La peritonitis esclerosante encapsulante (EPS) representa una complicación rara de la diálisis peritoneal (DP) con una alta mortalidad. Se caracteriza por la fibrosis difusa de la membrana peritoneal que progresa a encapsulamiento y se manifiesta con signos y síntomas de obstrucción intestinal. Su incidencia varía desde el 0,7 al 3,3 %. El factor de riesgo más importante en su desarrollo es el tiempo de exposición a las soluciones de DP, aunque posiblemente la edad joven y los episodios de peritonitis puedan contribuir. Su etiopatogenia no está claramente dilucidada y se cree que, sobre una membrana peritoneal lesionada, un segundo estímulo (second hit) como las peritonitis, hemoperitoneos, cirugías, predisposición genética, etc., puedan desencadenar el desarrollo de EPS. Algunos casos aparecen tras la transferencia a hemodiálisis o tras el trasplante, lo que quizá tenga relación con el uso de inhibidores de la calcineurina. La presencia de síntomas y signos de obstrucción intestinal, junto con los hallazgos radiológicos y/o anatómicos compatibles, permiten confirmar el diagnóstico. Su detección precoz es imprescindible, aunque en la actualidad no existen marcadores clínicos ni bioquímicos capaces de predecir su aparición. En el manejo terapéutico se emplean inmunosupresores como los esteroides y el tamoxifeno, la nutrición y, en casos más avanzados, la cirugía de adhesiolisis, con resultados variables. En esta revisión se discute el diagnóstico y tratamiento de la EPS, se promueve la participación en el Registro Europeo y se aboga por la necesidad de centralizar el manejo de esta complicación.
Encapsulating peritoneal sclerosis (EPS) represents a rare complication in peritoneal dialysis (PD) with high mortality. It is characterised by diffuse peritoneal membrane fibrosis, which develops into encapsulation and manifests as clinical signs and symptoms of intestinal obstruction. Its incidence varies from 0.7%to 3.3%. The most significant risk factor in its development is exposure time to PD solutions, although young age and peritonitis episodes can also contribute. Its aetiopathogeny has not been clearly explained and it is thought that a second hit like peritonitis, hemoperitoneum, surgery, genetic predisposition, etc on an already damaged peritoneal membrane, could also trigger the development of EPS. Some cases appear after transfer to haemodialysis or after transplant. In these cases, the use of calcineurin inhibitors is believed to be related. The presence of clinical symptoms and signs of intestinal obstruction, along with compatible radiological and/or anatomical findings could also confirm the diagnosis. At present there are no clinical or biochemical markers capable of predicting its onset. Therapeutic management comprises the use of immunosuppressors like steroids and tamoxifen, nutritional management and even surgery in advanced cases, all of which provide varying results. This article discusses the diagnosis and treatment of EPS, it encourages the participation in the European Registry and it advocates the need to centralise the management of this medical complication.
INTRODUCTION
Encapsulating peritoneal sclerosis (EPS) is an uncommon but severe complication of peritoneal dialysis (PD) that was described for the first time in 1980 by Gandhi,1 and is characterised by the presence of an inflammatory reaction and fibrosis in the peritoneum that produces recurrent, intermittent, or persistent symptoms of intestinal obstruction.2,3
We have no reliable estimate of the incidence of this condition, but studies have reported rates of 0.7% to 3.3%,3-11 with a progressive increase in incidence with longer durations of time on PD. In Spain, no reports have been published on the global incidence of this disease. In 2007, the Hospital Severo Ochoa in the autonomous community of Madrid reported 8 cases during a 17-year period, with a 4.2% incidence rate and a survival rate 1 year after diagnosis of 51%.12
The majority of the available information regarding this disease comes from other European countries and Japan in particular, where the percentage of patients on PD is high, with long durations of time spent on this dialysis technique. Little information is available from America and Spain, and it is possible that certain factors such as the overall percentage of patients on PD, the mean duration of treatment, and the rate of exit from this modality of dialysis, above all in centres where a large proportion of patients receive kidney transplants, could influence the variability described in the incidence of EPS between different countries.
