costs of dialysis techniques, and the low of evidence on the effectiveness of outsourcing treatment show all the need to continue promoting strategies that result in improvement in the care for Chronic Kidney Disease.
La enfermedad renal crónica representa un importante problema de salud, tanto por su elevada incidencia y prevalencia, como por su importante morbimortalidad y coste socioeconómico.
ObjetivoComparar la efectividad y consecuencias económicas de la diálisis concertada frente a la diálisis hospitalaria.
MetodologíaRevisión de alcance, para lo cual se consultaron diferentes bases de datos, mediante términos controlados y libres. Se incluyeron aquellos artículos que comparasen la diálisis concertada frente a la hospitalaria en términos de efectividad. Igualmente, se incluyeron aquellas publicaciones que comparasen, en el ámbito español, el coste entre ambas modalidades de prestación de servicios y las tarifas de precios públicos de las diferentes Comunidades Autónomas.
ResultadosEn esta revisión se incluyeron 11 artículos: 8 sobre comparación de la efectividad, todos ellos en EEUU y 3 sobre costes. Se observó una mayor tasa de hospitalización en aquellos centros concertados, pero no se observaron diferencias en mortalidad. Además, una mayor competencia entre proveedores se asoció a menores tasas de hospitalización. Los estudios de costes revisados muestran que la hemodiálisis hospitalaria es más costosa que en centros concertados, debido a los costes de estructura. Los datos de las tarifas públicas de las diferentes Comunidades Autónomas muestran una amplia heterogeneidad en el pago de los conciertos.
Conclusionesla coexistencia en España de centros públicos y concertados, la variabilidad en la prestación y costes de las técnicas de diálisis y la escasa evidencia sobre la efectividad de la externalización del tratamiento ponen de manifiesto la necesidad de seguir potenciando estrategias que redunden en una mejora de la atención a la Enfermedad Renal Crónica.
Chronic kidney disease (CKD) represents a major health problem, both due to its high incidence and prevalence, as well as its significant morbidity and mortality and socioeconomic cost1. In our country, renal replacement therapy (RTR) provides therapeutic support to 64,292 patients, according to data from 2019, of which 54.7% were patients with a functioning transplant, 4.9% were on peritoneal dialysis (PD), and 40.3% on hemodialysis (HD)2.
Non-transplanted patients choose from various RRT alternatives: conservative treatment or dialysis in its different modalities and settings. The choice of dialysis at home, in the intra- or extra-hospital setting (in satellite or peripheral centers) or supported centers is determined by various factors: structural and alignment of incentives, sociodemographic, patient (comorbidity, autonomy, etc.), professional, organizational and capacity of the service, or the distance itself to the health center3,4.
In the literature it is described that there is some heterogeneity in the quality of care in dialysis centers5. Two reports from agencies dedicated to health technology assessment of Canada (CADTH)6 and Norway (HPSR)7 found no differences in effectiveness in terms of hospitalizations (number and duration) and mortality between HD offered in subsidized centers, hospitals, or in peripheral centers (public and private). In Spain, the Spanish Society of Nephrology (SEN) published the "Guide for Dialysis Centers" in 20068 and 20119, which includes basic topics to guarantee the quality of treatment in out-of-hospital centers, in addition to addressing aspects of equity and good care practices. In 2012, the Quality Management Working Group of the Spanish Society of Nephrology developed a structure for weighting the results of HD centers that would allow the creation of an appropriate indicator to establish comparisons or benchmarking between centers10. Shortly after, the same group published a study that developed a methodology that estimated the worth of medical care generated for patients and society, provided in different types of HD centers, according to a group of results11.
Our RRT model is fundamentally based on HD and kidney transplantation, with a dialysis provision mechanism in which public-private collaboration has a high importance. Currently, around 357 centers12 provide services and a large number of patients belonging to the public health system receive HD in out-of-hospital centers, through agreements with the different health delegations.
The first Spanish experience of dialysis in a subsidized center (contracts between the center and the Public Administration) dates back to 1975 in Madrid (Dialcentro Clinic), with a price of 51−54 (8500−9000 pesetas) per session, including the following concepts: medications, diet, and attention to interrecurrent medical-surgical problems derived from renal failure and their treatment, including arteriovenous fistula (AVF)13.
