Antecedentes: Existen datos sobre una diferente situación laboral entre pacientes bajo diferentes modalidades de tratamiento renal sustitutivo (TRS). Objetivos: Comparar los costes indirectos por morbilidad en TRS: hemodiálisis (HD) en centro especializado, diálisis peritoneal automatizada (DPA), diálisis peritoneal continua ambulatoria (DPCA) y trasplante renal (TX). Métodos: Análisis de costes indirectos por morbilidad en TRS siguiendo la teoría del capital humano. Se incluyeron 243 pacientes en edad laboral (32 DPCA, 46 DPA, 83 HD y 82 TX) evaluados en 8 centros. Se estimaron el coste por pérdida de productividad laboral (CPPL) para el año 2009, los años de vida laboral potencialmente perdidos hasta la jubilación (AVLP) y el coste total de CPPL hasta la edad de jubilación (CPPL total) ajustados por edad y sexo. Las diferencias en costes se contrastaron mediante remuestreo con 1.000 simulaciones de las diferencias siguiendo el método simple corregido de los percentiles. Resultados: No se encontraron diferencias significativas en edad o sexo entre grupos. El CPPL (2009) en HD (6547 € [intervalo de confianza (IC) al 95%: 5727-7366 €]) fue significativamente mayor (p < 0,001) que en TX (5079 € [IC 95%: 4127-6030 €]) o DPA (4359 € [IC 95%: 3064-5655 €]), pero no que en DPCA (5785 € [IC 95 %: 4302-7269 €]). Los AVLP fueron: HD 12,58 años (IC 95%: 10,42-14,73); TX 10,05 años (IC 95%: 7,45-12,65); DPA 6,09 años (IC 95%: 3,43-8,74); DPCA 10,69 años (IC 95%: 6,14-15,23). Las partidas medias del CPPL total también fueron más altas en la HD que en el TX, la DPA o la DPCA en todos los escenarios contemplados. Conclusiones: El TX y, en especial, la DPA son las estrategias de TRS con menor impacto en costes indirectos asociados a morbilidad, presentando mayores tasas de ocupación y requiriendo menores recursos de prestaciones por incapacidad laboral.
Background: There is evidence of a different employment status between patients undergoing different modalities of renal replacement therapy (RRT). Objectives: The present study aims to compare the indirect costs associated with morbidity in the following RRT alternatives: haemodialysis in a specialised center (HD), automated peritoneal dialysis (APD), continuous ambulatory peritoneal dialysis (CAPD), and kidney transplant (TX). Method: We analysed indirect costs following the Human Capital Theory. In total, 243 patients of working age were included (32 CAPD, 46 APD, 83 HD, and 82 TX) from 8 hospitals. The potentially productive years of life lost (PPYL), the costs of lost labor productivity (LLPc) for the year 2009, and the total cost of PPYL (PPYLtc) until age of retirement were estimated. All estimations were adjusted by age and sex. Non-parametric analysis (bootstrap confidence intervals of differences in costs calculated following the simple bias-corrected percentile method -1,000 estimates-) was computed to highlight differences in costs. Results: No significant differences were found in age or sex between groups. In 2009, LLPc for HD (6547€; 95% CI: 5727€-7366€) was significantly higher (P<.001) than for TX (5079€; 95% CI: 4127€-6030€) or APD (4359€; 95% CI: 3064€-5655€), but not CAPD (5785€; 95% CI: 4302€-7269€). PPYL values were: HD: 12.58 years, 95% CI: 10.42-14.73; TX: 10.05, 95% CI: 7.45-12.65; APD: 6.09, 95% CI: 3.43-8.74; CAPD: 10.69, 95% CI: 6.14-15.23. PPYLtc was higher in HD than in TX, APD or CAPD in all scenarios tested. Conclusions: APD and, to a lesser degree, TX are the modalities of RRT with the lowest impact on indirect costs due to morbidity, resulting in higher rates of employment than HD and requiring less disability benefits.