In 2009, a Dutch initiative was started to recognise the status of EPS as a rare disease and to create an European registry. This registry is based out of the HansMak Institute located in the city of Naarden (Netherlands). This initiative was originally promoted by an association of Dutch and British nephrologists, with the addition of other European countries (Belgium, France, Germany, Italy, Sweden, and Spain) in the last year. The goal of this initiative is to achieve advancements in our understanding of the pathophysiology of EPS through registration and monitoring of definitive or suspected EPS cases in order to develop uniform criteria for diagnosing and managing this disease. The initiative also set the goal of collecting samples of serum, plasma, blood and peritoneal effluent.13
Our goal with this article is to promote awareness of this disease and participation in the European registry of EPS.
RISK FACTORS FOR ENCAPSULATING PERITONEAL SCLEROSIS
EPS is most likely a multifactorial process, in which various factors simultaneously occurring in the body act as a trigger. The duration of treatment on PD is the most closely related factor to the development of EPS, probably because this reflects the time during which the peritoneum has been exposed to the negative effects of dialysis solutions.9,10 The incidence of EPS increases with the accumulation of more years actively on PD, and a large portion of cases arise after PD has been ceased.
In addition, exposure to glucose-based PD solutions that are not free of glucose degradation products (GDP) produces increased peritoneal damage, and greater cumulative exposure to these products is associated with a higher risk for EPS, regardless of the duration of time spent on PD.14
This has led to the development of new biocompatible PD solutions with a lower content of GDP, and in vitro and animal studies have demonstrated that these solutions preserve the peritoneal membrane and increase the viability of mesothelial cells,15,16 which in turn could signify a decreased incidence of EPS in the future. This proposition requires corroboration, and a multi-centre prospective clinical trial (NEXT-PD) is currently underway in order to evaluate the incidence of EPS in patients on PD using biocompatible solutions.17
Other PD solutions have also been associated with the development of EPS. For instance, the use of icodextrin has been associated with EPS in observational studies,14,18 but no clear evidence exists either to refute or support this conclusion, since the majority of patients who develop EPS in these studies were exposed to icodextrin due to ultrafiltration failure (UFF). UFF could be considered as a factor associated with the development of EPS, or even an early manifestation of the disease. With this in mind, exposure to icodextrin could be considered more a consequence EPS than the cause.
Peritonitis episodes7,19,20 have also been consider to be a risk factor.21,22 UFF and a high-transport status are also very common in patients with EPS, and have been associated with the development of this disease.14,23,24
Another factor that has been related to EPS development is patient age at the start of PD. Observational studies have suggested that younger patients are at a greater risk for EPS, regardless of the time on PD and follow-up, but this may be related to the fact that these patients spend a longer period of time on PD. On the other hand, younger patients have a greater capacity to repair tissue damage induced by chronic exposure to dialysis solutions, which resulting in a higher degree of peritoneal fibrosis and thus a greater risk for developing EPS.3,25
PATHOGENESIS OF ENCAPSULATING PERITONEAL SCLEROSIS
Chronic exposure to PD solutions leads to the development of simple peritoneal sclerosis, which is characterised by thickening of the parietal wall and vascular alterations (without encapsulation).3,26,27 There is a certain amount of controversy in the medical literature regarding whether EPS is a distinct entity from the simple fibrosis/sclerosis that occurs in patients on prolonged treatment with PD. In EPS, peritoneal sclerosis plays an important role, but alone does not appear to reflect the progression of the disease, requiring the presence of a “second hit” that acts as a trigger.3,28 EPS is more common in patients that have been on PD for longer periods of time, but does not appear universally in all cases, pointing towards the existence of currently undefined factors that predispose certain patients to developing this condition. It is believed that episodes of peritonitis, intense or repeated haemoperitoneum, abdominal surgery, exit from PD, and genetic predispositions could be implicated.2,3,28
Post-kidney transplant encapsulating peritoneal sclerosis
A substantial proportion of cases of EPS occur following a kidney transplant, and these usually manifest shortly after the transplantation. This association tends to appear in patients who start PD at a younger age, and is not necessarily correlated with prolonged exposure to PD, which has led to the suggestion that this is a different entity from the more general form of EPS.18,24,29 The exact cause of this relationship is unknown, although several hypotheses have been set forth. According to the “double hit” theory, the peritoneal membrane is first damaged by chronic exposure to PD solutions, and then a “second hit” occurs in the form of a kidney transplantation, thus triggering EPS. It is possible that PD cessation and interruption of peritoneal lavages, with the consequent accumulation of pro-fibrotic factors, could also be capable of triggering EPS.29 Another factor that has been suggested in the development of this pathology is the concomitant use of calcineurin inhibitors such as tacrolimus and cyclosporine, both of which are capable of increasing the expression of transforming growth factor β (TGF-β), and consequently are capable of increasing the rate of fibrosis.30 The use of cyclosporine A in a rat model of individuals on PD and exposed to dialysis solutions led to an increased development of fibrosis, vascularisation, and inflammation, with similar lesions to those observed in cases of EPS.31 The pathogenic role of these drugs in post-transplant EPS has still yet to be confirmed.