Taking into account the high economic and social impact14, it is necessary to compile the available evidence to compare the effectiveness and economic consequences of concerted dialysis versus hospital dialysis. All this could serve to guide health managers and decision-makers in front of the different TSR provision options.
MethodologyA scope review15 was carried out, following the indications of the World Health Organization16 and following the proposed guide for scoping reviews17. Unlike systematic reviews, scoping reviews are exploratory and usually address a broad question. To do this, the following databases were consulted using free and controlled terms: PubMed, Embase, Web of Science (WOS), Cumulative Index to Nursing & Allied Health Literature (CINAHL), Scopus, and The Cochrane Library. This search was complemented with an exploration of the following resources: Google Scholar and the Network of Health Technology Assessment Agencies (https://redets.mscbs.gob.es/). The references included in the identified articles were examined and experts in key articles and publications on the subject under study were consulted via email (Appendix B Annex 1). In addition, the Official Gazettes of the different Spanish Autonomous Communities and the Mutual Society of Officials (MUFACE) were reviewed to extract the current public rates. The search strategy adopted for the different databases was validated by a librarian specializing in public health.
((“contract services” [MeSH Terms] OR “outsourcing agreement*” [Text Word] OR “contract service*” [Text Word] OR “reimbursement*” [Text Word] OR “Insurance, Health, Reimbursement” [Mesh] ) AND (“hemodialysis” [Text Word] OR “hemodialyses” [Text Word] OR “Renal Dialysis” [MeSH Terms] OR “Dialysis” [MeSH Terms] OR “Dialysis” [Text Word]))
Inclusion and exclusion criteria: all articles that made a comparison of contract dialysis versus the provision of services by the non-contracted one were included, in terms of results effectiveness, that is, the benefits obtained through the application of a health technology in terms of health outcomes (mortality, morbidity, hospital readmissions, etc.). The comparisons in terms of costs were limited to those studies carried out and published in Spain. Those references to studies in which no comparison was made between the types of centers and those published in a language other than English or Spanish were excluded; the search was limited to a period of 10 years.
Literature search results were stored in a Rayyan QCRI library, the screening process was performed in pairs (AOL and MdAGV) and discrepancies resolved by a third investigator (ACM). Firstly, by title and abstract (first selection); Subsequently, the full text articles were reviewed.
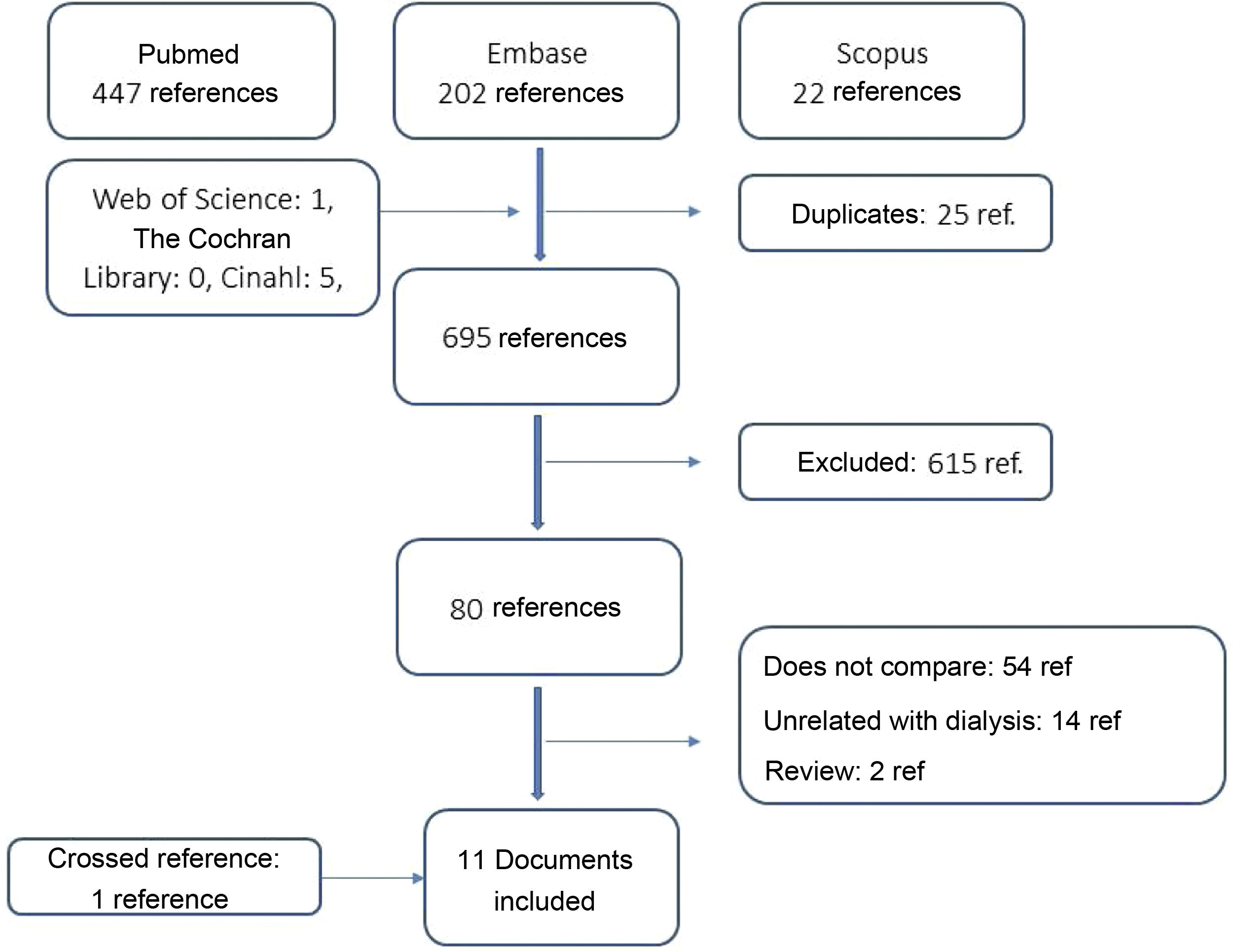