INTRODUCTION
Chronic kidney disease (CKD) is one of the major public health issues in modern medicine, since approximately 9%-10% of the population has an estimated glomerular filtration rate (eGFR) <90ml/min/1.73m2, and 0.3% already suffer symptoms of advanced renal failure1 in stages 4-52 (eGFR<30ml/min/1.73m2). It is reasonable to expect that these proportions will increase in our population, along with independent factors such as obesity, age, and hypertension.1 However, based on the reports released by the Spanish Society of Nephrology (S.E.N.), the national incidence rate of renal replacement therapy (RRT) appears to have experienced a slight reduction in recent years (going from 132 individuals per million population [pmp] in 2000 to 129pmp in 2009 and 119pmp in 2010), although the prevalence rate still continues to increase, situated at 1033pmp in 2010.3
In more advanced stages of CKD, when the patient progresses with chronic renal failure to the uraemia period, some method of replacing the lost renal function must be applied. Although this proportion of patients requiring RRT is small, the health resources required for their treatment are greater than for other, more prevalent chronic pathologies.4
As regards the available RRT alternatives, the scientific studies published in this field point towards kidney transplants (TX) as the overwhelming method of choice in terms of costs and benefits.5,6 Among the remaining alternatives (haemodialysis [HD] in the home, in a hospital ward, or in a specialised dialysis unit, continuous ambulatory peritoneal dialysis [CAPD], and automated peritoneal dialysis [APD]), clear discrepancies can be found. Differences in efficacy and utility health states associated with each alternative were reported, as well as related costs,7 as well as implied costs.4,8-12 A recently published study in our country regarding the possible short-mid-term superior results of peritoneal dialysis (PD) over HD13 in incident patients on RRT added new arguments to the previous studies regarding the pharmacological and economical benefits of the former in terms of efficiency in dialysed patients.6,14,15
Within the current socioeconomic context, studies examining costs of treatment are especially relevant for quantifying the magnitude of the health care issue faced by the public administration.4,15 In addition, these studies provide useful information to health care managers regarding the effects of the various treatment strategies available.16,17 In this sense, the objective of our study was to complement the analysis of employment situation among patients on RRT that was recently published18 with an estimation of the indirect costs associated with each different modality of RRT. In the aforementioned publication, the authors found that there is a greater proportion of actively treated patients in Spain on PD or with a TX than on HD, as has also been reported for nearby countries.19-21 Our study focuses on estimating the social costs implied by this employment situation for patients on the different RRT methods.
METHOD
We performed an analysis of the indirect costs associated with morbidity from a social perspective following the human capital theory.17,22,23 Usually, indirect cost analyses include an economic quantification of all potential losses in productivity caused by the disease. Then, in a social perspective, morbidity and mortality costs related to the disease under analysis should be considered. However, we were exclusively concerned with economic losses related to the loss of patient capacity for involvement in gainful employment due to morbidity. Specifically, in order to estimate the indirect costs associated with lost labour productivity, we used an approximation based on the mean annual income value established by the Salary Structure Survey from 2006, which was carried out by the National Statistics Institute Incomes were inflated to 2009 prices using consumer price index.
We based our analysis on the information compiled in the multi-centre, cross-sectional study carried out by the National Federation of Associations for the Fight Against Kidney Disease (ALCER) in 8 hospital centres from various autonomous regions (Catalonia, Madrid, Castile and Leon, Andalusia, and Basque Country). A total of 269 patients on RRT were interviewed between August 2007 and May 2009.18 The different modalities of dialysis treatment assessed included TX (n=88), HD (n=99), APD (n=47), and CAPD (n=35). Once patient age was reviewed, the study included a total of 243 patients of working age (in 2009, this corresponded to ages between 16-65 years).