DIAGNOSING ENCAPSULATING PERITONEAL SCLEROSIS
Currently, the diagnosis of EPS is based on the criteria proposed in 2005 by the International Society for Peritoneal Dialysis (ISPD), which include: 1) the presence of clinical symptoms with varying degrees of systemic inflammatory reaction, and 2) radiological findings compatible with a diagnosis of EPS (peritoneal thickening, calcification, intestinal obstruction, and encapsulation).32
Clinical presentation
Gastrointestinal symptoms are essential to the diagnosis of EPS; anorexia, loss of appetite, nausea, and vomiting are common symptoms in the early phases of EPS. In general, symptoms tend to be vague and insidious, occurring intermittently and making the diagnosis of EPS easily confused with other disorders. These symptoms can also be accompanied by elevated concentrations of inflammatory markers (C-reactive protein), hypoproteinaemia, and haemorrhagic ascites in 7%-50% of cases.2,3,19,32 In later stages, constipation, abdominal mass, and abdominal pain can also appear.3,19,32
The properties of the peritoneal membrane are usually evaluated using a peritoneal equilibrium test, and a progressive deterioration in UFF and high transport of solutes can be observed in patients with EPS.14,23,24
Diagnosis based on imaging tests
Abdominal x-rays are not particularly useful, since the findings are not specific; only in advanced stages may peritoneal calcification and signs suggestive of ileus be observed, such as dilated bowel loops and air-fluid levels.33
An abdominal ultrasound may reveal peritoneal thickening, loculated ascites, adherences, rigid and dilated bowel loops, and decreased peristalsis. This is a non-invasive and cheap diagnostic technique, but the accuracy is operator-depedant, and at this point there is no information available regarding the sensitivity or specificity of this technique for diagnosing EPS.33
Computerised tomography scan (CT) is currently the best imaging technique for confirming the diagnosis of EPS, and this procedure must be carried out by an experienced radiologist. Several studies have demonstrated the usefulness of CT scans for the diagnosis of EPS,34-36 and a classification system has been proposed based on CT results using the following parameters: peritoneal thickening and calcifications, bowel loop dilations and loculated ascites, thickening of the intestinal wall, and intestinal encapsulation, reaching a sensitivity of 100% and a specificity of 94% when three of these criteria are positive as assessed by an experienced radiologist.36 One limitation of CT scans that has been demonstrated by various studies is the lack of definitive diagnostic capability in cases of asymptomatic EPS.37
Magnetic nuclear imaging (MRI) is a potentially useful tool, with similar results to scans, although the usefulness of MRI in diagnosing EPS has not been examined.33 MRI does present the advantage of avoiding exposure of the patient to radiation, but the higher costs, lack of availability, and the risk of nephrogenic systemic fibrosis as the result of using gadolinium-based contrast dyes all limit the acquisition of experience using this technique.33 Recently, cine-MRI was developed consisting of MRI images obtained from different phases of the respiratory cycle, which are subsequently reconstructed using a special software in order to observe the movement patterns of the intestinal loops; this technique could facilitate the detection of changes in patients with EPS, although its usefulness for this purpose has not yet been demonstrated.38
Positron emission tomography may also be useful for establishing a diagnosis of EPS during the inflammatory phase, during which an increase in the peritoneal uptake of the tracer can be observed, but the use of this technique is limited due to the lack of specificity of these findings, which can also be observed in cases of acute peritonitis.33
Histological diagnosis
A definitive diagnosis of EPS is made through direct observation and a histological analysis, which can be obtained during surgery or post-mortem. A laparotomy may reveal the presence of peritoneal thickening, adherences, total or partial encapsulation of intestinal loops, and in very advanced stages, a fibrotic layer may cover and encapsulate the entire intestines; the root of mesentery may also show signs of fibrosis and retraction.39,40