ResultsResults of the search processThe search identified a total of 720 references (PubMed: 447, Embase: 245, Scopus: 22, Web of Science: 1, and CINAHL: 5). After reading the titles and abstracts, a total of 103 references were selected for the next step of full-text evaluation, to ensure that the articles met all the eligibility criteria. Finally, after identifying an article through cross references, 11 articles were included in this review: eight on comparison of effectiveness and three on cost (Fig. 1).
Comparative effectivenessAll included studies on effectiveness have been conducted in the US. Three articles compared the effectiveness of organizations based on profitability, and included patients from the US Medicare Renal Registry cohort who received dialysis in 200318, 2005−200819 and 201020. The number of patients was 170,13018, 150,64219, and 366,01120, respectively, once different inclusion criteria were applied; of these, 9% received assistance in non-profit centers. Multivariate models showed that patients treated in for-profit centers had a higher relative rate of hospitalization, specifically, 15% (95% confidence interval [CI]: 13–18%; p < 0.001)19 (main causes: heart failure [37%] and volume overload [15%]) and days of hospitalization were increase by 17.5% in relation to those treated in non-profit centers (standard error 4.8; p < 0.001)18. In addition, Brunelli20 compared hospitalization and mortality rates, including 366,011 and 34,029 patients in for-profit and non-profit centers, respectively; and, it was found no significant differences in mortality (p = 0.64), nor in hospitalizations (p = 0.69).
On the other hand, there have been found four articles that compared the health outcomes of patients that received care in centers dependent on the Veterans Admnistration (VA) versus other external services. Thus, it has been possible to conclude that patients treated in VA centers showed a greater probability of receiving nephrological care prior to dialysis and having an AVF, although they had longer hospital admissions and longer durations and less access to kidney transplantation as comnpared to patients treated in outsourced centers21–24.
Erickson (2018)25 evaluated the association between competition in dialysis markets and levels of hospitalization and mortality in the US. Competition was measured using the Hirschman-Herfindahl (IHH) index, which ranges from 0 to 1, where a lower score represents a higher concentration of suppliers and, therefore, greater competition. A sample of 632,734 patients from 3379 dialysis centers between 2001 and 2011 was analyzed, with an average HHI index of 0.48. After adjusting for different variables, it was found that a reduction of 0.2 units in HHI was associated with a significant decrease in hospitalizations 2.9 per 100 patient/year, that is, an increase in competition between providers entails benefits for patients. patients. Competition that, however, was not associated with mortality (Table 1).