In addition to basic clinical and sociodemographic characteristics, we formulated the following dichotomic (yes/no) questions regarding employment situation: -Are you actively employed and receiving a salary? -Do you receive some type of stipend due to permanent worker’s disability (PWD)? -If you do not work or receive a stipend due to PWD, do you receive disability benefits? -Do you possess a certificate of disability greater than 33%?
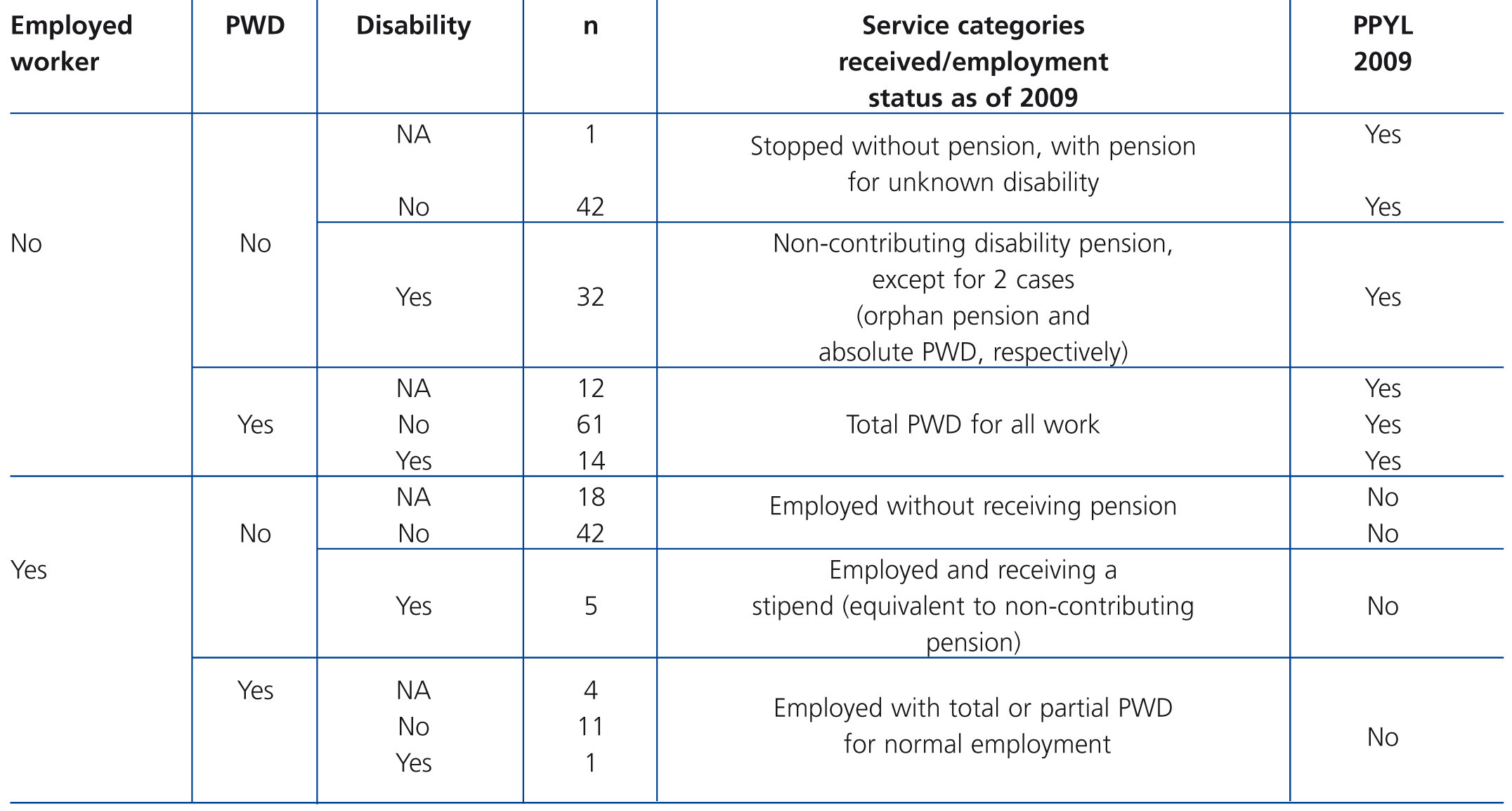
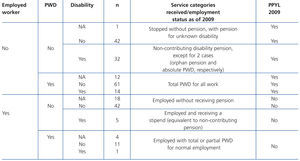
Since the responses to these questions do not allow to establish the specific employment situation of each person and the benefits they receive, we then performed a complementary review of the observations of each of the 243 patients in order to classify these into different employment categories (Table 1). We then inferred the lost labour productivity within each category, assuming that patients who continue to work and receive a salary regardless of type of employment, would not suffer any loss in labour productivity that year (Table 1). Using this information with adjustments for age and sex, we estimated the cost of lost labour productivity due to morbidity (LLPc) for each group of patients in 2009. We also took patient age at the time of the interview into account to calculate potentially productive years of life lost (PPYL) until reaching retirement age assuming that the current employment status is sustained. Using the LLPc and PPYL values for 2009, we estimated total lost labour productivity (overall LLPc) for each modality of RRT analysed (TX, HD, CAPD, and APD). In order to evaluate total losses due to patient morbidity, we took into account the values associated with lost productivity in 2009 (regardless of the time that each patient had spent in their current employment situation or when it started) and estimated a projected value leading up to retirement age, assuming that the rate of activity would remain constant within this sample (rate of activity among patients with physical disabilities: 35.8%. Source: National Statistics Institute, 2008).
Statistical analysis
We performed a descriptive analysis of the sample (with frequencies and percentages for categorical variables and central tendency/dispersion for continuous variables). In order to evaluate inter-group heterogeneity, we evaluated differences among the different modalities of RRT in terms of variables of interest such as sex, employment situation, benefits received, and age. χ2 tests were applied for analysing categorical variables and Kruskal-Wallis and Mann-Whitney U-tests (with Bonferroni corrections) for continuous variables. χ2 tests were also used to examine the differences in percentages of patient activity and employment between study groups and the spanish general population24 and other reference groups (individuals with physical disabilities due to gastrointestinal, metabolic, endocrine, or cardiovascular diseases25).
We compared indirect costs using a bootstrapping technique with 1000 simulations of the differences between groups using a corrected simple percentile method.26 We used a statistical significance threshold value (α) of 0.05 in all statistical tests performed.
In addition to the bootstrapping method, we applied different rates of inflation/discounts in the calculation of LLPtc costs until the age of retirement for a sensitivity analysis: inflation rates for worker salaries (0%, 1%, and 3%) and discount rates projected from 2009 onwards (0%, 3%, and 6%), so as to be able to compare results between the different RRT options among different possible future scenarios. Finally, based on our estimates of costs associated with morbidity for the study reference year (2009), we estimated these same costs for future years (we presented projections until 2020), using a published model of the progression of disease14,15 that has been validated based on epidemiological values published by the S.E.N (time series: 1996-2008).