From a histological point of view, the most common morphological changes in EPS are a complete loss of the mesothelium, with substantial thickening of the peritoneal membrane, interstitial fibrosis, dense layers of fibrous connective tissue with infiltration of mononuclear and polymorphonuclear cells, angiogenesis, increased number of capillaries, increased fibrin concentrations, exudation, ossification, and calcification.39,40
Molecular diagnosis of the peritoneal effluent
Research into the identification of early markers of EPS is a promising field of investigation, although the majority of studies have been based on animal models, with experience in human subjects being limited to small and retrospective studies. A group from the United Kingdom, under the Global Fluid Study initiative, prospectively collected samples from incident patients on PD with the goal of using proteomic, metabolomic, and genetic techniques to search for possible markers for EPS. There is also a biological bank being maintained in Germany of approximately 200 samples of peritoneal biopsies from patients on PD for this same purpose.13
Early diagnosis
Until now, no single biochemical marker or radiological test has been established that to help identify patients with risk of developing EPS. Changes in peritoneal function may only be the reflection of long exposure to PD, and have not clearly show to be useful in establishing an early diagnosis. However, it has been shown that patients who develop EPS tend to have UFF prior to PD stop,14 and that remaining on PD after acquiring UFF increases the risk of developing EPS.23 The use of imaging tests such as CAT scans in asymptomatic patients is not indicated, since many patients develop EPS even with a normal CAT scan recently taken (within less than one year).37
The need for an early diagnostic protocol has led to the search for possible markers found in the peritoneal effluent. All cytokines and growth factors involved in the processes of peritoneal fibrosis and angiogenesis could potentially be markers for EPS. Certain mediators such as cancer antigen 125 (CA125), which is produced by mesothelial cells and serves as a marker for the mass integrity of mesothelial cells, as well as other cytokines such as interleukin (IL) 1β, IL-6, IL-8, transforming growth factor β1 (TGF-β1), and platelet-derived growth factor have been examined in the peritoneal effluent of patients with EPS. Very low levels of CA125 have been observed in the peritoneal effluent of patients during the years prior to developing EPS, as well as elevated levels of IL-6.25 This led the group of Sampimon et al. to investigate the use of combined measurements of IL-6 and CA125 in a group of patients with EPS and in a control group, resulting in a specificity of 89% but a sensitivity of 70%, with larger cohort studies needed in order to validate these findings.25
CLASSIFICATION OF ENCAPSULATING PERITONEAL SCLEROSIS
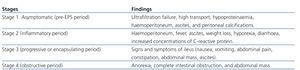
The development of EPS has been divided taking into account clinical and pathological findings into 4 stages, proposed by Nakamoto et al. (Table 1). The pre-EPS stage is characterised by the presence of UFF and/or altered solute transport status; this is followed by inflammatory, encapsulating, and obstructive phases, the last of which is characterised by intestinal obstruction and the formation of a “cocoon”.2
CONSEQUENCES OF ENCAPSULATING PERITONEAL SCLEROSIS
The initial symptoms of abdominal pain, nausea, vomiting, and anorexia can progress towards partial or complete intestinal obstruction, and these disorders can lead to malnutrition, infection, and death. The mortality rate of EPS is high, reaching 50% (especially during the first year), and increases with duration of time spent on PD.2-3,32
TREATMENT MANAGEMENT FOR ENCAPSULATING PERITONEAL SCLEROSIS
General treatment measures
Following diagnosis, discontinuation of PD is one of the initial treatment strategies, although in certain cases, this might actually aggravate the clinical symptoms, as demonstrated by the high frequency of cases of EPS that manifest following patient transferral to haemodialysis or following kidney transplantation.32 When PD is discontinued, the peritoneal catheter must also be removed. Leaving the peritoneal catheter in order to continue regular peritoneal lavages in order to remove fibrin and inflammatory mediators was not shown to be an effective strategy in a multi-centre prospective study.39 In this study, bacterial peritonitis episodes due to peritoneal lavages had the reverse effect to that intended, which predisposed patients to developing EPS,39 although this should be an avoidable complication.