Characteristics of the included studies.
| Author | Aim | Methodology | Results |
|---|---|---|---|
| Lee (2010)18 | To determine the association between the purpose of the profit with the days of hospitalization. | Patients included in the USRDS registry on dialysis before January 1, 2003, without previous transplant and insured by Medicare. | It includes 170,130 patients in 3443 facilities, 9% being in non-profit facilities. Dialysis patients in for-profit facilities spent 17.5% more hospitalized days (p < 0.0001), this difference was maintained in the adjusted model. |
| Brunelli (2014)20 | To estimate the association between the profit purpose with the adjusted mortality and hospitalization. | Those included in the USRDS registry on dialysis during 2010, without previous transplants and insured by Medicare. | A total of 366,011 and 34,029 patients treated in for-profit and non-profit centers, respectively, were included. The crude hospitalization rate was higher in the population in lucrative centers (1.66 hospitalizations/patient-year) than in non-profit centers (1.59 hospitalizations per patient-year), not being significant in the multivariate model (p = 0 .69). The mortality rate was 23.1 and 22.0 for for-profit and non-profit centers respectively, this difference not being significant (p = 0.64). |
| Dalrymple (2014)19 | To study the relationship between the profit purpose of the dialysis center and the hospitalization rate. | Patients included in the USRDS registry on dialysis between 2005−2008 insured by Medicare. Those who received a transplant or recovered renal function were excluded. | The cohort included 150,642 patients, of whom 12,985 (9%) received their care at non-profit facilities. Hospitalization rates were significantly higher for patients receiving for-profit hemodialysis 15% (95% CI: 13%–18%) compared to nonprofit dialysis centers. |
| Fisher (2010)21 | To examine the effect of exclusive use of pre-dialysis services or not in outpatients. | Retrospective cohort with subjects who started dialysis in 2000 and 2001 and were eligible for VA and Medicare coverage in the 12 months prior to the start of dialysis. | A total of 1395 received VA services only, while 3093 used Medicare and 3545 used both. Those who used both services showed a greater probability of receiving pre-dialysis care (RR: 1.12; 95% CI: 1.07−1.17), with no differences with users of both services (RR: 0.98; 95% CI: 0.88−1.08). Likewise, those of VA (RR, 0.63; 95% CI: 0.50−0.81) and dual use (RR, 0.78; 95% CI: 0.70−0.88) were associated with a lower likelihood of late nephrology care (<3 months before the start of dialysis), compared with only Medicare users. |
| Hurst (2010)22 | Evaluate AVF use in national organizations versus the VA and DoD. | Cross-sectional study with patients who started dialysis between 2005 and 2006 and included in the USRDS. | A total of 129,525 patients who had centers for Medicare and Medicaid Services (CMS) available, of which 17,110 (13.2%) started HD with an AVF. Regarding care, 27.2% were treated in DoD, 18.5% employer group, 16.7% other insurance, 15.6% Medicare, 13% Medicaid and 8.2% uninsured. Those DoD started with a greater probability with an AVF (OR 1.82; 95% CI: 1.67−1.98) and less with a catheter (73.1 vs. 80.6%; OR 0.65; 95% CI: 0 .60−0.71), compared to the rest. |
| Parikh, (2011)23 | To determine differences in types of vascular access according to the different VA health care systems. | Cross-sectional study in patients that started dialysis between June 1, 2005 and May 31, 2006 included in the USRDS registry. | A total of 378 patients from 20 VA centers and 25,534 from 1631 non-VA centers were included. The study showed that a higher proportion of AV patients started dialysis with an AVF (20.9 vs. 11.6%; OR 1.70; 95% CI 1.31–2.20). This significant difference disappeared when adjusting for the pre-dialysis variables (OR 1.28; 95% CI 0.98−1.66). |