RESULTS
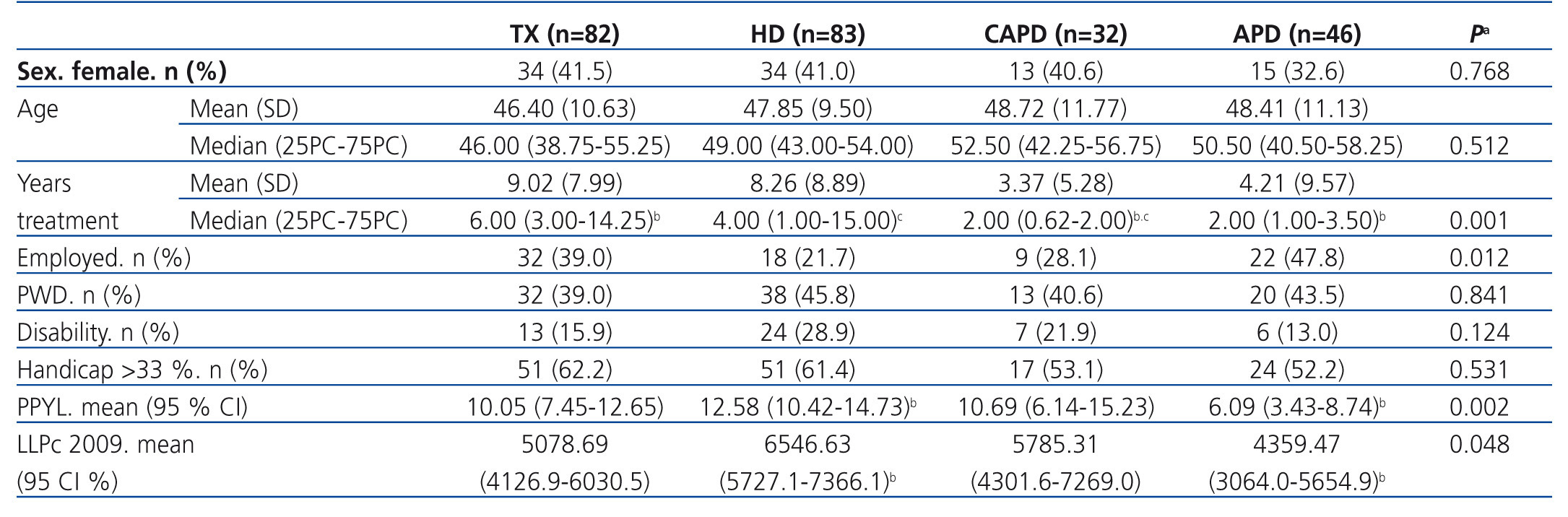
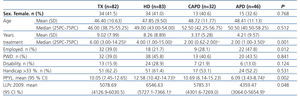
Of the 243 patients with CKD who were included in the analysis, 82 (33.7%) had received a TX, 83 (34.2%) were on HD, and, among the patients on PD, 46 (18.9%) were on APD and 32 (13.2%) were on CAPD. Mean patient age was similar among all groups, at 46-48 years (Table 2). The sex distribution was also similar among all groups, with a greater proportion of males (approximately 60%-65% of all patients evaluated). We did observe a difference between groups in terms of years on RRT, which was significantly lower in the group on CAPD (Table 2).
In terms of employment rate among the patients in our study, the resulting proportion was 33.3% (n=81), which was significantly higher (P<.05) than the values reported for the general population of individuals with disability (28.0%).25 In contrast, this percentage was similar (P>.05) to rates published for individuals with physical disability and similar conditions (31.1%),25 and to rates for the sub-group of patients with disabilities from gastrointestinal, metabolic, and endocrine diseases (32.5%).25 We also observed that male patients in our sample were employed at a significantly higher rate (χ2=6.993; P=.008) than females (40.14% vs. 22.92%). In comparison with the reference population of disabled individuals,25 females in our sample had approximately the same rate of employment (22.92% vs. 22.0%; P>.05), whereas the proportion of male patients with gainful employment in our study was significantly higher than in the reference population (40.14% vs. 32.8%; P<.001). On the other hand, as expected, the rate of employment in our study population was significantly lower than the global values published by the National Statistics Institute for 200924: 60.62% for the general population, 67.55% for males, and 53.54% for females (P<.001).