Nutritional support is a crucial component of the treatment of advanced cases in order to prevent malnutrition, in association with other therapeutic strategies.40,41 Patients with EPS generally experience a weight loss >10%, which is correlated with worst outcomes; in many cases, body mass index may remain within normal limits, but more than 50% of patients experience a loss of appetite and gastrointestinal symptoms.40
Malnutrition in these patients is associated with higher mortality and morbidity rates, and in the case of surgery, nutritional support has been shown to improve postoperative patient evolution, with equal efficacy obtained using either parenteral or enteral nutrition, which should be maintained until the patient mantains an adequate oral intake.41
Corticosteroids
Corticosteroids are the most commonly used drugs for the treatment of EPS. It is believed that corticosteroids may be able to suppress the peritoneal inflammatory process and inhibit the synthesis of collagen due to their anti-inflammatory properties. However, the isolated use of corticosteroids in patients with EPS was effective in only 38.5% of cases in a prospective study,42 although other studies have reported cases in which early treatment with corticosteroids was associated with dramatic responses.43-45 So the use of corticosteroids only seems appropiate in early stages of the disease and in patients with signs of peritoneal inflammation, with lower response rates obtained in patients with more chronic damage and a greater level of fibrosis.
Tamoxifen
Tamoxifen is a selective inhibitor of oestrogen receptors with the potential for anti-fibrotic effects, and is capable of inhibiting the production of TGF-β by fibroblasts, which has been successfully used to treat syndromes such as idiopathic retroperitoneal fibrosis.46,47 In case reports and small studies, tamoxifen has been used alone or in conjunction with corticosteroids with satisfactory results.48-50 Furthermore, its use has been extended to patients on PD for long periods of time with high peritoneal transport27 as a preventive measure with promising results, although controlled randomised studies are needed in order to confirm the efficacy of this strategy. In a recent retrospective study in Holland, mortality rates were lower in cases of EPS treated with tamoxifen.48 Potential adverse effects related to the use of tamoxifen, such as increased frequency of thromboembolic events and risk of endometrial cancer, must be taken into account, although the frequency of these side effects are low if we consider the low doses of tamoxifen (1040mg/day for 1 year) that have been used to treat these cases.
Surgical treatment
The surgical treatment for EPS is adhesiolysis, a simple procedure in which adherences and fibrotic tissues are released, which requires separating fibrin membranes from the visceral peritoneum that surrounds the small intestine.51,52 This intervention may revert the intestinal obstruction, but it does not improve the deterioration of the peritoneum, which can continue to progress with renewed formation of a fibrotic capsule and recurrence of symptoms within as short a period as 6-12 months; in addition, as a result of the lesion produced by the surgical procedure, new adherences may also develop.53,54 The group headed by Kawanishi has reported substantial experience with this surgical technique, in addition to new complementary surgical methods designed to reduce the frequency of recurrence following the procedure, such as Noble’s operation (plicature), in which the intestinal loops are sutured together in order to prevent later cases of reobstruction.55,56 Their results in 180 cases of EPS treated surgically showed survival rates reaching 81% after 5 years, and with a rate of recurrence following the first operation of 22.4%.54 Surgical interventions is essential in the treatment of cases with intestinal obstruction. In order to improve surgical results, local reference hospitals and experienced surgical teams are needed.
GENERAL CONCLUSIONS
EPS is an uncommon but very severe complication of PD that is associated with high mortality rates. The aetiopathogenesis of this condition is still unclear, and at present, no early markers have been identified for use in predicting the risk of a given patient on PD for developing EPS.
Recent advancements in PD, including systematic use of biocompatible solutions, allow for postulating that certain mechanisms that could be implicated in the development of EPS may be relics of the past. However, there is low evidence to suggest this trend, and further collaboration is needed in order to better understand this disease that, due to its rarity, facilitates only limited individual experience.
The vision of the European EPS registry will hopefully aid in taking us closer to these objectives (Figure 1). We must work together in a concentrated fashion by incorporating all of our cases of EPS into the European registry.55
Conflicts of interest
The authors declare that they have no potential conflicts of interest related to the contents of this article.
Table 1. States of encapsulating peritoneal sclerosis and clinical manifestations
Figure 1. European registry of encapsulating peritoneal sclerosis