| Wang, (2013)24 | Evaluated differences in hospitalizations and mortality between veterans receiving dialysis in VA vs. no VA. | Retrospective cohort with subjects on dialysis between 2007 and 2008 included in the USRDS registry. Those who died in the first 90 days were excluded. | Of the total of 1388 veterans, 27% received dialysis exclusively at the VA, 47% at subcontracted centers, and 25% both types of centers. A 48% of the sample was hospitalized and 12% died. Those who received dialysis at VA were more likely to be hospitalized, compared to users who used both services and outsourced services (65, 30, and 63%, respectively, p < 0.001). Among those admitted to the hospital, in the VA the average stay (22.9 days) was longer than in those who used both services or the outsourced services (22.4 and 16.6 days, respectively), although differences were not significant (p = 0.146). |
| Erickson, (2018)25 | To examine whether market competition is associated with better health outcomes in hemodialysis. | Patients included in the USRDS registry on dialysis between 2001−2011. Patients who received dialysis in prison and in military centers were excluded. | A total of 632,734 patients (1,939,460 patient-years) receiving hemodialysis in 3379 hospital health areas were included. Those areas with less competition at the beginning became more competitive at the end. The annual probability of mortality was 20% (range 21−17), with a higher mortality in those less competitive, although it was not significant. The annual probability of hospitalization was 76%, with an average of 2.7 (SD 3.5) hospitalizations /year. An increase of 0.2 units in Hirschman-Herfindahl Index (IHH) is associated with 2.9 hospitalizations (95% CI 0.4−5.4). |
| Articles about costs | |||
| Conde-Olasagasti (2017)27 | Calculate the direct cost of renal replacement therapy in the province of Toledo between 2012 and 2013. | It was considered the consumption of resources of patients in RRT between 2012 and 2013 was. With this purpose, the following sources of information were used: the Registry of Renal Patients, economic management of hospitals, pharmacy and billing of concerts and transportation. | There were 668 patients included in 2012 and 682 in 2013. The average cost of the different therapeutic options was: HDH: 51,228, CHD: 44,814, PD: 48,704 and transplant: 10,946. The dialysis procedure represents 53, 55 and 54% of the cost of HDH, CHD and PD, respectively. |
| Parra-Moncasi (2011)26 | To estimate the effective cost of renal function replacement therapy with HD in end-stage chronic kidney disease in various centers. | Prospective study using analytical accounting that specifies the imputation criteria. | Six centres participated, two public centers (PC) and four subsidized centers. The cost/patient/year (excluding hospitalization and vascular access) for public centers were 42,547 and 39,289 and for subsidized centers were 32,872, 29,786, 35,461 and 35,294 (23% higher in public than in concerted ones). The highest percentage on the total cost were for the public 22.4% consumables, 21.7% nursing staff and 11.8% hospital pharmacy, while in subsidized centers they were 16.4% hospital pharmacy, 15% consumables and 14.1% for hospital pharmacy and nursing staff. |
| AETSA (2013)3 | To estimate the cost of the different modalities of dialysis based on data from hospital centers of the Public Health System of Andalusia. | Annual cost according to dialysis modality and healthcare setting, using measurements of activity related costs (ABC methodology), considering total healthcare costs from the perspective of the sponsor. The study was applied to a intercenter clinical management unit of the province. | The total annual cost of the patient care, without including the cost of the follow-up, was 43,395.40 in hospital HD vs. 38,815.77 for concerted HD. With an utilization rate of 47.81% and 52.19%,for HDH and CHD respectively. The total annual cost for the HD process amounted to 44,778.10 per patient (including follow-up estimated at 1,972.77). /year/patient). |
HD: hemodialysis; HDH: hospital hemodialysis; CDH: concerted hemodialysis; USRDS: United States Renal Data System; OR: odds ratio; RR: relative risk; 95% CI: 95% confidence interval; VA: Veterans Administration; DoD: Department of Defense; AVF: arteriovenous fistula; SD: standard deviation; : Euro; IHH: Hirschman-Herfindahl index; RRT: renal replacement therapy.