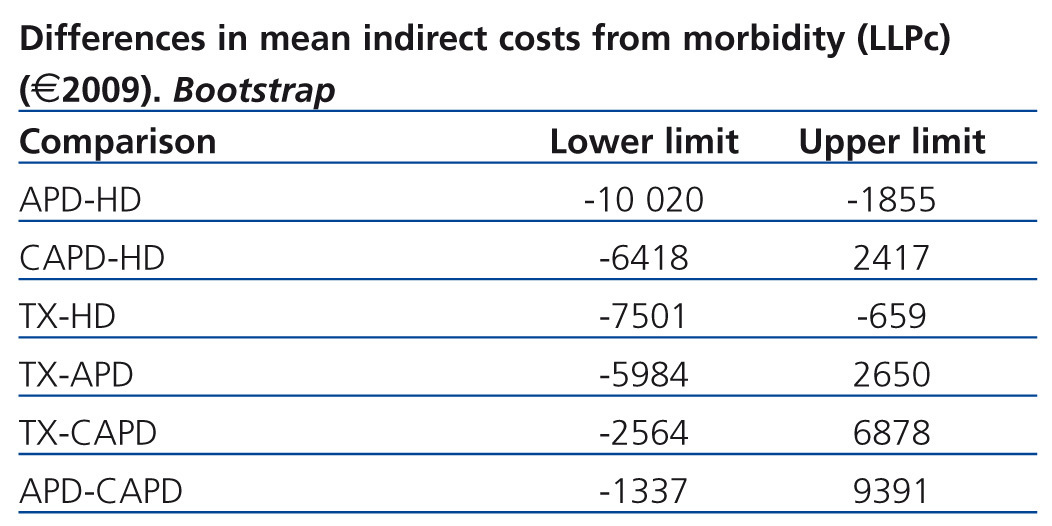
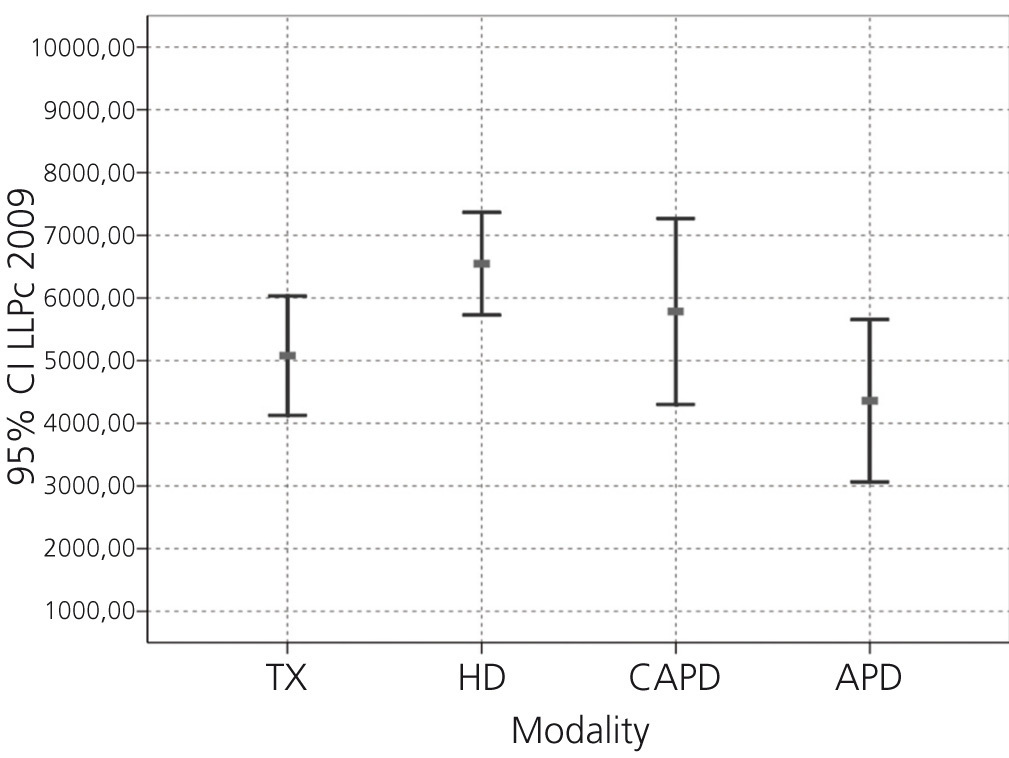
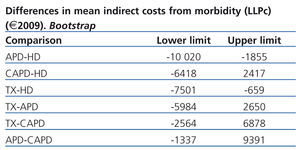
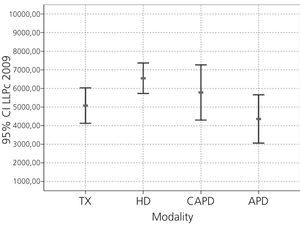
Based on employment status, we calculated PPYL associated with morbidity, resulting in a mean value for the overall study sample of 10.25 years (95% confidence interval [CI]: 8.86-11.63). As shown in Table 2, the difference in mean PPYL between HD (12.6 years) and APD (6.09 years) was statistically significant. Once we adjusted the estimates for LLPc, the mean cost per patient (€ in 2009) on HD was 6547€ (95% CI: 5727.11-7366.15€), this being the group with the highest mean indirect costs associated with morbidity (Table 2). In the non-parametric analysis of sensitivity (bootstrapping method) of the differences in LLPc for 2009, APD and TX presented lower economic costs in at least 95% of cases than HD (Table 3 and Figure 1).