A report from the Agency for Health Technology Assessment of Andalusia analyzed the difference in costs between the modalities of hospital hemodialysis (HDH) (n = 256 patients) and concerted hemodialysis (HDC) (n = 226). The total annual cost, per patient and year, was 45,395.40 in HDH vs. 38,815.77 in HDC. This difference is mainly explained by the much more complex structure existing in the hospital compared to the centers where concerted dialysis is performed, and which represents an increase in direct costs of 6718.52 and 2573.03 in each of the modalities. Direct costs, for their part, are very similar in HDH and HDC, with 38,676.88 and 36,062.74, respectively3.
A multicenter cost study in two public owned and four subsidized, obtained an average cost of 40,136; ranging between 33,130 and 45,370 in the case of subsidized centers, and between 46,254 and 44,486 for public centers26. A similar distribution was found between the types of centers, except for spending on personnel, which was 37.3% of the total cost in public centers and 27.7% of the total in subsidized ones. By acontrast, other expenses (transport, management or maintenance) were higher in subsidized centers with 24.4% vs. 17.1% of those of public ownership.
In the study by Conde-Olasagasti27 it was estimated the cost of the dialysis program in Toledo during the years 2012 and 2013. The total cost of the treatment was 15,778,360, of which 40.1% corresponded to the dialysis treatment, 21.2% hospital charge (major outpatient surgery, outpatient consultations and emergency visits), 20.3% pharmacy, 10.1% transportation and 7.5% support (unscheduled HD sessions, PD training or unforeseen care at the day hospital). Thus, the cost per patient and year of HDH was 53,289 vs. the 44,971 of the HDC. The comparison of the different cost components reveals that the main cost difference between one modality and the other is in what is called the hospital charge, or expenses derived from direct medical care (HDH 9599 vs. HDC 6721), followed by of the cost of dialysis (HDH 27,289 vs. HDC 24,653). The part of the cost that transport, pharmacy or support represents in the total cost of each modality was not significantly different between hospital or subsidized HD (Table 1).
Public prices for hemodialysis sessions in SpainTable 2 shows the public prices for dialysis services in the different Autonomous Communities28–46, observing a wide difference in the time of the publication dates of the prices between June 2011, in Castilla y León, and March 2011. 2019, in Murcia. The public price ranged from 393.42 per hemodialysis session in La Rioja to 132.5 for the hemodialysis session in Andalusia (2015). In addition to the variability between the rates of the different regions, once the amounts are updated to 2020 using the Consumer Price Index (CPI), a notable diversity is observed in the name of the concept and type of dialysis, with a wide range of therapeutic options ranging from the "HD session" of the Basque Country or Castilla y León, to the detail of five different types of HD published by Aragon.
Public rates of the different Spanish Autonomous Communities.
| Description | Fare | Month and year of publication | Update 2020a | ||
|---|---|---|---|---|---|
| Basque Country37 | Hemodialysis session | 271.00 | February 2019 | 273.98 | |
| murcia36 | Hemodialysis session including laboratory tests and routine radiology | 209.67 | March 2019 | 211.98 | |
| MUFACE40 | Hemodialysis as outpatient regime (per patient/month) | 3610 | December 2014 | 3,761.62 | |
| Hemodialysis as outpatient regime per session | 251 | 261.54 | |||
| ISFAS39 | Hemodialysis as outpatient regime patient/month | 3610 | February 2014 | 3,754.40 | |
| Hemodialysis as outpatient regime per session | 251 | 261.04 | |||
| Madrid35 | Hemodialysis as outpatient regime patient/month | 3,610.00 | ]August 2017 | 3,707.47 | |
| Hemodialysis as outpatient regime per session | 278.00 | 285.51 | |||
| Hemodialysis in a concerted center | 140.00 | 143.78 | |||
| La Rioja34 | Cost of the dialysis session | 393.42 | December 2014 | 409.16 | |
| Galician33 | For each HD session in hospital centers both for hospitalized and outpatient the price of the hemodialysis session includes routine laboratory tests and transfusions that are performed after indication by the physician | 243.26 | April 2017 | 249.83 | |
| Extremadura32 | Hemodialysis (session) | 295.80 | January 2019 | 299.05 | |
| Valencia31 | Hemodialysis session | 235.17 | February 2018 | 240.11 | |
| Catalonia30 | Hospital (outpatient) hemodialysis (session) | 176.00 | February 2013 | 182.86 | |
| Supplement, online Hemofiltration (HDF) (session) | 36.00 | 38.52 | |||
| Castile and Leon46 | Hemodialysis session | 142.21 | December 2011 | 151.17 | |
| Club of Dialysis (according to treatment sessions) | ≤250 sessions | 160.91 | 171.05 | ||
| 251−390 sessions | 145.85 | 155.04 | |||
| 391−780 sessions | 142.51 | 151.49 | |||
| >780 sessions | 139.21 | 147.98 | |||
| Satellite center with health personnel from SACyL | 111.47 | 118.49 | |||
| Satellite center with personnel from the subsidized company | 130.95 | 139.20 | |||
| At the patient's home | conventional | 136.77 | 145.39 | ||
| short daily | 122.68 | 130.41 | |||
| Home dialysis with machine from the club of dialysis | conventional | 136.77 | 145.39 | ||
| short daily | 122.68 | 130.41 | |||
| Castile-La Mancha45 | Hemodialysis | 299.60 | November 2014 | 311.58 | |
| Cantabrian44 | Hemodialysis as outpatient regime (session). Treatments for patients with chronic renal failure undergoing dialysis programs on an outpatient basis. The price includes routine analysis and radiology, as well as the necessary transfusions. The price per session include the cost of erythropoietin | 221.00 | December 2017 | 226.97 | |
| Canary Islands43 | Hemodialysis session | 374.33 | April 2017 | 384.44 | |
| Balearic Islands29 | Hemodialysis session | 262 | January 2018 | 267.50 | |
| Asturias42 | Dialysis session | 162.69 | February 2019 | 164.48 | |
| Andalusia38 | Dialysis session | 132.50 | November 2015 | 139.66 | |
| Aragon41 | Hemodialysis in hospitals, includes the cost of bicarbonate concentrate | 140.00 | [4.0]August 2017 | 143.78 | |
| Standard hemodialysis, including the cost of bicarbonate concentrate | 140.00 | 143.78 | |||
| High-flow hemodialysis, including the cost of bicarbonate concentrate | 140.00 | 143.78 | |||
| OnLine hemodiafiltration, including the cost of bicarbonate concentrate | 160.00 | 164.32 | |||
| Hemodialysis at home with a machine (includes: hemodialysis material, dialysis liquid, dialysis monitors and own cardiopulmonary resuscitation material) | 137.90 | 141.62 | |||
| Ceuta and Melilla28 | Hemodialysis | 257.66 | July 2013 | 268.48 | |
MUFACE: General Mutual Society of Civil Servants of the State of Spain; ISFAS: Social Institute of the Armed Forces.
In an attempt to obtain evidence quickly and pragmatically, it was decided to use the scoping review, since it allows the inclusion of articles with different designs and outcome measures. The available evidence obtained from this review shows that in Spain that HDH is more costly than CHD and that in the US it has a lower rate of hospitalizations, with no significant differences in mortality.
On the other hand, the few results on effectiveness, measured by the aforementioned indicators, must be taken with caution due to the great heterogeneity of results and methodologies, and it should also be noted that they are obtained in a care framework that is so different in Spain vs USA, in which the modification of the care practice of for-profit centers prevails to conform to the contracts and/or obtain the maximum economic benefit47–49. The fact that all the studies on comparative effectiveness come from that country makes it difficult to extrapolate the results to our environment.
A striking finding is tha taking into account the economic and social importance, and the expected increase in dialysis patients there is a small number of publications on the comparative evaluation of concerted dialysis. Therefore it is difficult to offer a consistent and useful information base for decision making at the meso and macro management levels.
Other information and considerationsIt should be noted that there were found two systematic reviews that evaluated the quality of health care in a multitude of services in centers dependent of VA. These two reviews conclude that, in general, care at VA-operated facilities (eg, Medicare, Medicaid) is good or better than care provided by non-VA-operated or outsourced facilities50,51.
In terms safety of care, no article was found that evaluated differences in different areas of dialysis provision. In a 2017 study52, carried out in a Spanish hospital, all HD sessions were reviewed in two months (2149 in the hospital unit and 2125 in the peripheral center), detecting 11.8% of adverse events (AEs) in the hospital unit (12.9% high severity) vs. 9.2% in the peripheral center (1% high severity). The most frequent AEs were hypotension, in both cases, followed by extracorporeal circuit coagulation and AVF problems (hospital unit) and problems related to AVF puncture and extracorporeal circuit coagulation (in the peripheral center).