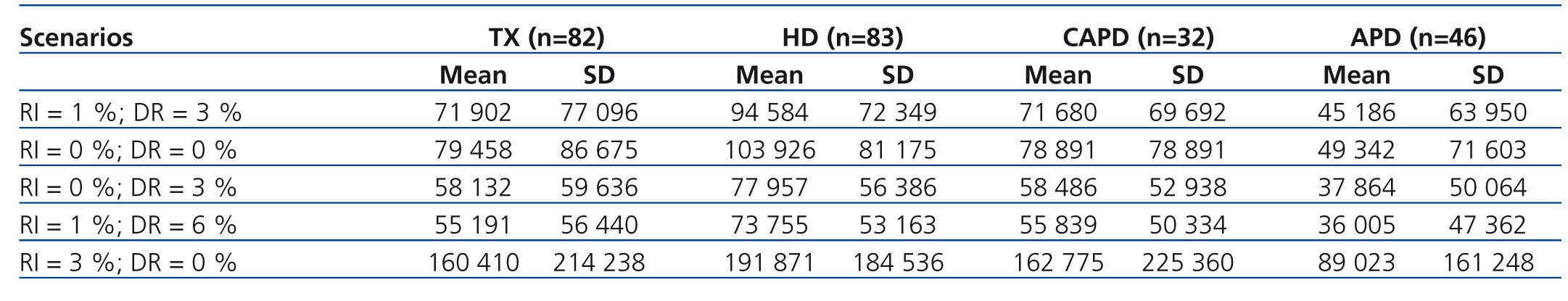
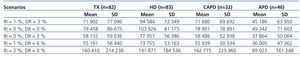
Based on employment status, we calculated the estimated loss in productivity until reaching retirement age (defined as 65 years) for each patient. Table 4 summarises the mean values (and standard deviations) of these potential losses per patient until retirement (total LLPc). Again, HD was the modality that implied the greatest mean loss per patient, with a significant difference when compared with APD (P<.001). This table also shows the mean values for each scenario based on different rates of future discounts and potential increases in income that these patients would experience until reaching retirement age.
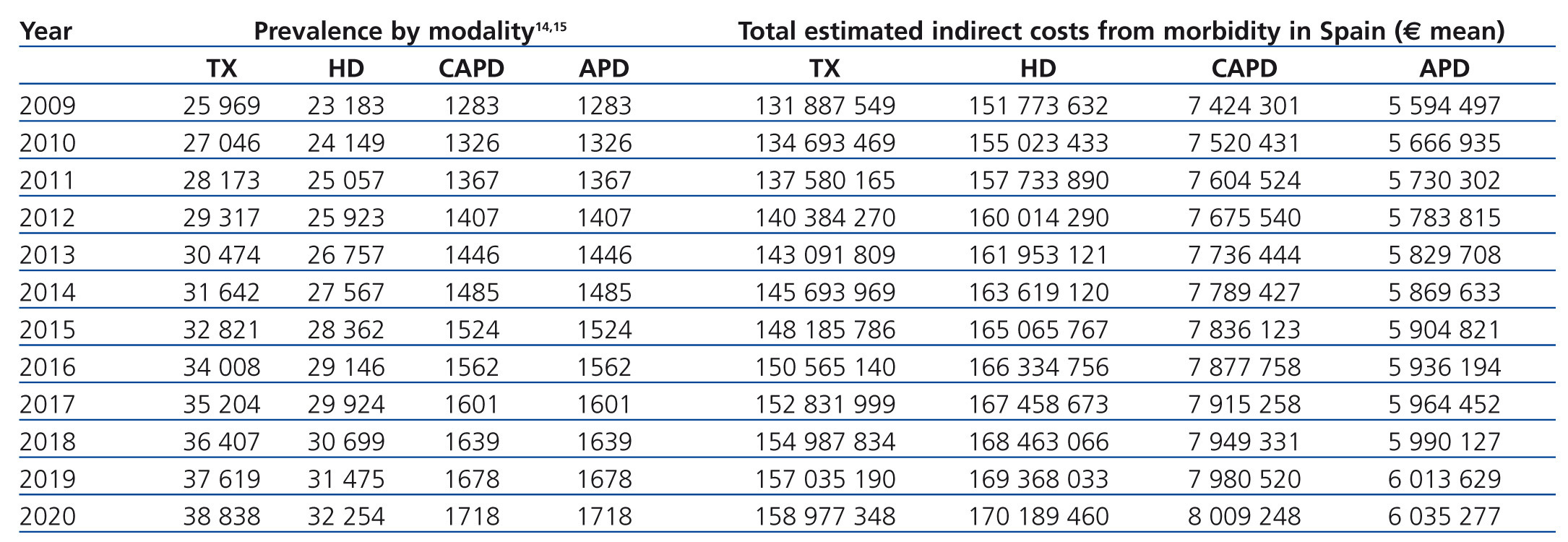
Finally, we estimated the disease-associated costs for each of the different treatment options in future years, correlating the results from indirect costs per patient with the recently published progression models for advanced chronic kidney disease in Spain.14,15 In this analysis, we observed that although the number of prevalent patients on HD was lower than the number of transplanted patients in 2009, the total indirect cost associated with morbidity in these patients was clearly greater (approximately 20 million Euros, Table 5).
DISCUSSION
Currently, there is little doubt regarding the complex and significant social health costs of the most advanced stages of CKD.27,28 In response, the S.E.N., along with the Spanish Society of Family and Community Medicine, has made it a priority in recent years to promote a series of measures designed to detect and prevent (both primary and secondary prevention) chronic kidney disease in order to reduce the associated morbidity and mortality rates.29 In order to present feasible and reasonable management strategies, we must gain a detailed understanding of the resources consumed by this disease in order to quantify and evaluate the potential benefits obtained through the use of different strategies. Without a doubt, these analyses of economic costs can aid health care managers in making optimal (and rational) decisions.16,17 To this end, our study provides information regarding the social costs associated with morbidity in the group of patients with CKD who require RRT and who, let us not forget, present the greatest level of risk and consume the greatest quantity of health care resources despite representing a relatively small proportion of patients.4 Although this analysis certainly covers only one single aspect of the personal and social consequences that this disease implies, it has allowed us to observe from this point of view that CKD implies an important loss in employment productivity. We have shown that the percentage of patients receiving RRT with gainful employment is significantly lower (at 33.3%) than that of the overall Spanish population for the same year (60.62%), although the rate is similar to that of individuals with physical disabilities (31.1%) and those with gastrointestinal, metabolic, and endocrine diseases (32.5%). In addition, we have also demonstrated the existence of differences between the different modalities of dialysis in terms of gainful employment: patients on TX, those with a APD, and, to a lesser degree, those on CAPD, present a greater proportion of employed individuals (39.0%, 47.8%, and 28.1%, respectively) than patients on HD (21.7%). Julian-Mauro et al.18 showed that these differences between PD and HD are consistent even when controlling for variables that are closely related to employment status, such as patient sex, age, and time of treatment. These differences in employment rates based on modality of RRT used are similar to those published in nearby countries.19-21,30-33 However, we must point out that, due to the cross-sectional nature of our study, we were not able to detect whether PD modalities favour the ability of patients to remain employed, or whether it is actively employed patients who prefer these dialysis options due to the greater degree of autonomy they provide.19,21,33 This relationship between a greater personal autonomy, the patient’s physical well-being, and maintaining gainful employment has been well documented,19,20 leading to the reasonable conclusion that those dialysis strategies which facilitate these circumstances (whether APD, CAPD, or home HD) would imply a reduced loss in productivity.
The first conclusion from our calculation of the indirect costs derived from loss in productivity was that CKD in general implies substantial indirect costs from morbidity (approximately 5537€ in 2009 per person/year of working age, assuming a 35.8% activity rate). We also observed a marked difference between different treatment strategies in terms of the indirect costs incurred. While the mean annual loss in labour productivity in 2009 was 6547€ for patients on HD, patients with TX or who were on APD incurred significantly lower indirect costs (5079€ and 4360€, respectively). Patients on CAPD also had lower mean indirect costs than those on HD in terms of lost labour productivity (5785€), although this difference was not statistically significant. Our non-parametric sensitivity analysis confirmed the consistency of the differences observed between patients on HD and those on APD and with TX.