Roderick et al.6 asked the nursing staff the incidence of AEs observed in the last six weeks in 368 CHD patients. A 37.5% of patients did not have major adverse events, and of the 551 adverse events identified, the most frequent were: hypotension (48.8%), others (32.1%) and access problems (15.3%). These results are in line with the study by Arenas53 which found a proportion of adverse events in a CHD unit of 25.8%, the most frequent being hypertension (42.7%) and hypotension (27, 5%).
Balhara54 conducted a survey of 906 US nephrologists on the time they spent educating their CKD stage 4 patients. It was estimated at 20 min, the ideal time devoted to patient education on kidney transplantation. One of the results found that only 43% of professionals claimed to invest that time. In addition, it was found that those for-profit centers statistically showed less time dedicated to education (relative risk [RR] = 0.89) counseling (RR = 0.58), discussion about transplantation (RR = 0.58), family involvement (RR = 0.57), as compared to those without profit. This result is especially relevant, since patient training is a key element for patient autonomy and self-care55 and directly affects the results of the techniques and patient satisfaction.
Two studies were found In relation to the patient satisfaction according to the care received6,56. In both, greater satisfaction was found among HD patients in subsidized centers, being significantly higher in those aspects related to food, the appearance of the center, and the information received by health personnel.
Equity and continuity of care are shown to be key elements to obtain the maximum health results for dialysis patients; it is essential an appropriate coordination between subsidized centers and their reference hospitals, this allows standardizing the criteria for action, portfolio of services or techniques, procedures, etc.8.
In Spain, there are still no systematic and independent evaluations of the different forms of management, that could serve as a guide for future organization and management strategies57. It should be noted that the promotion of competition between centers (regardless of the legal form of management) could result in improvements25. Such a competition cannot arise spontaneously, given the quasi-monopoly characteristics that health centers have in their areas of influence, therefore it but must be generated by the request for services (in the case of private management) and by comparing results of efficiency and quality of care provided by the different centers57. Thus, the health outcomes of dialysis patients should not be conditioned by the ownership (public or private) of the health centers.
The great variability between the prices of the Autonomous Communities could be explained by the differences in the concepts included or different methodologies for their calculation, and also because they are not reflecting the real costs of the treatment58. A study carried out in Galicia concluded that HD concerts generated added value (economic growth and jobs) for the healthcare area, much higher than PD concerts59. This result highlights the need to carry out a more exhaustive evaluation that includes different dimensions and perspectives, using a multi-criteria decision analysis as a novel methodology that allows to perform and evaluation with a more holistic and transparent perspective.
The treatment of kidney disease has a high impact on health systems; the percentage of healthcare spending ranged between 1.3 and 3% of total healthcare cost, and it is higher in countries with lower incomes. These patients representing only 0.02−0.03% of the general population1,60. In 20 years, it is estimated that a third of the population will be ≥65 years of age, which could be translated into an increase in the prevalence of patients on RRT of 41% in the next two decades61. All of this highlights the need to use strategies that manage to reduce the economic burden of CKD, through programs to prevent the progression of the disease, together with the promotion of PD62. Thus, the coexistence in Spain of public and subsidized centers, the variability in the provision of dialysis techniques and the scant evidence on whether the outsourcing of RRT is an adequate plan to reduce treatment costs, illustrate the need to dedicate efforts and means to perform comparative investigation of results for the application of strategies that result in an improvement of care for chronic kidney disease, within the strategies of chronic diseases63–65.
Author contributionsAOL and ACM contributed substantially to the conception, design, analysis, and interpretation of the data, with assistance from MdAGV. AOL designed the search strategy and the data dump sheet. All authors have participated in the preparation and critical revision of the manuscript with important contributions, approved the final content and agreed to be responsible for all aspects of the work.
FinancingThis work has not received any type of funding.
Conflict of interestsThe authors declare that they have no conflict of interest.
Camila Higueras Callejón, librarian from the Andalusian School of Public Health, and David Epstein from the Faculty of Economics of the University of Granada.