We also observed notable differences between HD and other modalities of dialysis in terms of mean cost per patient in the form of lost labour productivity extrapolated from 2009 until retirement age: an additional loss of between 18,565€ and 38,408€ as compared to TX, between 37,750€ and 102,848€ as compared to APD, and between 17,917€ and 38,783€ as compared to CAPD. Taking into account the recently published progression model for advanced kidney disease in Spain,14,15 the total indirect cost associated with morbidity for patients on HD in Spain was almost 20 million Euros greater than for TX, although the number of prevalent patients on HD was lower, or at least similar (23,183 patients on HD vs. 25,969 patients with TX). These markedly different results in terms of lost labour productivity could be explained by the percentage of patients of working age being treated using each different modality of RRT (21.7% on HD vs. 39% with TX, 47.8% on APD, and 28.1% on CAPD) and the total number of PPYL if working status in 2009 were to be maintained (12.58 years [95% CI: 10.42-14.73 years] on HD vs. 10.05 years [95% CI: 7.45-12.65 years] with TX, 6.09 years [95% CI: 3.43-8.74 years] on APD, and 10.69 years [95% CI: 6.14-15.23 years] on CAPD). In consequence, it would appear that, from a social perspective, favouring treatment strategies that facilitate patient autonomy on RRT would minimise the impacts of the indirect costs associated with morbidity. In addition, this superior productivity could be indicative of improved social and individual well-being of these patients.19
Although this economic cost of CKD could be quantified more intuitively using other metrics, such as by calculating disability payments or other compensations that the State must provide for these patients, we preferred not to include them due to conceptual and methodological reasons. Even so, using the information compiled in our study, we also estimated these costs (mean per patient/year 2009), and the resources directed towards covering these costs, as can be imagined, were greater for HD (7247€; 95% CI: 5884-86009€) than for TX (5740€; 95% CI: 4352-7128€), APD (5861€; 95% CI: 4007-7715€) or CAPD (6413€; 95% CI: 4122-8706€). Again, these results can and should be used by public administrators to promote preventative strategies in patients in initial stages of CKD and to facilitate personal autonomy when RRT becomes a necessity.
In terms of limitations to our study that may have influenced the results, we must point out that the proportion of male patients was greatest in the APD group. This could be of importance since the rate of employment was greater in males than in females (40.1% vs. 22.9%). Even so, we did not observe significant differences between the different treatment types in terms of sex distribution, as occurred in the cross-sectional study by Helanterä et al. in 2012.33 In addition, the sex ratios for our patients were similar to those published in regional registries.34-36 We also failed to detect statistically significant differences in terms of age or years of treatment between HD and APD or TX groups (although patients on CAPD had fewer total years on treatment), and in the case of APD, employment rates were clearly different from HD patients in a multivariate analysis carried out in a prior analysis.18
On the other hand, we did not register loss of employment due to temporary disability, and so we were unable to assess the magnitude of this factor. In this case, we assumed that patients who worked and received a salary did not lose productivity due to their disease. It would have been preferable to carry out a specific analysis of changes in employment due to disease that could take into account the type of employment before treatment in comparison with employment situation in 2009. Since we ignored these possible changes, we made the decision not to assume any change, although this could have led to an under-estimation of these indirect costs. Despite these limitations, the results of our study are in accordance with other recently published studies from Spain,15 which indicate that HD is the least preferable modality of dialysis from the point of view of indirect costs associated with morbidity (8025€ vs. 6911 on APD and CAPD and 5359€ with a TX, 2010). In addition, the greater proportion of patients on PD that are employed is also reflected in other recent publications.20,21
To conclude, we have provided information regarding the magnitude of the social consequences of CKD and the relevant differences in terms of lost employment productivity based on type of RRT. This information provides a new argument in favour of maximising the use of dialysis modalities that facilitate the greatest possible patient autonomy, and thus a greater freedom and flexibility for developing the patient’s private and professional life. While previous studies reported a greater degree of satisfaction on the part of patients on PD as compared to those on HD, because of the decreased perceived disruption of daily activities,37,38 our results show tangible consequences of optimising the autonomy of patients on dialysis in terms of reducing the social cost of the disease in addition to differences in mortality rates. Thus, far from considering the different modalities of RRT as isolated components of a patient’s life, treatment planning must consider the patient as a whole, taking into account the greatest number of options possible at each stage based on the patient’s state of health, with a view towards the long-term results in maximising patient quality of life and efficiency of the intervention (in terms of the patient and society as a whole). In order to make an informed and objective decision, active patients must be familiarised with home dialysis modalities, which, in addition to being advantageous in terms of costs, produce excellent clinical results while allowing patients to maintain their normal lifestyle and activities, professional and otherwise, to the greatest extent possible. With this in mind, from the point of view of the health care authorities, these home dialysis alternatives could be considered as the initial dialysis treatment option of choice (except for those patients eligible for an early transplant), whereas modalities administered in dialysis centres would be reserved for later, when the patient has lost autonomy or increased in clinical complexity. Finally, ALCER recommends that patients continue with their professional activity whenever possible (whether by self-employment, private, public, etc.), since enough evidence exists to establish the physical, psychological, and socioeconomic patient benefits, in addition to maintaining a sustainable social health care system, as reflected in this study.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Description of the personal situation of each patient interviewed in 2009 and their corresponding number of potentially productive years of life lost
Table 2. Description of the sample based on modality of renal replacement therapy administered
Table 3. Non-parametric sensitivity analysis of the difference between different dialysis modalities in the mean indirect costs per patient (year: 2009); bootstrap method with 1000 repeats
Table 4. Total cost from the loss in employment productivity considering different rates: increased worker income and discounts
Table 5. National annual indirect costs due to morbidity associated with the different possible alternatives for renal replacement therapy
Figure 1. Cost of lost labour productivity in 2009